Abstract
Patients with multiple valve disease are a frequent and heterogeneous entity whose evaluation and management are challenging. The assessment of the severity requires a cautious integrative evaluation. The indications for intervention are based on global assessment of the consequences of the disease, mainly based on symptoms, pulmonary hypertension, and left ventricular dysfunction. The decision to intervene should also take into account the inherent additional risk. Percutaneous intervention in this population is in its infancy but the future development of transcatheter techniques will be of interest in this high-risk cohort and will offer the possibility of tailored and staged procedures.
Introduction
Patients with multiple valve disease (MVD) are a heterogeneous group for which specific data are limited1. Therefore there are few evidence-based recommendations.
In the Euro Heart survey on valvular heart disease2, patients with MVD represented one fifth of the total study population. Rheumatic heart disease was the most frequent aetiology followed by degenerative valve disease. The frequency of comorbidities was close to that observed in patients with single-valve disease but patients tended to present with more serious symptoms.
In patients with MVD, besides the separate assessment of each valve lesion, it is necessary to take into account the interaction between the different lesions. As an example, mitral regurgitation (MR) may lead to an underestimation of the severity of aortic stenosis (AS), since a decrease in stroke volume results in low-flow low-gradient AS. On the other hand, the severity of MR may be overestimated in the presence of high left ventricular pressures induced by AS. Similarly, it might be more difficult to assess the severity of AS in patients with severe mitral stenosis (MS). These important haemodynamic interactions underline the need for cautious integrative evaluation3.
The indications for intervention are based on global assessment of the consequences of MVD: symptoms, pulmonary hypertension, and left ventricular dysfunction. The decision to intervene on multiple valves should also take into account the inherent additional risk of mortality and morbidity.
Surgical intervention
With regard to valve surgery, the choice of indication, strategy and technique will take into account the presence of other valve disease. Recommendations for the management of the most frequent clinical scenarios are as follows:
– When MR is associated with severe AS, surgical intervention on the mitral valve is necessary in patients with severe primary MR. On the other hand, secondary MR (especially if less than severe) usually improves after the aortic valve is treated. It should also be remembered that additional mitral valve surgery markedly increases the risk of surgery, particularly in the elderly with significant mitral annular calcification.
– In patients who undergo mitral valve surgery and have concomitant moderate aortic valve disease, the decision to treat the aortic valve will be based on the aetiology of the aortic disease, age, presence of LV dysfunction and the likelihood of mitral valve repair.
– Moderate to severe tricuspid regurgitation (TR) untreated at the time of surgery for severe MR is associated with poor clinical outcome. Thus, combined tricuspid surgery is indicated in patients with mitral valve disease requiring surgery and associated severe primary or secondary TR. Surgery should also be considered in patients with moderate primary TR as well as in patients with mild to moderate secondary TR with a dilated annulus (>40 mm or >21 mm/m2)3.
Percutaneous intervention
As regards percutaneous valve intervention the strategy could be as follows:
– The prevalence of moderate or severe MR in patients who undergo transcatheter aortic valve implantation (TAVI) for severe AS ranges between 19% and 30%4. The presence of moderate or severe MR was reported to carry a higher mortality risk at 30 days although patients with MR also have a significantly higher risk profile. Most patients with severe MR experienced functional improvement one year after TAVI (49% improved by at least one NYHA class, 16% remained unchanged4). Prediction of improvement in MR after TAVI remains challenging – a baseline aortic mean gradient <40 mmHg and the presence of primary MR, pulmonary hypertension or atrial fibrillation have been shown to be predictors of a lack of improvement in MR4. However, these data are limited by the lack of differentiation between primary and secondary MR in most series and the short duration of follow-up.
– Very limited evidence on the combined use of TAVI and MitraClip5 (Abbott Vascular, Santa Clara, CA, USA) suggests that this combination of procedures is feasible but clinical efficacy remains unproven. Such a strategy should be limited to highly selected cases. A combined (usually staged) procedure may be applicable, in patients with severe primary MR accessible to MitraClip treatment in whom TAVI has already been successful. In patients with severe secondary MR, it is probably better to wait a few months after TAVI and undertake MitraClip treatment only if MR does not decrease and symptoms persist.
– The management of associated mitral stenosis (MS) is very challenging since MS in such cases is usually degenerative and not suitable for percutaneous mitral commissurotomy (PMC). Furthermore, the severity of MS is difficult to assess. Mitral intervention should only be undertaken when the degree of mitral obstruction remains severe after TAVI. Limited preliminary reports suggest that transcatheter mitral valve implantation is feasible, usually sometime after TAVI6. These patients generally have extensive calcification of the mitral annulus (Figure 1), and there is a significant risk of residual left ventricular outflow tract obstruction in patients with a small left ventricular cavity and/or septal hypertrophy and/or narrow aortomitral angle.
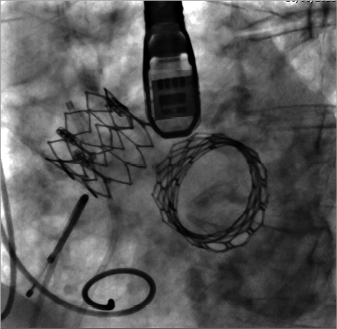
Figure 1. Double transcatheter valve implantation.
Transcatheter aortic valve implantation (Edwards SAPIEN XT; Edwards Lifesciences, Irvine, CA, USA) was performed in 2011 in an 81-year-old woman for severe aortic stenosis followed by transcatheter mitral valve implantation (Edwards SAPIEN 3; Edwards Lifesciences) in 2015 for severe mitral stenosis and massive annular calcification.
– In patients with MR and concomitant moderate to severe TR, MitraClip treatment leads to improvement in TR and functional NYHA class in most patients. However, severe TR is a predictor of poor outcome with higher incidence of death and rehospitalisation for heart failure at 12 months7. In the future, it is expected that percutaneous tricuspid repair techniques could be used in combination with transcatheter mitral valve repair in a manner reflecting current surgical strategy.
– In patients with severe MS and moderate aortic valve disease, PMC can be performed as a means of postponing the need for surgical treatment of both valves.
– In cases of severe MS and severe TR, PMC can be attempted in patients with sinus rhythm, moderate atrial enlargement and functional TR secondary to pulmonary hypertension. Surgery on both valves may be preferred in other scenarios3.
– In the very rare instance of combined severe isolated tricuspid stenosis and/or MS/AS of rheumatic origin (which may arise in countries where rheumatic valve disease is frequent), multiple balloon commisurotomy can be performed.
Conclusions
Patients with MVD are a frequent and important entity whose evaluation and management are challenging. Today, percutaneous intervention in patients with MVD is in its infancy but the future development of transcatheter techniques will doubtless be of interest in this high-risk cohort and offer the possibility of tailored and staged procedures.
Conflict of interest statement
A. Vahanian is a consultant for Medtronic, Valtech and Abbott and is on the speakers bureau for Edwards Lifesciences. E. Brochet has received speaker fees from Abbott Vascular. D. Himbert is a consultant and proctor for Edwards Lifesciences and Medtronic.

