Abstract
Aims: The aim of this study was to demonstrate the feasibility and safety of ST-elevation myocardial infarction (STEMI) management in young patients by limiting implantation of durable intracoronary devices (using a bioresorbable stent or medical treatment alone).
Methods and results: Patients <50 years old admitted for STEMI with single-vessel disease received a two-stage management strategy. During a second coronary angiography performed between day 2 and day 7, optical frequency domain imaging (OFDI) guided the decision on therapeutic management, i.e., i) in the case of a stenosis greater than 70% or plaque prolapse, implantation of a BVS; or ii) in the other cases, continuation of medical management alone without stenting. All patients underwent systematic angiographic control with OFDI imaging at six months. Among the 653 patients admitted for STEMI, 124 patients were under 50 years old and 45 patients were included. Early management was performed on average at day 3.9 (day 2 - day 7). Thirty-four (34) patients received BVS implantation and 11 were treated medically. Only one major adverse cardiac event (MACE) had occurred at six months.
Conclusions: In a selected younger population, the management of STEMI guided by OFDI and based on the concept of limiting implantation of durable intracoronary devices appears to be a feasible and safe therapeutic option.
Abbreviations
ACS: acute coronary syndrome
BVS: bioresorbable vascular scaffold
CPK: creatine phosphokinase
DES: drug-eluting stent
ECG: electrocardiogram
LAD: left anterior descending artery
MACE: major adverse cardiac event(s)
MLA: minimal lumen area
OFDI: optical frequency domain imaging
QCA: quantitative coronary angiography
STEMI: ST-segment elevation myocardial infarction
TIMI: Thrombolysis In Myocardial Infarction
Introduction
Stenting in the acute phase of myocardial infarction exposes the patient to complications related to the presence of a thrombotic component (microvascular embolisation and the risk of stent malapposition potentially favouring the occurrence of late stent thrombosis). Certain medical teams have developed two-stage strategies with consideration given to deferred stent implantation in order to limit these complications1. Furthermore, it is possible at times to consider the continuation of medical treatment alone without stenting2.
When stenting is performed, long-term tolerance of a metallic structure within a coronary artery in terms of vasomotion and endothelial function is an issue. New bioresorbable scaffolds could potentially restore the vasomotor properties of arteries and their endothelial functions3 and avoid stent malapposition after resorption. Young patients may be a preferential target for these new devices. Indeed, young patients admitted for STEMI often have simple coronary lesions with an important thrombotic component4.
In the light of the above, we developed a specific management scheme dedicated to the young patient admitted for STEMI.
Methods
ELIGIBLE PATIENTS
INCLUSION CRITERIA
STEMI within the first 12 hours after the onset of symptoms
Age <50 years
A single coronary lesion on initial angiogram
Written consent obtained
EXCLUSION CRITERIA
Cardiogenic shock on admission (SBP <80 mmHg)
Angiographic exclusion criteria:
Multivessel lesions
Target lesion in left main trunk
Target vessel diameter >4.2 mm
Target lesion involving a bifurcation (side branch diameter >2 mm)
Moderate or heavy calcifications on target vessel
Pregnancy
INITIAL MANAGEMENT STRATEGY (Figure 1)
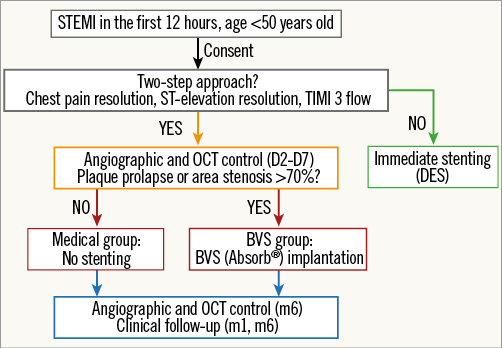
Figure 1. Management algorithm.
The aim of the initial strategy was to achieve optimal reperfusion by the restoration of a Thrombolysis In Myocardial Infarction (TIMI) flow ≥2, associated with pain reduction. In the absence of optimal epicardial reperfusion, a metallic drug-eluting stent (DES) was implanted. In the case of optimal epicardial reperfusion, the therapeutic decision was based on a second angiography performed between day 2 and day 7 (delay time at the discretion of the operator). The exam was completed by performing optical frequency domain imaging (OFDI): in the absence of plaque prolapse (defined by: (i) an appearance of a mobile plaque in continuity with the coronary wall with (ii) evidence of plaque prolapse into the lumen, and (iii) a maximal plaque length exceeding one third of the arterial diameter) or a stenosis of less than 70% of the reference area, the continuation of medical treatment alone without stenting was retained (MED group). Conversely, the patient underwent BVS implantation (BVS group).
CONTROL ANGIOGRAPHY AND OFDI AT SIX MONTHS
All patients underwent systematic control angiography with OFDI at six months.
MATERIAL
OPTICAL FREQUENCY DOMAIN IMAGING
The images were acquired on a Terumo OFDI system (Lunawave®, FastView®; Terumo Europe, Leuven, Belgium).
Automatic pullback of the catheter (20 mm/s) was contemporaneous to an intracoronary injection of an iodixanol contrast agent.
BIORESORBABLE STENT
The implanted bioresorbable stent was the Absorb® GT1 bioresorbable vascular scaffold (Abbott Vascular, Santa Clara, CA, USA).
ANGIOGRAPHIC ANALYSES
Based on the initial angiography, the following criteria were determined: initial TIMI flow grade, stenosis by QCA (%), reference artery diameter (mm), lesion length (mm) and thrombus grade quantified by the Gibson score5. In case of arterial occlusion, lesion length and the degree of stenosis by QCA were determined after restoration of a flow.
OFDI ANALYSIS
OFDI analysis was based on the presence of thrombus, its quantification (thrombotic score6), the reference luminal area in mm2 (mean between upstream and downstream reference areas), and the minimal luminal area (MLA) in mm2. In the case of stenting, minimal stent area in mm2, edge dissection, stent malapposition and stent strut coverage were determined.
CLINICAL FOLLOW-UP
Patient follow-up consisted of the monitoring of major adverse cardiac events (MACE), defined as death, recurrent myocardial infarction, and stent thrombosis at six months.
ETHICS
The study was performed according to the provisions of the Declaration of Helsinki and good clinical practice, and was approved by the local ethics committee.
STATISTICAL ANALYSIS
Statistical analyses were performed using Stata software, version 13 (StataCorp, College Station, TX, USA). The tests were two-sided with an α=0.05. Patient characteristics are described for each group as mean±standard deviation or median and interquartile range for continuous variables, according to statistical distribution, and as the number of patients (%) for categorical variables. Comparisons between independent groups (MED vs. BVS groups) with regard to baseline patient characteristics were performed using chi-square or Fisher’s exact tests for categorical variables and using a Student’s t-test or non-parametric Mann-Whitney test if assumptions of the t-test were not met for quantitative parameters. Since this study was a proof of concept study evaluating feasibility and safety, the estimated number of subjects required was obtained using a multi-step Fleming design. Taking into account recruitment capacities, the feasibility objective for this study and literature data, we decided to consider a one-step process with a lower limit for maximum non-feasibility set at 80% and an upper limit for minimum feasibility at 95%. For a type I error at less than 5% and a statistical power (1-β) greater than 90%, it was necessary to recruit 45 patients. If there were 41 or more patients without MACE, the study could conclude as feasible.
Results
STUDY POPULATION (Table 1)
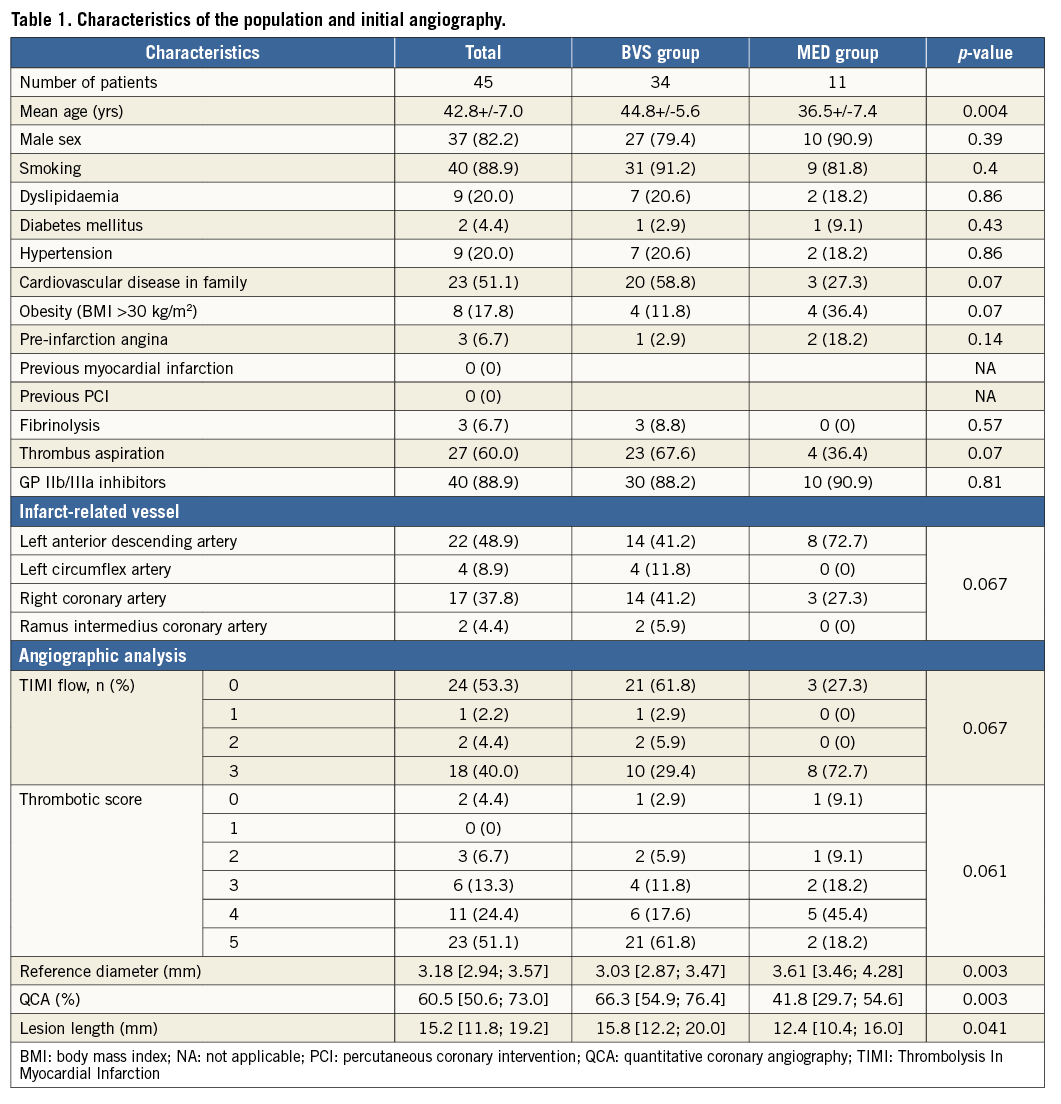
Among the 653 patients admitted to our centre for STEMI between April 2013 and April 2015, 124 patients were under 50 years of age. Sixty-five had a single coronary artery lesion. Finally, forty-five consecutive patients were included in the study (Figure 2).
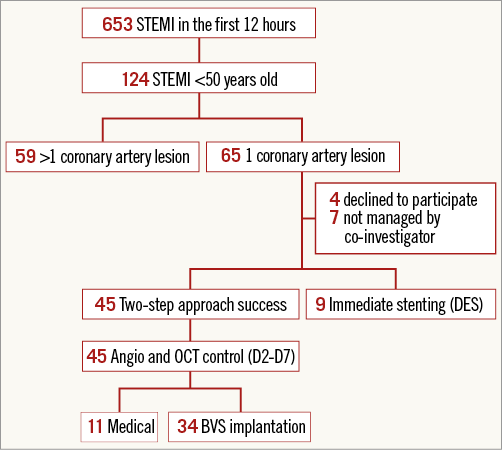
Figure 2. Flow chart.
The majority of patients were male (82.2%), with a median age of 42.8 years (±7 years). Most patients were smokers, i.e., 88.9% of cases (34 active and six ex-smokers). Three patients received prehospital fibrinolysis (6.7%) with a delay of 2.5±0.86 hours.
Glycoprotein (GP) IIb/IIIa inhibitors were used in 88.9% of cases and manual thrombus aspiration was performed in 60% of cases.
INITIAL ANGIOGRAPHY RESULTS (Table 1)
The target vessel was the left anterior descending artery (LAD) in almost half of the cases (48.9%). The artery was occluded (TIMI 0) in 53.3% of cases and flowed normally in 40% of cases. The residual stenosis after the initial angiography was 60.5% on QCA.
EARLY CONTROL RESULTS AND THERAPEUTIC STRATEGY (Table 2)
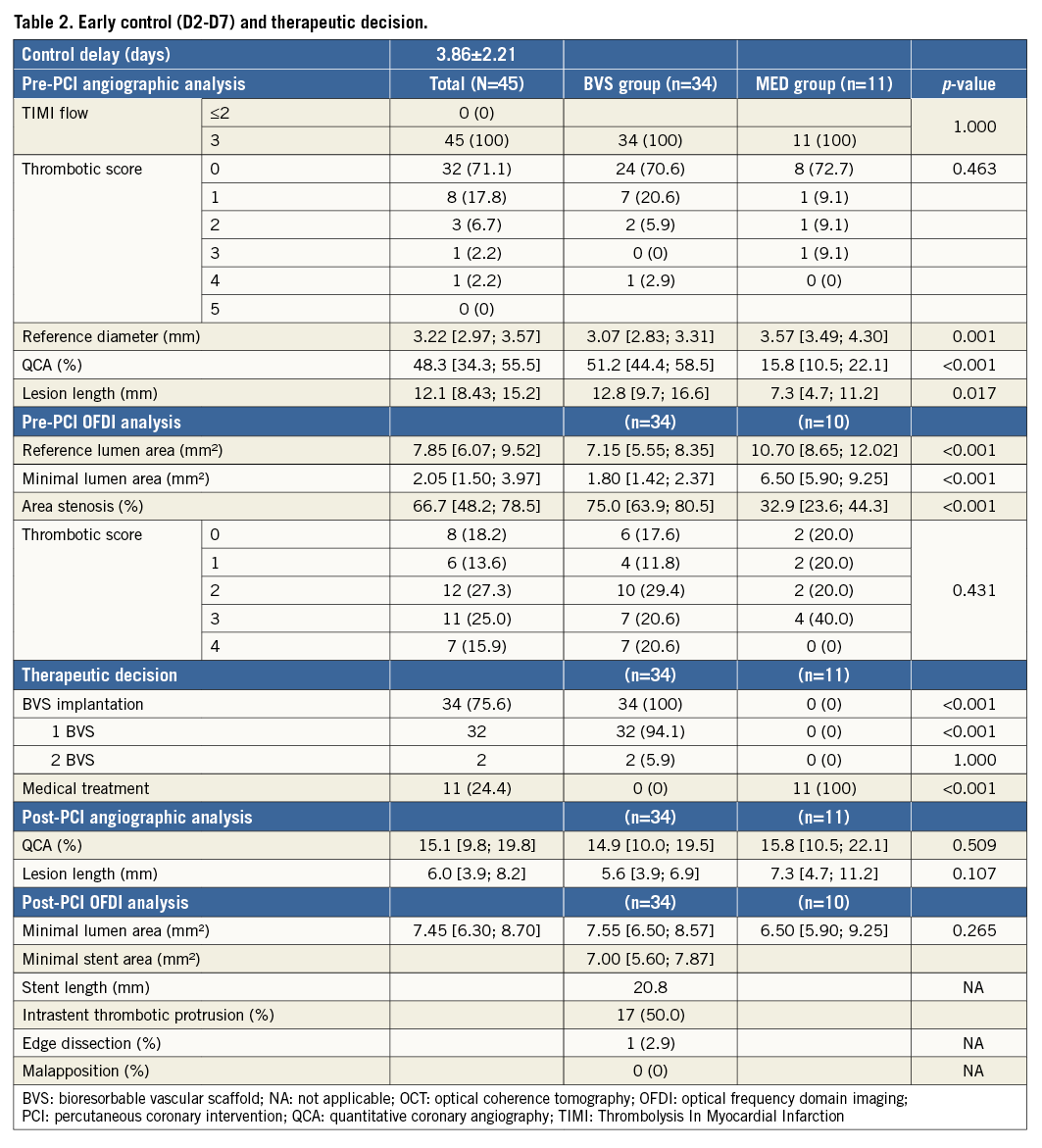
Early control was performed on average on day 3.9 (day 2-day 7). No events occurred between the initial coronary angiography and early control. The OFDI procedure was successfully performed in 100% of cases, without any complications. Thirty-four patients underwent BVS implantation (Figure 3). Eleven patients were treated medically (Figure 4).
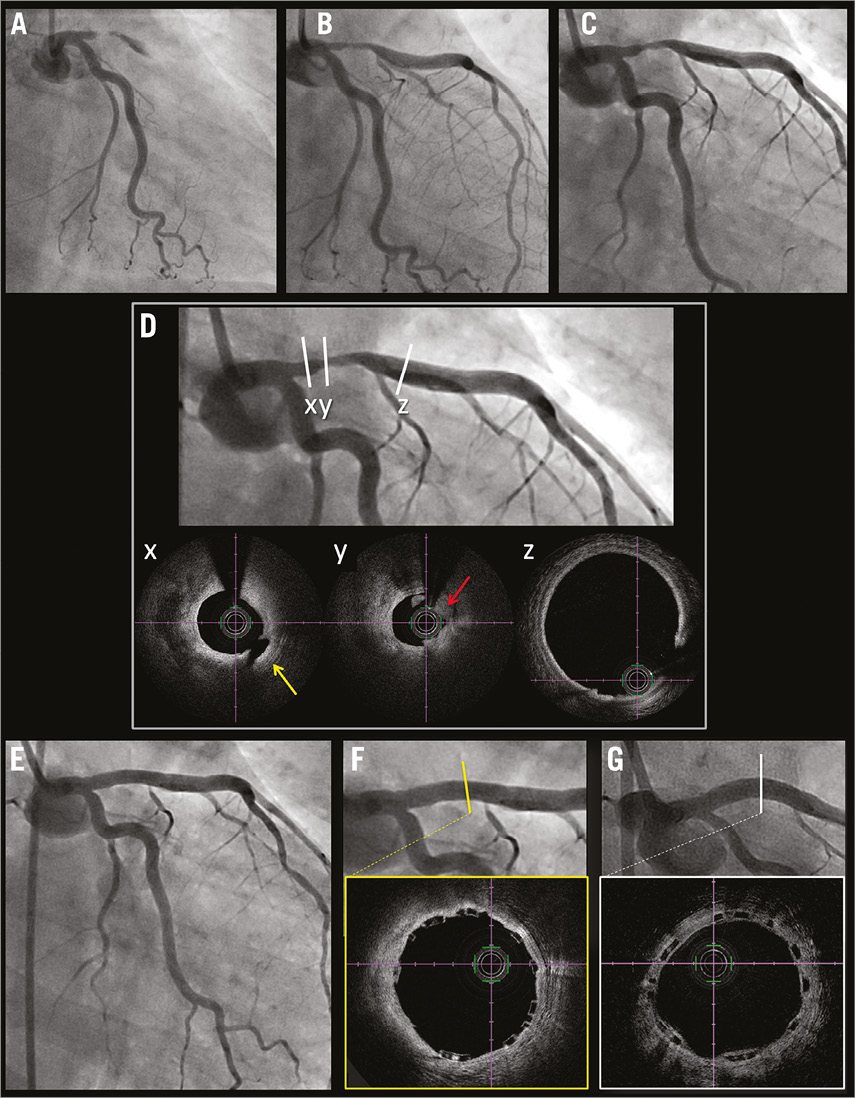
Figure 3. Example of a 47-year-old woman smoker admitted for anterior STEMI and treated with BVS. Occlusion of the LAD (A), restoration of TIMI 3 flow by thrombus aspiration (B). Angiographic control at D4 (C). OFDI at D4 (D) confirming a tight stenosis (88% area stenosis compared to the reference lumen in panel z) with low thrombus load (red arrow in panel y) and plaque rupture (yellow arrow in panel x). Post-BVS implantation angiography (E) with OFDI (F). Angiography and OFDI at six months (G).
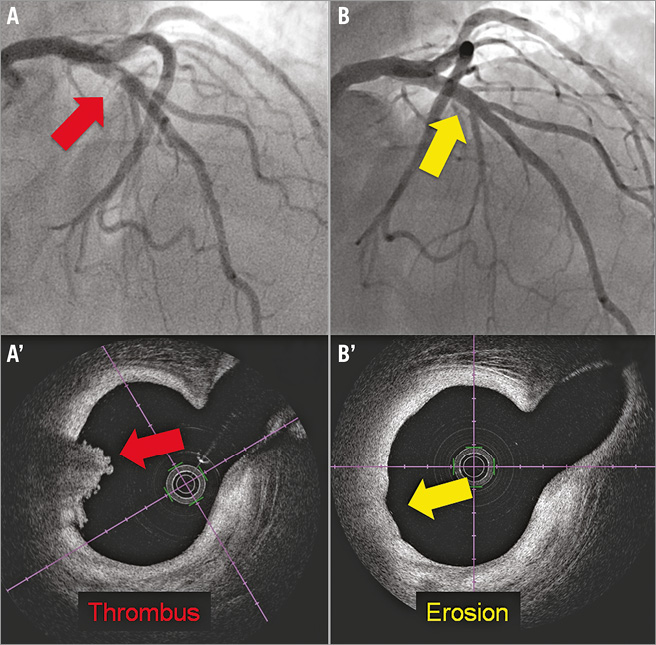
Figure 4. Example of a 46-year-old man admitted for anterior STEMI with initial reperfusion under medical treatment and treated without stent. Initial angiography (A) revealing a thrombus aspect of the LAD with a non-occlusive red thrombus aspect on OFDI (A’) at day 2. Angiography and OFDI at six months (B and B’) with OFDI aspect evocative of plaque erosion.
SIX-MONTH CONTROL RESULTS (Table 3)
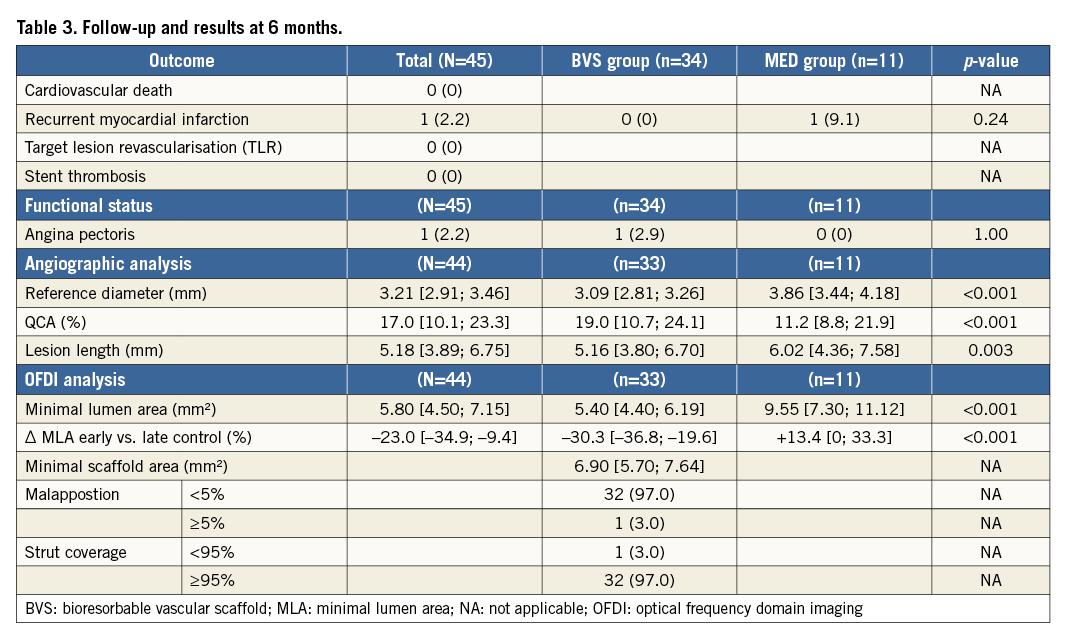
MLA at six months was 5.80 mm2 with 5.40 and 9.55 mm2 in the BVS and MED groups, respectively. We observed an MLA reduction of 23% in the total population. In the BVS group, this reduction reached 30.3% although an increase of 13.4% occurred in the MED group. The minimal stent area was almost the same between the initial and the six-month control (6.90 vs. 7.00 mm2).
FOLLOW-UP
One MACE (recurrent infarction) was observed in the MED group. Initial angiography revealed a thrombotic occlusion of the distal right coronary artery. OFDI performed on day 4 showed no plaque rupture with a small persistent thrombus. One month later, the patient was admitted for another inferior STEMI. Angiography revealed a spasm on the mid segment of the RCA, not on the first culprit lesion.
Discussion
ACS IN YOUNG PATIENTS: SPECIFIC CARE MANAGEMENT?
In our cohort, the largely predominant risk factor was smoking (88.9%). It is likely that vascular inflammation induced by smoking may in part explain the pathophysiological mechanisms of ACS in young subjects which are often the result of atherosclerotic plaque rupture without necessarily being stenotic, as demonstrated by Virmani et al7. This may explain the fact that smokers have more favourable outcomes after fibrinolysis8. Thrombosis is the predominant component of the artery occlusion: in our cohort, 75.5% of patients had a thrombus score of 4 or 5 while less than 5% had none. Percutaneous coronary intervention (PCI) and fibrinolysis are equally beneficial in smokers with STEMI9; however, it could be interesting to use an aggressive antithrombotic strategy in this population with a frequent use of GP IIb/IIIa inhibitors (used in 88.9%) and manual thrombus aspiration. It was used in 60% of cases with no stroke events recorded. Recent studies have not shown any benefit for the systematic use of thrombus aspiration in STEMI10, but we can consider the interest of this tool in specific clinical situations, as suggested by Escaned et al11. Finally, in order to limit the complications of stent implantation in STEMI and to enable OFDI analysis, we opted for a two-stage management strategy. This strategy, developed by many centres1,12, has not shown clinical benefit in recent studies13,14, but we believe that it could be interesting in a selective population. OFDI allowed the presence of plaque rupture or erosion to be confirmed, occasionally without an underlying organic stenotic lesion (Figure 4), and can guide management, either by guiding BVS implantation or by confirming the possibility of continuing medical therapy alone, as suggested by recent studies15 particularly in the case of plaque erosions16. A higher rate of plaque erosion in a selective population is possible but the residual thrombus limits the analysis of ACS mechanisms by OFDI.
CLINICAL OUTCOME
We selected patients with single-vessel disease to keep a simple interpretation of this pilot study. We wanted to prevent any case with a culprit lesion treated medically and a non-culprit lesion treated by stenting. In OFDI, the arterial healing after stenting of culprit lesions in STEMI is comparable between DES (everolimus) and BVS at six months17. OFDI helps to ensure optimal implantation of the BVS, which could explain the absence of thrombosis in our cohort (vs. a 2.1% incidence in the GHOST-EU registry18 and 1.1% at six months in the TROFI II trial17. The reasons for the high device thrombosis rate as compared with metallic DES in ABSORB II at three years19 have not been established but non-optimal implantation (underexpansion, malapposition) could be evocated. Optimal BVS implantation guided by OFDI could reduce these risks and permit better outcomes. Furthermore, limiting implantation of durable intravascular material could affect the quality of life and could explain, for possible psychological mechanisms, the controversial results of the reduction of angina at one year in the ABSORB II cohort20. Finally, even if this argument is secondary, STEMI management without stenting could have an economic interest.
ANGIOGRAPHIC AND OFDI ANALYSES
At six months, MLA analysis was favourable, with a decrease of 7.45 to 5.80 mm2 at six months, representing a 23% reduction. In the MED group, there was a trend for increased MLA, which rose from 6.50 to 9.55 mm2, hence a gain of 13.4%. We observed a reduction in atheromatous plaque volume at the expense of the fibro-lipid core, probably as a result of the effect of statins administered at high dose during the first months (Figure 5). The ALTAIR study21 has shown, in angioscopy and IVUS, a reduction in volume of plaques under high dose statins in stable coronary artery diseases. There was a significant reduction in MLA in the BVS group, which decreased from 7.55 to 5.40 mm2, hence a reduction of 30.3% in lumen area. This can be explained on the one hand by the important thickness of BVS struts, and on the other by neointimal hyperplasia, as demonstrated by Serruys et al in OCT analysis at six months after implantation22. The development of this neointimal hyperplasia is stable over time. The reduction of MLA during the first six months is counterbalanced by the expansion of the scaffold described after six months23.
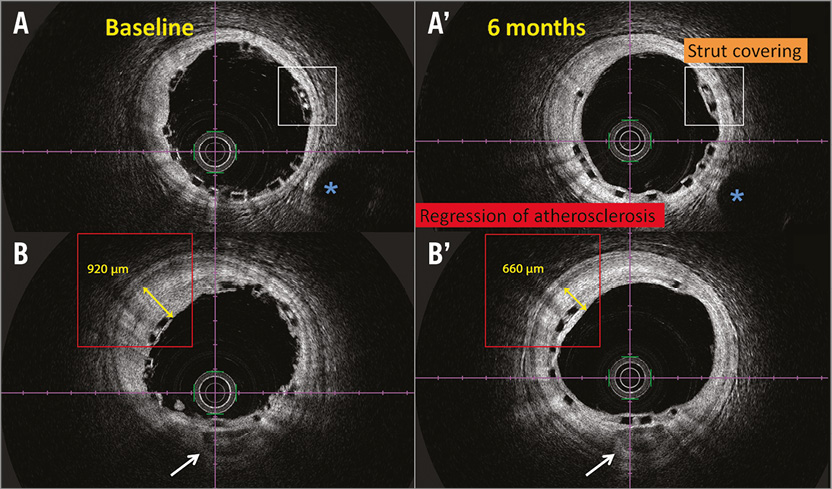
Figure 5. Comparative OFDI frames of BVS. Comparative OFDI frames immediately after implantation (A, B) and at six months (A’, B’). Landmarks: vein (blue asterisk), calcifications (white arrow). The struts are apposed (white rectangle) and covered at six months. The thickness of the atheromatous plaque has decreased at six months (red rectangle).
Study limitations
This was a non-randomised single-centre study conducted on a small sample and a selected population. The results were obtained at six months, before the onset of the polymer resorption process. Because patients pre-treated with fibrinolysis may have a clinical course that differs from those referred directly for primary PCI, the clinical course of our patients should be interpreted accordingly. All of these data would require validation after clinical follow-up and with imaging in the longer term.
Conclusions
This work presents an innovative management of STEMI in young subjects with a single-vessel lesion in which the ultimate objective is to limit implantation of durable intracoronary devices, either by using BVS or by continuing medical treatment alone. The findings herein confirm that this management is a potential treatment option in a selected patient population. This strategy is further enhanced in the present study by OFDI. This concept remains to be validated in a larger-scale randomised multicentre study.
| Impact on daily practice This study proposes a new management of STEMI in young patients by limiting implantation of durable intracoronary devices and with OFDI guidance. In this selective population, a strategy based on aggressive thrombus management and under OFDI guidance could allow medical treatment without stenting. Furthermore, if stenting remains necessary, BVS should be preferred to avoid the late complications of metallic stents. |
Conflict of interest statement
P. Motreff and G. Souteyrand are consultants for Abbott Vascular and Terumo Corp. The other authors have no conflicts of interest to declare.