Abstract
Aims: We evaluated the safety and feasibility of an intracardiac echocardiography probe through the oesophageal route (ICE-TEE) for the monitoring of left atrial appendage (LAA) closure to avoid general anaesthesia.
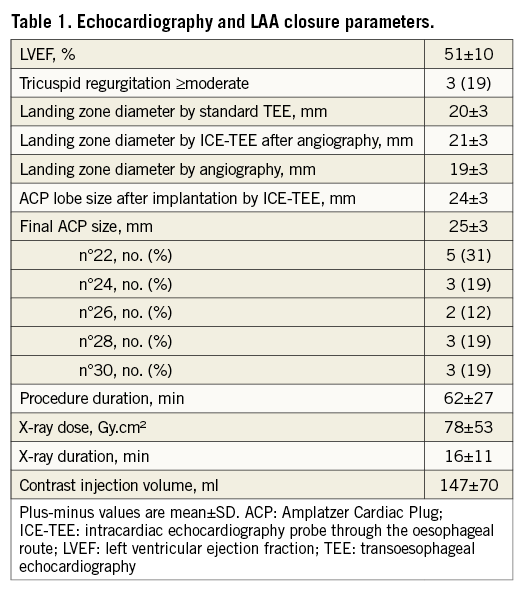
Methods and results: The study included 16 consecutive patients (75±7 years) in atrial fibrillation with high embolism (CHADS-VASc=5±1.4) and bleeding risk (HAS-BLED=4±0.9) referred for LAA closure (Amplatzer Cardiac Plug [ACP]). Standard TEE was performed before device implantation for LAA analysis. During the procedure, ICE-TEE was used under local anaesthesia to determine LAA size and monitor ACP positioning. Maximum and minimum LAA diameter by standard TEE averaged 21±3 mm and 18±1 mm, respectively. Eccentricity index (1.1±0.2) increased with LAA diameter (r=0.73, p=0.001). Maximum LAA size (21±3 mm) obtained by ICE-TEE during the procedure closely correlated with standard TEE measurement (r=0.9, p<0.0001). LAA closure was successfully performed in 15 patients without complication (one failed despite testing three ACP). Implanted ACP size averaged 25±3 mm (range 22-30 mm) and correlated with the size predicted by ICE-TEE (r=0.89) and standard TEE (r=0.57). Procedure duration (62±27 min) correlated with LAA size by ICE-TEE (r=0.71, p=0.002) and eccentricity index (r=0.58, p=0.02).
Conclusions: An ICE-TEE probe through the oesophageal route without general anaesthesia may be used for the monitoring of ACP device implantation.
Introduction
Atrial fibrillation (AF) is the most common arrhythmia1 occurring in 1-2% of the general population, and its prevalence increases with age. AF is associated with a twofold increase in mortality and a fivefold increase in stroke2. It has been estimated that 90% of the thrombi responsible for ischaemic strokes in patients with non-valvular AF originate from the left atrial appendage (LAA)2-4. According to the current European Society of Cardiology guidelines, oral anticoagulant therapy by vitamin K antagonists (VKA) or new oral anticoagulants (NOA)5-7 is indicated in all patients with a high risk of thromboembolism (CHADS-VASc score ≥2)2,8. However, patients with a history of severe bleeding complications under anticoagulation therapy remain theoretically exposed to the risk of stroke. Recent studies have found that LAA closure with an implanted percutaneous device may provide similar efficiency in terms of protection against systemic embolism in atrial fibrillation. Before the procedure, transoesophageal echocardiography (TEE) is recommended to assess LAA shape and size, and exclude thrombus. During the procedure, fluoroscopy monitoring alone may be used9, but TEE is generally repeated to confirm the sizing, optimise the device position and identify early complications10. However, general anaesthesia used for improving TEE tolerance may prevent early detection of neurological complications. In the present study, we report our experience of an intracardiac echocardiography probe used through the transoesophageal route (ICE-TEE) without sedation for LAA closure, as described previously for other procedures11-13.
Methods
STUDY POPULATION
The study included 16 consecutive patients with a contraindication for prolonged anticoagulation referred for LAA closure between November 2011 and December 2012. All patients included had a non-valvular AF with a high risk of thromboembolic complications. For the procedure, only the Amplatzer™ Cardiac Plug (ACP) device (St. Jude Medical, St. Paul, MN, USA) was used. Written informed consent was obtained from all patients and the study was approved by our local ethics committee.
AMPLATZER CARDIAC PLUG DEVICE
The Amplatzer Cardiac Plug device (St. Jude Medical)14 is a nitinol mesh composed of three parts: 1) a lobe with tiny hooks for device anchoring, 2) a sealing disc towards the left atrium, and 3) a stretchable waist connecting the lobe and the disc. The ACP lobe is implanted in the landing zone located one centimetre distally to the LAA ostium. As recommended by the company, the ACP size was calculated as 20% greater than the largest measured landing zone diameter by TEE, ICE-TEE or angiography.
ECHOCARDIOGRAPHY DATA
All patients underwent a standard TEE (Vivid 7; GE Vingmed, Horten, Norway) the day before the procedure to identify the presence of a patent foramen ovale and to exclude the presence of LAA thrombus. LAA measurements were performed using 35-55°, 55-90° and 90-120° views. The landing zone was defined as the LAA internal diameter one centimetre away from the circumflex artery. Three measurements were performed in each view and the maximum diameter was included in the analysis. ICE-TEE (ACUSON AcuNav™ [10 Fr probe frequency set at 7.5 MHz]; Siemens Healthcare, Erlangen, Germany) was only performed for the procedure using a commercially available echocardiographic system (Vivid 7; GE Vingmed). The same contraindications as for standard TEE were respected. The ICE probe was always introduced in the supine position by the nasal route after local nasal anaesthesia. After ICE probe introduction, the first anatomical structure visualised was the descending aorta. Probe clockwise rotation allowed the visualisation of the interatrial septum. LAA and left superior pulmonary vein views were obtained by following a clockwise rotation. The size of the landing zone was compared among the three modalities: angiography, TEE and ICE-TEE.
IMPLANTATION PROCEDURE
The whole procedure was guided by ICE-TEE and fluoroscopy. Access to the left atrium was achieved through the femoral vein after a transseptal puncture. ICE-TEE was used to guide and secure the transseptal puncture position which should be inferior and posterior to avoid aorta puncture and give an easy access to the LAA. A guiding catheter was then passed through the transseptal puncture and a pigtail catheter was advanced towards the LAA. The landing zone was measured by ICE-TEE after LAA angiography. The pigtail catheter was replaced with the delivery system carrying the closure device. The device was advanced towards the LAA and the opening and proper positioning of the ACP lobe were verified by ICE-TEE. Once the location was verified, the ACP disc was expanded in the left atrium to occlude the LAA orifice. Colour Doppler was used to assess any flow around the device. If no flow was detected and the LAA appeared completely isolated from the main left atrium, the device was released and the catheters removed.
STATISTICAL ANALYSIS
Continuous variables with a normal distribution are expressed as mean±standard deviation (SD) and dichotomous data are expressed as percentages. Comparison was performed using a t-test for continuous variables and a χ² test for percentages. Paired analysis was performed when required. Agreement between the predicted size and the device used was assessed using Kendall’s correlation for paired comparison. For all analysis, significant statistical difference was considered for a p-value of <0.05.
Results
All patients (mean age 75±7 years) included in the study had a relative contraindication to VKA with high thromboembolic (CHADS-VASc=5±1.4, range 3-8) and bleeding risk (HAS-BLED=4±0.9, range 3-5). No patient had significant left valvular disease and three patients had severe functional tricuspid regurgitation. No PFO or LAA thrombus was detected by standard TEE before the procedure. ICE probe introduction through the nasal route and the procedure monitoring were perfectly tolerated in all patients without any sedation.
LAA landing zone measurement
The appendage diameter averaged 18±1 mm (median=19 mm, IQR=2.0) for the TEE view between 35° and 55°, 21±3 mm (median= 21 mm, IQR=3.5) between 55° and 90° (circumflex view), and 19±3 mm (median=19 mm, IQR=5) between 90° and 120°, respectively. The circumflex view systematically provided the greatest LAA diameter and 35° to 55° views the smallest diameter. Eccentricity index, defined as maximum over minimum LAA size ratio (mean= 1.1±0.2, range 1.0 to 1.5), increased with LAA diameter (r=0.73, p=0.001).
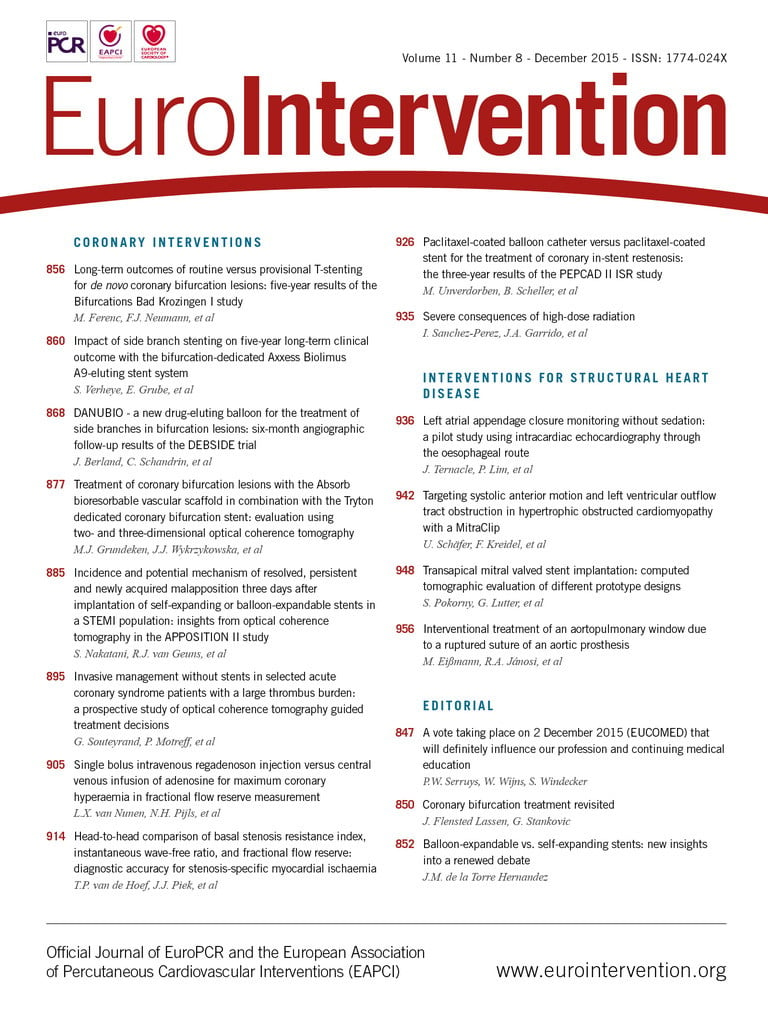
Maximum LAA diameter obtained by ICE-TEE (mean=21±3 mm) during the procedure closely correlated with those obtained by standard TEE (r=0.9, p<0.0001) (Figure 1, Figure 2). Angiographic measurement (mean=19±3 mm; median=19 mm, IQR=4.5) correlated better with ICE-TEE (r=0.85, p<0.0001) than with standard TEE measurement (r=0.72, p=0.002) (Figure 3).
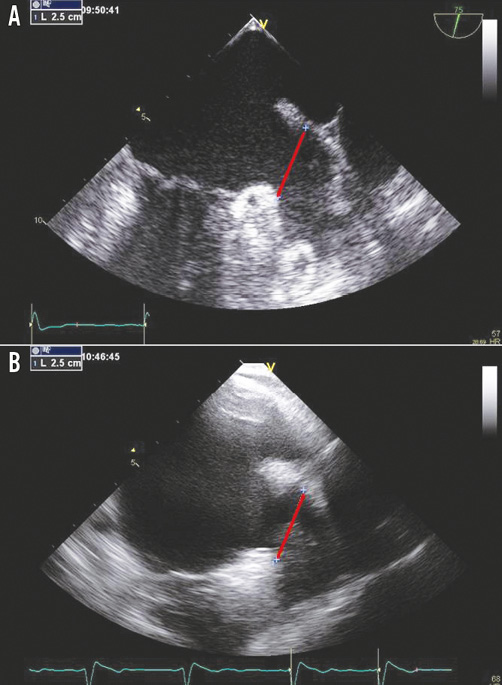
Figure 1. Left atrial appendage landing zone sizing by standard transoesophageal echocardiography (A) and intracardiac echocardiography probe through the oesophageal route (B).
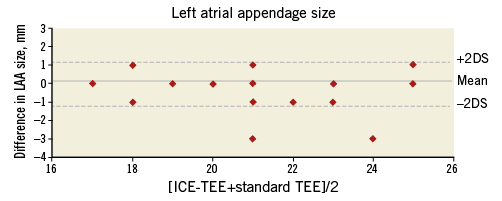
Figure 2. Agreement between left atrial appendage landing zone sizing by standard transoesophageal echocardiography and intracardiac echocardiography probe through the oesophageal route.
Figure 3. Agreement between left atrial appendage landing zone sizing by angiogram and standard transoesophageal echocardiography (A), and intracardiac echocardiography probe through the oesophageal route (B).
ICE-TEE FOR PROCEDURE MONITORING
LAA closure was successfully performed in 15 patients (Figure 4). Despite similar measurements obtained by standard TEE, ICE-TEE and LAA angiography, the specific LAA anatomy (large neck) required changing the ACP device size during the procedure to a larger size in two patients (24 mm to 26 mm, and 26 mm to 28 mm). The LAA closure device was repositioned in one patient because of incorrect ACP lobe positioning in front of the circumflex artery (Figure 5). No neurological complication or pericardial effusion was observed (Table 1), and LAA closure only failed in one patient despite the use of three different device sizes because of instability due to an unfavourable LAA anatomy for ACP lobe grip. Finally, the implanted ACP size averaged 25±3 mm (range 22-30 mm) and correlated with the size predicted from ICE-TEE (r=0.89) better than from standard TEE (r=0.66) and LAA angiography (r=0.73). Procedure duration (62±27 min, x-ray exposure=78±53 Gy.cm²) correlated with the LAA size (r=0.71, p=0.002) obtained by ICE-TEE and eccentricity index (r=0.58, p=0.02).
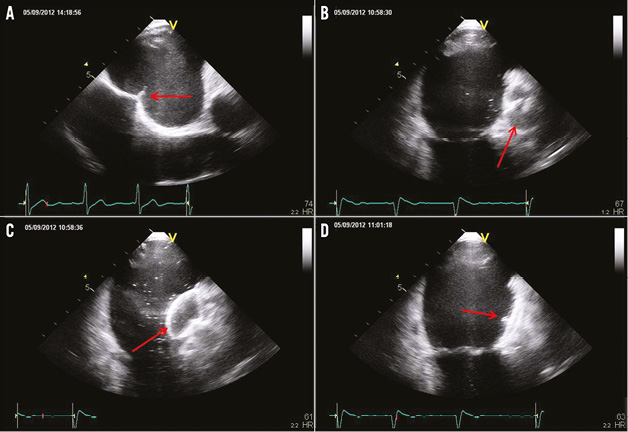
Figure 4. Monitoring of left atrial appendage closure: transseptal puncture guidance (A), Amplatzer Cardiac Plug lobe (B) and disc (C) deployment, and final control of the device position (D).
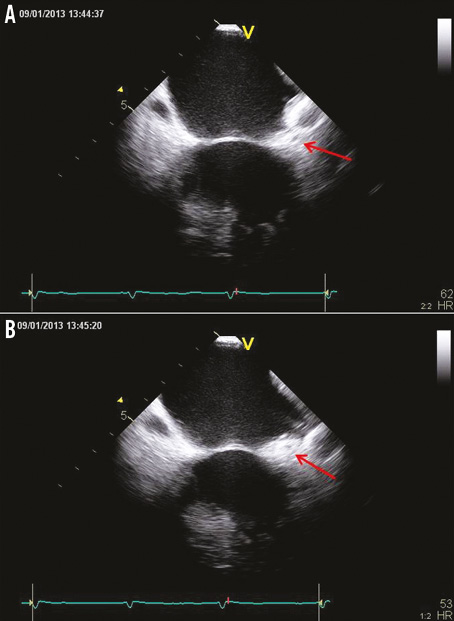
Figure 5. Misplacement of the Amplatzer Cardiac Plug lobe identified by intracardiac echocardiography probe through the oesophageal route (A). The correct position of ACP lobe is behind the circumflex artery (B).
Follow-up
During the follow-up period (mean 2.3 months), one patient experienced a stroke related to a severe carotid stenosis, and one patient developed a thrombus appended to the LAA device. However, no device embolisation or late pericardial effusion was observed.
Discussion
Standard TEE used to guide and secure LAA closure procedures requires general anaesthesia and mechanical ventilation. The present study demonstrates that an ICE probe (ACUSON AcuNav; Siemens Healthcare) may be safely used through the oesophageal route to size the LAA landing zone and to monitor the device positioning, deployment and stability. LAA diameter assessed by ICE-TEE was closely correlated to standard TEE measurement.
A careful analysis of LAA appendage by standard TEE is required before the procedure to exclude thrombi and to size LAA diameter. Particular care in evaluating LAA shape15 may be helpful to predict difficulties during the implantation process. As observed in the present study, ACP implantation duration is greater in large and eccentric LAA, probably because of the difficulty of stabilising the anchoring system. TEE is also recommended to monitor the procedure but general anaesthesia is often required to improve patient comfort and avoid pulmonary complications. However, early diagnosis of neurological complications is challenging in sedated patients, and LAA appendage procedure duration and cost are increased when general anaesthesia is required. Fluoroscopy-only monitoring in non-sedated patients can be envisaged9, but this is still the exception worldwide. An ICE catheter is an interesting alternative to standard TEE for the monitoring of interatrial septum puncture. Several groups have demonstrated that the LAA anatomy may be accurately imaged by an ICE catheter16, and recent studies have suggested that ICE may be used as an alternative to TEE for LAA closure monitoring17. However, ICE is an invasive tool which requires experience, and there is a specific learning curve. Moreover, the cost of a single-use probe is a strong limitation in many European countries.
To overcome these limitations, we propose the use of an ICE probe through the oesophageal route as an alternative to standard TEE and ICE monitoring. In previous studies, we demonstrated that ICE-TEE could be routinely used to monitor PFO closure11 and transseptal puncture during an atrial fibrillation (AF) ablation procedure12. Despite its monoplane imaging, ICE-TEE does not require a specific learning curve and provides an excellent image quality13. ICE-TEE is routinely used in our institution with the same contraindication as standard TEE for the monitoring of transseptal puncture (>300 patients) during AF ablation with a perfect tolerance and no complications reported. Importantly, ICE-TEE is cost-effective since the ICE probe can be used several times after a standard sterilisation procedure. In the specific setting of LAA closure, transseptal puncture, as well as device positioning and deployment, can be accurately monitored. Moreover, ICE-TEE provides a comparable LAA diameter to standard TEE. We also believe that stroke or haemodynamic complications may be diagnosed and treated earlier in conscious patients monitored by ICE-TEE.
Limitations
This is a pilot, non-randomised study that includes a limited number of patients at high risk of stroke and bleeding, since the LAA closure procedure is relatively new. Despite a better agreement between the ICE-TEE measurement and the size of the implanted ACP device, the superiority of ICE-TEE over standard TEE cannot be stated. Moreover, the LAA size determined by TEE may be slightly different from that measured 24 hrs later by ICE-TEE. The study reported the feasibility and safety of ICE-TEE in LAA closure procedures. We believe that this approach may be interesting in patients at high risk of general anaesthesia, particularly in cardiac centres with a limited experience with conventional ICE. Importantly, accurate evaluation of LAA dimensions and shape should always be performed before the procedure, preferably by three-dimensional (3D) TEE and at least by standard TEE, because only the maximum LAA diameter can be obtained from ICE-TEE monoplane imaging. This limitation should be overcome in the next year by the development of multiplane micro-TEE and 3D ICE probes. Finally, we think that deep throat anaesthesia should be avoided because of the risk of aspiration.
Conclusion
An intracardiac echocardiography probe used through the oesophageal route without general anaesthesia may be used for the sizing and monitoring of left atrial appendage closure with an ACP device.
| Impact on daily practice Transoesophageal echocardiography is generally used for the monitoring of left atrial appendage closure. A general anaesthesia with mechanical ventilation is required to avoid discomfort. However, early diagnosis of neurological complications is challenging in sedated patients. This study demonstrates that an intracardiac echocardiography used through the oesophageal route without sedation may be used for the monitoring of LAA closure with an ACP device. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
| Excerpt from the reviewer 1) The authors mention that 2D/3D has been addressed by ICE. It is difficult to say whether the probe and programme used allow 3D and biplane capability. As LAA closure moves forward, we believe this will be necessary for better alignment and deployment. 2) The idea that using ICE-TEE is better for the patient is uncertain. We have the following major concerns: a) the cost per probe is prohibitive b) 3D and biplane capability are lost c) a TEE probe is required anyway earlier to rule out thrombus; the fact that this is done at an earlier visit means two visits for the patient and he has to swallow a probe twice. On the other hand, the authors mention the following – patient comfort and also decreased global fluoroscopy time. A) Patient comfort – the probe is not usually in for two hours; it is often in for 30 minutes for a full LAA case. If anything, this is a shortened overall procedure time for the patient! If the ICE algorithm is followed, the patient has to be NPO for two events, be sedated for two events, and have two visits to the hospital and away from work or home. B) Decreased global fluoroscopy time – the TEE person can work behind a shield, greatly limiting their exposure. Under the ICE-TEE method, the second operator who is handling the ICE probe is exposed to fluoroscopy when they would not have had to be doing so otherwise. |