Pros: trials that challenge the guidelines
Victoria Delgado, MD, PhD
Current international guidelines recommend aortic valve replacement (AVR) in severe aortic stenosis (AS) if it is causing symptoms or left ventricular systolic dysfunction (left ventricular ejection fraction [LVEF] <50%). However, several registries have shown that performing AVR when symptoms or reduced LVEF occur is associated with poor outcomes. Staging algorithms that consider the extent of structural and/or functional alterations associated with AS help to refine the risk stratification of patients with severe AS1. Accordingly, the question that then arises is whether performing AVR in asymptomatic patients with severe AS and no clear structural and functional abnormalities in response to the pressure overload would lead to better survival as compared to a watchful waiting strategy. This hypothesis was tested in 2 recent randomised trials that included patients with critical AS and patients with severe AS and a negative exercise test, respectively23; however, both trials had a limited number of patients. The mean age of the patients was around 65 years old and the proportion of bicuspid aortic valve anatomy was more than 50% in one of the trials: characteristics that do not resemble those of the patients currently treated with transcatheter aortic valve implantation (TAVI). In addition, recruitment of patients was performed almost entirely in a single centre in one of the trials2, while in the other trial, the heart valve clinics did not confirm symptomatic status nor utilise the watchful waiting strategy3. The ongoing Evaluation of Transcatheter Aortic Valve Replacement Compared to Surveillance for Patients With Asymptomatic Severe Aortic Stenosis (EARLY TAVR; ClinicalTrials.gov: NCT03042104) trial, which aimed to recruit more than 1,000 asymptomatic patients with severe AS, will shed more light onto the survival benefits of early intervention.
Meanwhile, large registries have shown that patients with moderate AS have worse clinical outcomes as compared to patients with less severe forms of AS4. Independent of the presence of reduced LVEF, diastolic left ventricular systolic dysfunction and other comorbidities, moderate AS is associated with a 5-year mortality rate of 56%4. A recent systematic review of 12,134 patients with moderate AS, who were followed up for a median of almost 4 years, showed pooled rates per 100 person-years of 9.0 events for all-cause death, 4.9 for cardiac death, 3.9 for heart failure and 1.1 for sudden death5. In addition, the presence of symptoms or left ventricular systolic dysfunction were associated with a significant impact on the overall estimate of all-cause death5. These findings lead to the hypothesis that AVR would be beneficial in patients with moderate AS, particularly in those with symptoms and/or left ventricular dysfunction.
Currently, surgical AVR should be considered in patients undergoing surgical coronary artery revascularisation or surgery of the aortic root and ascending aorta. However, the low complication rates of TAVI and the lower in-hospital mortality rates of TAVI as compared to surgical AVR in patients with low, intermediate and high operative risk begs the question of whether TAVI could be a valuable option for patients with moderate AS. In particular, among patients with moderate AS and reduced LVEF or heart failure symptoms and in whom there is no indication for coronary revascularisation or surgery of the aortic root and ascending aorta, TAVI could alleviate the pressure overload of the failing left ventricle and improve symptoms as well as left ventricular remodelling. To answer this question, 3 ongoing randomised trials will provide more information. The Transcatheter Aortic Valve Replacement to UNload the Left Ventricle in Patients With ADvanced Heart Failure (TAVR UNLOAD; ClinicalTrials.gov: NCT02661451) trial is aiming to recruit 300 patients with heart failure and moderate AS who will be randomised to TAVI using a balloon-expandable bioprosthesis versus guideline-directed heart failure therapy. The results are expected in 2023. The PROGRESS Trial: Management of Moderate Aortic Stenosis by Clinical Surveillance or TAVR (ClinicalTrials.gov: NCT04889872) will randomise 750 patients with moderate AS and symptoms or cardiac damage to TAVI with a balloon-expandable bioprosthesis versus medical therapy, while the Evolut EXPAND TAVR II Pivotal Trial (ClinicalTrials.gov: NCT05149755) will randomise 650 patients with symptomatic moderate AS to TAVI versus clinical surveillance under medical therapy. Besides knowing the potential survival benefit of TAVI in patients with moderate AS, it will certainly be interesting to see if TAVI is associated with a regression of the haemodynamic consequences of the increased pressure overload. This hypothesis will be challenged by the risk of pacemaker implantation and the presence of more than mild paravalvular regurgitation associated with TAVI. While the concept of performing TAVI in moderate AS seems reasonable from the pathophysiological point of view, the results of these trials will help to demonstrate this.
Conflict of interest statement
V. Delgado received speaker fees from Abbott Vascular, Edwards Lifesciences, Medtronic, GE Healthcare, Philips, and Novartis; and consulting fees from Edwards Lifesciences, and Novo Nordisk (heart failure).
Cons: TAVI, a role to be explored
Michele Senni, MD, PhD; Paolo Manca, MD
The prevalence of both AS and heart failure (HF) increases exponentially with advancing age, leading to a frequent coexistence of the 2 conditions in the elderly. Consistent data are available about the prognostic role of severe AS in HF patients, and the benefit of TAVI for this condition has been demonstrated6. Conversely, data on patients with moderate AS and HF are scarce and derived from small observational studies78910. Furthermore, the possible role of TAVI in this population is almost unexplored7.
In a cohort of 262 patients affected by heart failure with reduced ejection fraction (HFrEF) who were matched with a corresponding group without AS, moderate AS was shown to be a strong independent predictor of HF hospitalisation and mortality (hazard ratio [HR] 2.34)7. In the same study, 44 patients with baseline moderate AS required AVR during follow-up. In this subgroup, TAVI, but not surgical AVR was associated with survival benefit; however, TAVI was performed in only 15 patients. Furthermore, patients who underwent AVR had worse baseline characteristics compared to the other cohorts and could not be adequately matched. Lastly, HF treatment was not optimal and did not include new HF therapies such as angiotensin-neprylisin inhibitors and sodium-glucose cotransporter 2 inhibitors. Another recent study, which enrolled 952 patients affected by moderate AS who were matched with a comparable population without AS, found similar results, showing a significantly higher risk of mortality in moderate AS patients, regardless of left ventricular ejection fraction8. However, HF prevalence in this study was low (<10%), and patients who underwent AVR were excluded. Moreover, some baseline differences between the 2 groups still remained after matching, leaving doubts regarding the possible independent prognostic role of moderate AS.
In contraposition, a previous report which included 107 patients with low-flow low-gradient AS and HFrEF demonstrated a significantly lower risk of death in patients affected by moderate AS compared to those with severe AS (HR 0.53)9. Also, a group of 28 HFrEF patients with moderate AS was adequately matched with 28 HFrEF patients without AS and no difference in the 5-year survival rate was documented.
Lastly, in a recently published series of 1,974 patients affected by moderate AS, who were divided into 4 groups based on flow-gradient patterns, only paradoxical low-flow low-gradient and classical low-flow low-gradient moderate AS emerged as independent predictors of mortality, while concordant moderate AS and normal-flow AS did not5. Interestingly, patients with these patterns were also significantly older and had a higher prevalence of comorbidities.
Taking all these data together, the independent prognostic role of moderate AS in HF remains unclear, with some conflicting results in the literature. The number of patients enrolled in these reports was usually low, and the possible beneficial role of TAVI was only reported in a very small sample size, clearly limiting the conclusions for this population. It should instead be emphasised that optimal medical treatment was generally underrepresented and it must be implemented in future studies. Additionally, the prompt treatment of comorbidities, which are usually seen in these patients, is fundamental as they could independently act as casual factors for the ventricular-valvular afterload observed in AS patients. Finally, whether moderate AS may have a different impact in patients with HFrEF or HF with preserved ejection fraction (HFpEF) is still controversial (Figure 1).
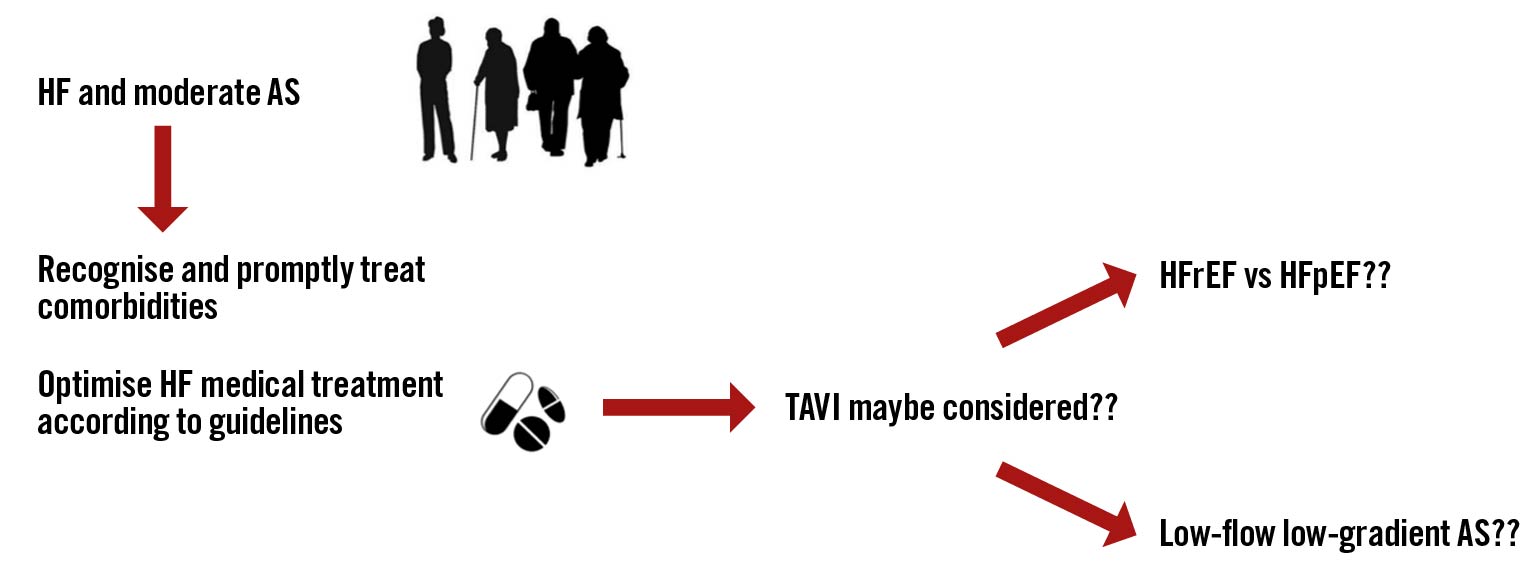
Figure 1. Possible flowchart of the treatment of patients with heart failure and moderate aortic stenosis. AS: aortic stenosis; HF: heart failure; HFpEF: heart failure with preserved ejection fraction; HFrEF: heart failure with reduced ejection fraction; TAVI: transcatheter aortic valve implantation
Conflict of interest statement
The authors have no conflicts of interest to declare.