Following the first aortic and mitral valve replacement procedures performed in the 1950s, valve disease has historically been treated surgically. However, many studies identified patients who were deemed too high risk for surgery and were denied a definitive therapy. For symptomatic severe aortic stenosis (AS), the introduction of transcatheter aortic valve implantation (TAVI) changed the prognosis of these patients significantly; the PARTNER trial showed that TAVI improved survival by a dramatic 20% at one-year follow-up1. In patients deemed very high risk, TAVI was non-inferior to surgical aortic valve replacement (AVR)2.
The complexity of the aortic valve anatomy and the aetiology of degenerative AS are limited; surgical AVR is a relatively straightforward procedure in which the native valve is replaced by a prosthetic valve. Moreover, much of the enthusiasm associated with TAVI is generated by the self-evident principle of the procedure. This is underlined by the fact that current transcatheter aortic valves on the market are designed using the same principle: a transcatheter valve is placed inside the native valve.
Global enthusiasm and the advent of new devices set the stage for exploring TAVI in lower-risk patients and ongoing trials are including patients at intermediate risk. Indeed, risk assessment is complicated but the most important factors affecting prognosis are age and comorbidities3,4.
Transcatheter valve interventions for mitral valve disease have been available for several decades but have not been adopted as much as TAVI procedures, even though many patients with severe mitral regurgitation (MR) eligible for treatment are denied surgery (Figure 1A, Figure 1B)5. In the current issue of EuroIntervention, Andalib and co-authors present a systematic review and meta-analysis of mitral valve surgery for MR with the goal of showing that high-risk patients may be more suitable for transcatheter than surgical mitral valve intervention6. Indeed, transcatheter mitral valve interventions (TMVI) are currently most often performed in patients not suitable for surgery because of a too high procedural risk7-9. This is supported by recommendations in the 2012 ESC/EACTS valvular guidelines10.
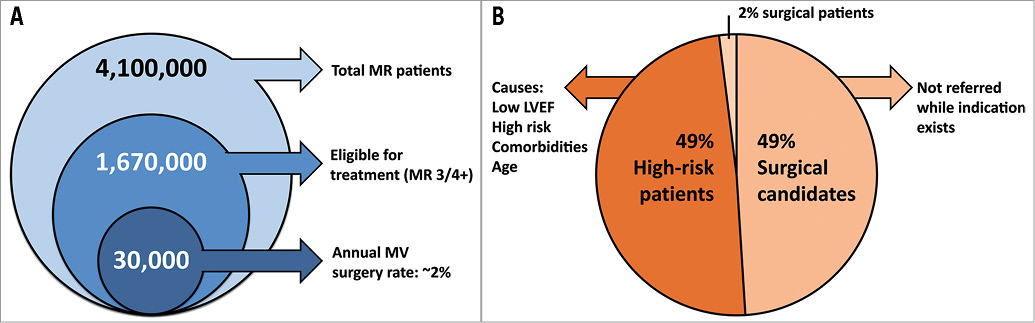
Figure 1. Patient population (A) and treatment evaluation (B) for mitral regurgitation. Data for (A) are derived from the United States in 2009. Data for (B) are approximations derived from the literature.
From their review and analysis of 16 studies comprising 5,747 octogenarian patients, the authors conclude that operative mortality after mitral valve surgery is high, long-term survival is poor and the quality of life benefit is uncertain. They state that TMVI may be an alternative in high-risk patients6. Among the questions which arise from this analysis is whether octogenarians truly represent a high-risk population in whom TMVI should be considered, and whether this is the correct identifier of a population suitable for TMVI. In the German TRAMI registry which included 1,064 patients who underwent the MitraClip procedure, advanced age appeared to be the strongest factor for denying surgery11. Indeed, age contributes significantly to the predictive operative risk of mortality and therefore many elderly patients are at high risk. However, risk assessment based on age alone, or exclusively on operative risk of mortality, is too arbitrary4. Many patients with MR have left ventricular dysfunction (LVD) and there are no data to support the view that mitral valve surgery in elderly patients with LVD improves prognosis; it is therefore often denied to these patients (Figure 1B). It may seem that age per se is used to deem patients unsuitable for surgery, while there is actually a lack of proven benefit in elderly patients with LVD. It is unlikely that TMVI in these patients will improve prognosis.
In addition, categorisation of MR into a degenerative (primary) and a functional (secondary) aetiology is crucial as is the severity of disease, since it significantly affects outcomes and determines the optimal treatment strategy for individual patients: mitral valve repair or replacement with or without concomitant coronary artery bypass grafting, tricuspid annuloplasty, or atrial fibrillation ablation. In the studies included by Andalib and co-authors, this case mix is pooled and many of these patients would not be candidates for TMVI because of the concomitant procedures that are required to provide an optimal result. Moreover, the complexity of these patients resulted in a pooled 30-day mortality of 7% after mitral valve repair and 13% after mitral valve replacement. These rates cannot reliably be used to compare with TMVI; in the EVEREST II trial which compared mitral valve surgery with repair using the MitraClip for patients with an indication for isolated mitral valve surgery, rates of death at 30 days were only 2% and 1%, respectively12.
The anatomy of the mitral valve is complex. Even in cases of degenerative mitral valve regurgitation without an indication for concomitant procedures, the severity and complexity of regurgitation to a large extent determines the feasibility of mitral valve repair as opposed to replacement (e.g., involvement of the anterior and posterior leaflets, papillary muscles, and chords). Although many studies have suggested that mitral valve repair is superior to replacement, randomised clinical trials remain absent. The current literature is limited by selection bias, with repair being performed in less complex cases. Moreover, the success of repair is highly dependent on surgical experience, and the good outcomes with repair are often from selective practices of high-volume, specialised centres. In contrast, outcomes of surgical repair in the EVEREST II trial were more modest with 20% of patients having recurrence of 3+/4+ MR at one year12. The conclusion from Andalib and co-authors that repair is superior to replacement should therefore be interpreted with caution. In addition, it may be somewhat premature to indicate transcatheter mitral valve repair in high-risk patients. It remains debatable whether repair is better than replacement, which in this heterogeneous patient population is strongly dependent on the aetiology of MR and a number of patient- and surgeon-related factors. The heterogeneity in the design of TMVI devices indicates that it remains unclear how best to repair MR through a transcatheter approach13. There will be patients in whom repair is not feasible because of the complexity of their disease. In these patients it will be interesting to see how current developments of transcatheter mitral valve implantation may affect implementation of TMVI as the complexity of the anatomy and aetiology will be less crucial in these patients. Indications for TMVI will then more and more resemble TAVI, but at present it may be too simplistic to copy indications from TAVI based on age and/or preoperative risk of mortality alone.
Conflict of interest statement
The authors have no conflicts of interest to declare.

