On 11 January 2021, while on-call with my colleague Tomaz, the intensive care unit (ICU) was rather quiet. I woke at 6:30, travelled to my office, turned on my computer and started to delete junk mail. I wiped my nose and suddenly experienced a strange feeling in my head, and my right hand felt like it did not belong to me. I sat down thinking I must be suffering from orthostatic hypotension because I am typically dehydrated when working. However, it did not get any better and, when I tried to say something to my secretary, I realised that I was uttering strange and meaningless words. At that moment I noticed a text message from my wife Anita and, while trying to answer, I had to correct three simple words several times because of misspelling. I made another effort to phone my colleague Peter and somehow managed to say “please come”. I started to think about my future, as by this time a diagnosis of evolving stroke with motor dysphasia was quite obvious. I realised that I would have to give up my clinical work which I loved, I would not be able to lecture anymore, to write papers…. Wow, what a nightmare! When Peter arrived, I tried to tell him my diagnosis, but I could not. I just put my hand on the frontotemporal region of my head and he realised immediately what was going on.
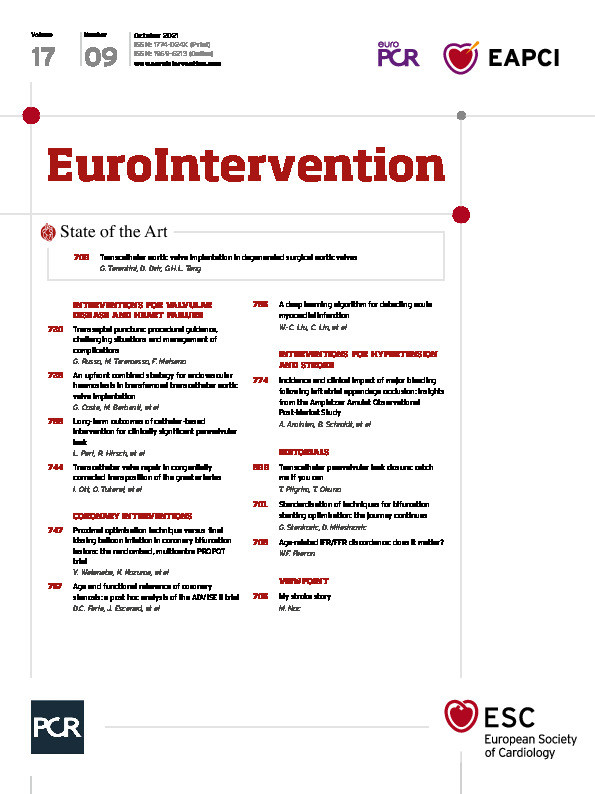
We walked together to our department, and he ordered an emergency computed tomography (CT) scan, arterial pressure measurement and basic laboratory panel. I saw the pale face of our nurse Goga who was mute with fear. I did not want to be transported to the CT unit and insisted on walking with Peter without speaking because I knew something strange would come out if I tried. Whilst in the CT scanner, I was thinking about glioblastoma. I remembered some of my patients in whom unexpected stroke revealed this terrible diagnosis. At the end of the examination, I managed to say something like “tumour” and Peter responded “no”, but he mentioned acute vessel occlusion with significant penumbra (Figure 1A). I wanted to walk back from the CT unit to our ICU but this time Peter insisted on transporting me in a wheelchair. I gave in but tried to avoid any eye contact with people coming to work. For the first time in my life, I was very sick and dependent. In the ICU, I was allocated the same bed which had been occupied 20 years earlier by my father while he had a large anterior myocardial infarction. He had been treated with one of the first primary percutaneous coronary interventions (PCI) in Slovenia. It was also the same bed occupied by my mother-in-law, in whom I had diagnosed and stented critical left main eight years previously. This bed, so far a very lucky bed for our family, was now mine…
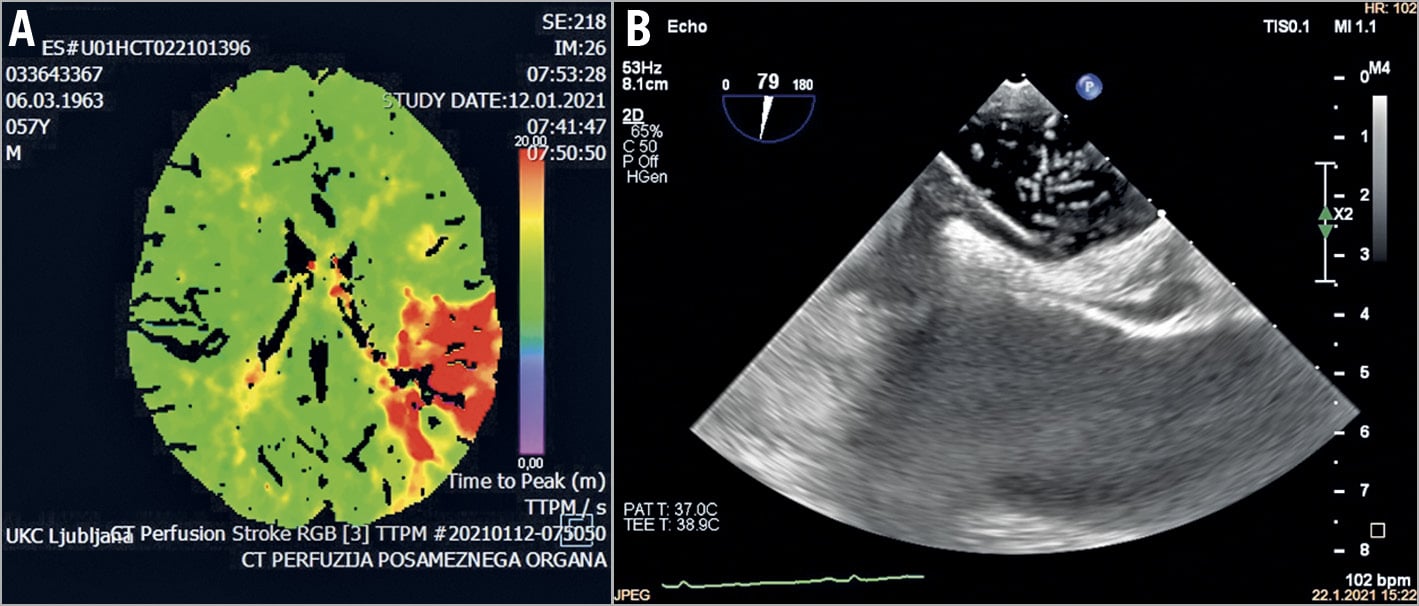
Figure 1. Computed tomography perfusion scan showing a large (8.5 cm) penumbra (in red) located in the left frontal-parietal region (A) and transoesophageal echocardiography showing a large patent foramen ovale with contrast bubbles crossing from the right to the left atria (B).
I heard Peter calling Anita and I knew she would come immediately. I wanted to see her but, on the other hand, I did not want her to find me in such a poor condition. I closed my eyes and lost all sense of time. Suddenly she was there. I was so happy and tried to say something, but not very successfully.
Peter came again and informed me that the stroke team had decided on immediate thrombectomy. They grabbed my bed, rushed me to the elevator and along underground corridors towards the interventional neurology department. During the transportation I noticed that my speech was suddenly improving and remember asking Peter to skip intubation as this would only delay reperfusion. I just wanted my cerebral artery to be opened as soon as possible! I knew so well that time is even more crucial for an ischaemic brain than for an ischaemic myocardium, as this had been my mantra for the last 20 years of my professional life. While my speech was constantly improving, I realised that I had probably spontaneously reperfused.
I remember seeing Fajko, the chief of vascular neurology, with his co-workers, worried but ready to go. I told Fajko that I had probably spontaneously reperfused because my speech had improved dramatically. He agreed and decided that magnetic resonance imaging (MRI) was to be performed. It took forever. My eyes were closed and again I was thinking about a possible brain tumour not seen on the CT scan. Finally, they got me out of the MRI scanner and confirmed a lack of residual ischaemia and no need for thrombectomy – great news!
When I was lying in the bed in a stroke unit, I felt my crashed “brain computer” gradually restarting. I spoke to my co-workers Peter and Misa who visited me a few hours later with best wishes from the rest of our team. Later in the afternoon, I tested myself in writing text messages on my phone. All went well. When everybody left, I tested myself in English, both speaking and writing – that went well too. Even my German was not any worse than before. I started to phone friends who were worried telling them that I was fine. Indeed, I felt like checking my restarted brain computer for lost files… and fortunately all were there. Later in the evening I carefully observed some of my friends visiting me to see if they showed any “signs of mercy” indicating lack of my complete recovery. It was not there.
The night was good with no recurrence of symptoms. In the morning, my classmate Sasa, who is a neurologist, came and showed me the CT perfusion and MRI. When I saw the extent and location of the ischaemic brain area before spontaneous reperfusion, I realised that every word I say or write is God’s very generous gift. When my daughter Naomi called, I realised that I might never have spoken to her again if that artery had remained occluded.
Soon, however, I returned from my “emotional excursion” to reality. It was me again, a physician looking for causes and mechanisms of diseases for more than 34 years. Besides, the echo, kindly performed by one of my colleagues, was fine except for atrial septal aneurysm. I never had arterial hypertension, I never smoked, I do not recall any palpitations and my electrocardiogram during the last 24 hours did not record even a single ectopic beat. All my arteries were very smooth on CT/MRI. Then came the transcranial Doppler. The bubbles already at baseline and a real storm during Valsalva manoeuvre indicated significant right to left shunting. Even though I wanted to see my patent foramen ovale (PFO) as soon as possible, I preferred to postpone transoesophageal echo (TOE) for a week.
On the other hand, because of the high likelihood of PFO-related stroke, I decided to postpone my second dose of COVID-19 vaccine for a few months after closure. Even though a potential cause effect relationship between the first vaccination 13 days earlier and stroke was unlikely, my reasoning was that PFO had been there all my life and I have done so many crazy things including Europa Cup downhill competitions, crazy professional plane trips and very frequent on-calls…. but I had never experienced any symptoms indicative of paradoxical embolism. Moreover, there were also no old ischaemic lesions on my MRI. I came up with the interesting hypothesis that the immunological response to vaccination might have created a prothrombotic condition leading to transient deep vein thrombosis and paradoxical embolism, which of course cannot be viewed as an endorsement to avoid the COVID-19 vaccine if PFO is present. On the other hand, I was probably very lucky not to get COVID-19 while working during the pandemic because this infection would probably have created an even more distinct prothrombotic state.
After a few days in the stroke unit, I was discharged on aspirin and clopidogrel. My friend Natasa performed TOE and, as expected, she found a large PFO with septal aneurysm, a prominent Eustachian valve and baseline right to left shunting which significantly increased during Valsalva (Figure 1B). While the benefit of preventive closure in patients without prior stroke/transient ischaemic attack (TIA) is controversial, there was little doubt that my PFO had to be closed1. How ironic, because with Natasa, who has been my echocardiographer for structural interventions from the very beginning, we have closed PFO in 254 patients, and I am the only independent operator in the country. So, I had another problem because I needed someone to come over and close my PFO or I would have to travel abroad. However, because of the second COVID wave, we were facing progressive and unpredictable travel restrictions. Wow, what bad timing…
I was very lucky to have my dear friend Flavio Ribichini in Verona (Italy) three hours away by car. He drove from Verona on the morning of 6 March, my 58th birthday. I received diazepam 5 mg and, when they left me in the cath lab, I was completely dizzy. I hardly remember swallowing the TOE probe, groin shaving, draping, or the femoral puncture. As a matter of fact, I only recall when they asked me for the Valsalva manoeuvre at the end. When I heard the words “no bubbles crossing”, I knew Flavio had done an excellent job. What a birthday present. No more “waiting” for the second stroke. This had been my daily fear, despite taking aspirin and clopidogrel, because I knew very well the randomised trials showing a 45-97% relative risk reduction in stroke recurrence after closure compared to medical therapy only1. Even though the Kaplan-Meier curves initially separated relatively slowly, all the fancy statistics would not matter if I was unlucky and got a second stroke while waiting for closure. I also learned that even a TIA, which I may have banalised too often in the past, is a very important clinical endpoint. Indeed, all these valuable lessons for my future work which I could have learned only as a patient came down to a very simple take-home message – close it as soon as possible to liberate a patient from the daily threat of a second stroke. As a patient I also learned how important it is to be treated by doctors and nurses whom you fully trust. This is especially true for interventional procedures where only a skilled and responsible operator may calm you as a patient, as Flavio did.
Acknowledgements
I would like to thank all my friends and colleagues for their generous support on my way back to normal life, especially Peter Radsel, MD, PhD, who took care of me in the acute phase, Fajko Bajrovic, MD, PhD, who was my neurologist, Natasa Cernic Suligoj, MD, who guided percutaneous PFO closure by TOE, and Flavio Ribichini, MD, PhD, who successfully closed my PFO.
Conflict of interest statement
The author has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.