Aortic valve stenosis (AS) may be unpredictable in that the degree of valve narrowing often does not correlate with the functional limitations of the patient. In current practice guidelines, aortic valve replacement (AVR) has a class I recommendation for symptomatic patients with severe AS, but valve replacement in asymptomatic patients has a class IIb recommendation.
The characteristics of asymptomatic patients with severe AS who are considered under this IIb recommendation include an abnormal response to exercise testing (development of hypotension and/or symptoms) and extremely severe AS (aortic valve area less than 0.6 cm2, mean gradient >60 mmHg, and jet velocity greater than 5.0 m per second); consideration of AVR in such patients presumes a low (1.0% or less) operative mortality1. Other patients who may be considered to have a IIb indication for surgery are those with a high likelihood of rapid progression of valve stenosis (increased age, heavy valve calcification, and coronary artery disease). Aortic valve replacement may also be reasonable in patients who have aortic stenosis and are undergoing other cardiac surgery such as coronary artery revascularisation or mitral valve repair or replacement. Guidelines from the European Society of Cardiology and the European Association for Cardio-Thoracic Surgery for AVR in asymptomatic patients are similar to those from the ACC/AHA, but the European guidelines add as a class IIb recommendation elevation of natiuretic peptide levels or excessive left ventricular hypertrophy in the absence of systemic hypertension2.
The rationale for AVR in asymptomatic patients is prevention of symptoms, irreversible left ventricular dysfunction, and cardiac death. Asymptomatic patients with severe AS have a high likelihood of developing symptoms during follow-up. In a study from our Clinic, Pellika et al reported that, among patients who did not undergo AVR, the probablility of developing cardiac symptoms was 18% at one year, 33% at two years, and 67% at five years following diagnosis. Risk factors for the development of symptoms have been alluded to and include a smaller aortic valve area and presence of left ventricular hypertrophy3. In other publications, older age, presence of atherosclerotic risk factors, development of symptoms during stress testing, and elevated plasma levels of natiuretic peptides have been identified as predictors of symptom development2. Williamson and Gelfand stated that the most predictive characteristic for development of symptoms is the degree of stenosis as determined by the physiologic valve area4. Even though there are no class I indications for AVR in asymptomatic patients, approximately 45% of patients in our series had AVR prior to the development of symptoms; indeed, by three years following diagnosis of AS, 52% of the patients had developed symptoms, had undergone AVR, or had died (Figure 1)5.
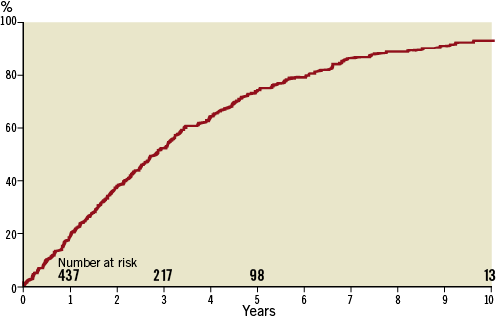
Figure 1. Cumulative risk of death, aortic valve replacement, or symptoms in patients with asymptomatic severe aortic valve stenosis. (Figure from Brown ML et al, J Thorac Cardiovasc Surg. 2008;135:308-15. Reproduced with permission from Elsevier Limited, Oxford, United Kingdom)
Another consideration in the management of asymptomatic patients with severe AS is the development of left ventricular dysfunction before the onset of cardiac limitations6. Although this is a rare occurrence, valve replacement does not appear to improve late survival of asymptomatic AS patients with left ventricular dysfunction7.
The survival benefit of AVR for symptomatic patients with AS has been well established, even in patients with advanced age8,9. Cardiac death, especially sudden cardiac death (SCD), is the most feared complication in asymptomatic patients with severe AS who are being observed. Recent natural history studies, however, suggest that the risk of sudden death in asymptomatic patients with severe AS is relatively low, approximately 1% per year3,6,10.
Other practical issues need to be considered in management of asymptomatic patients. Progression of aortic valve narrowing and development of symptoms is common. Upon learning this, many elderly patients may reasonably ask whether early AVR may be the best strategy for them, if their general health is good, in order to avoid operation at a later date when frailty and comorbid conditions may increase surgical risk and complicate postoperative recovery. Although risk of sudden death is low overall, death after development of symptoms and before operation is a theoretical risk that would be decreased by AVR while the patient is asymptomatic.
Early and late outcomes of AVR in asymptomatic patients with severe AS is excellent. In our follow-up of 263 patients who were initially asymptomatic and underwent AVR, survival at five years postoperatively was 85% and at 10 and 15 years was 64% and 36%, respectively. Indeed, as Brown et al have demonstrated, asymptomatic patients undergoing AVR have a 15-year survival similar to an age and gender matched population (p=0.985)5. As seen in Figure 2, survival after AVR was best in patients who had the operation before onset of symptoms (10-year survival 70% versus 62%), and survival of both surgical groups was dramatically better than that of unoperated patients. The 10-year survival of asymptomatic patients who did not have AVR was only 33%.
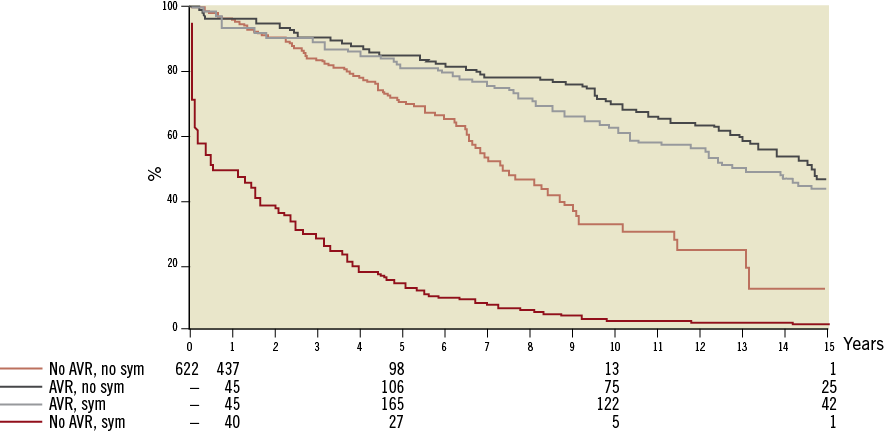
Figure 2. Among patients with severe asymptomatic aortic valve stenosis, survival was best in patients who had valve replacement while asymptomatic. (Figure from Brown ML et al, J Thorac Cardiovasc Surg. 2008;135:308-15. Reproduced with permission from Elsevier Limited,Oxford,United Kingdom)
In a prospective study, Kang et al found lower mortality, both cardiac-related and overall mortality, in patients undergoing operation for asymptomatic AS compared to those who were conservatively managed. In this series, six-year mortality (overall and cardiac-related) was 2% and 0% in the group that underwent AVR compared to 32% and 24% in unoperated patients11.
Several risk scores have been developed to stratify patients with asymptomatic AS. From our institution, Le Tourneau et al examined the value of an operative risk assessment (Society of Thoracic Surgeons [STS] score) in predicting outcome of patients with asymptomatic AS. The STS score was highly predictive of overall survival (Figure 3). Among patients with an STS score <4%, there was no difference in survival of patients managed surgically or conservatively (p=0.83). However, in those patients with STS scores >4, there was a significant survival advantage with operation and, as shown in Figure 4, this improvement in survival with AVR was especially evident in patients with STS scores >4 and <6.512. The advantage of AVR in the risk assessement of asymptomatic patients depends upon operative mortality in individual centres. In the analysis by Le Tourneau et al, AVR operative mortality was 1.9%, but nationally median operative mortality for AVR was 3.1% (interquartile range, 2.4% to 4.0%)13. Thus, in some centres, the risk-benefit analysis of AVR in asymptomatic patients with severe AS may favour observation. When operative mortality is low, however, early surgery for valve replacement appears to confer a survival benefit.
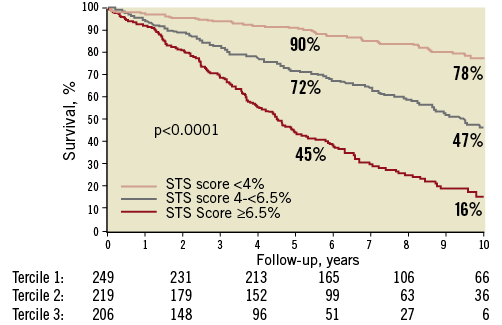
Figure 3. Different survival based on the Society of Thoracic Surgeons operative risk score. ( Figure from Le Tourneau T et al, Ann Thorac Surg. 2010;90:1876-83. Reproduced with permission from Elsevier Limited, Oxford, United Kingdom)
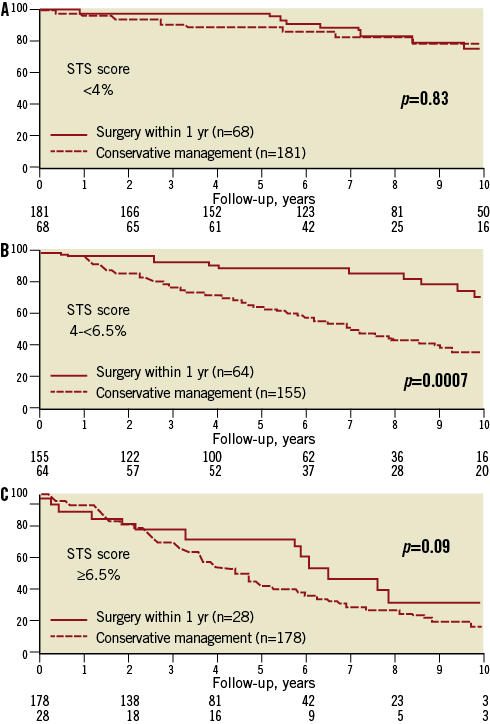
Figure 4. Difference in survival comparing patients undergoing early surgery and medical management stratified by Society of Thoracic Surgeons operative risk estimate. (Figure from Le Tourneau T et al, Ann Thorac Surg. 2010;90:1876-83. Reproduced with permission from Elsevier Limited, Oxford, United Kingdom)
Conflict of interest statement
The authors have no conflicts of interest to declare.

