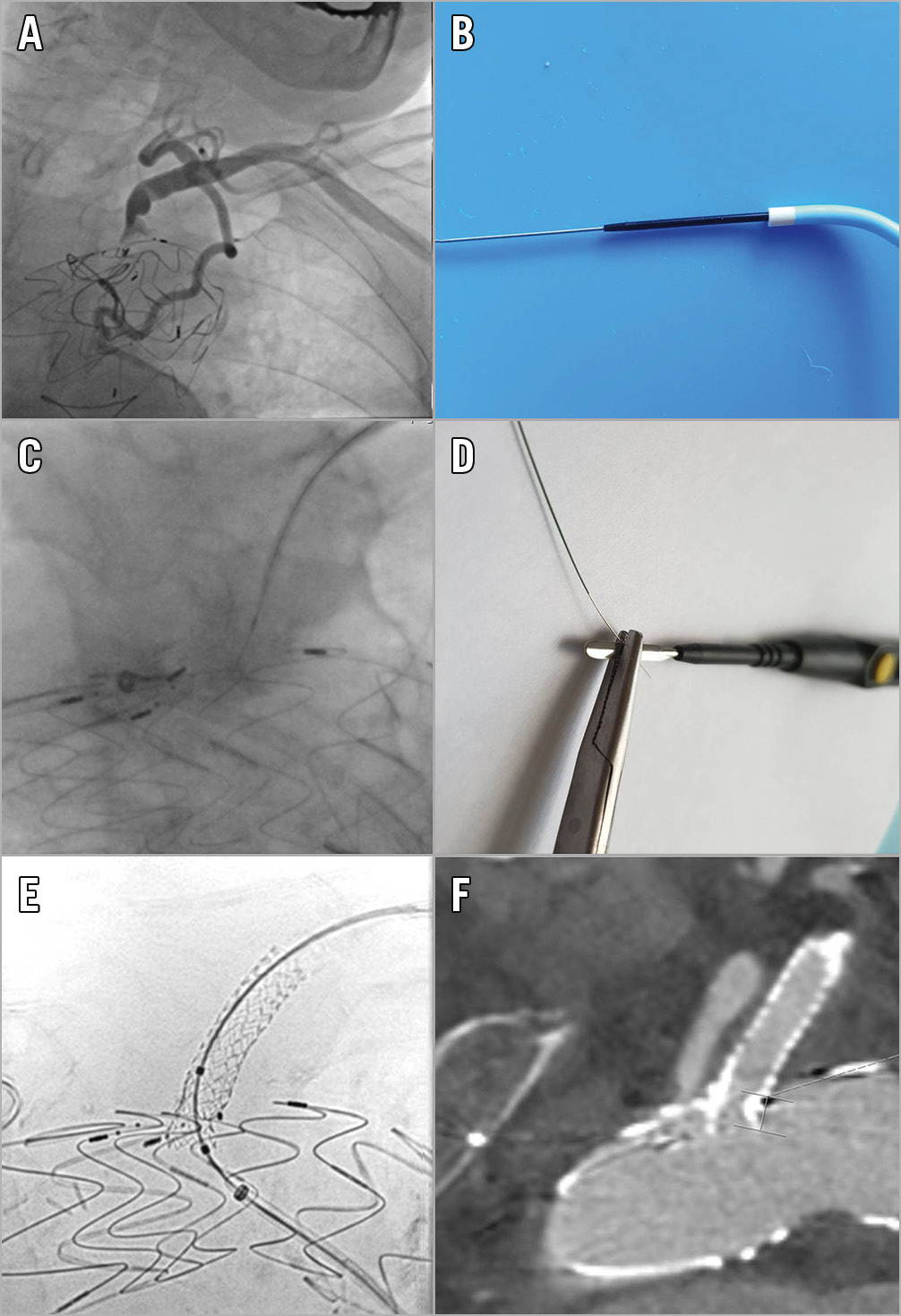
Figure 1. Steps of the procedure and the result. A) Angiography of the left subclavian artery. B) Telescopic system of the wire in the PiggyBack in the JR4 diagnostic catheter. C) Guidewire penetration through the stent graft fabric. D) Wire connected to electrosurgery pencil using a needle driver outside of the patient’s body. E) Stent enhancement imaging after stent implantation in the left subclavian artery through the fenestration. F) CT angiography after the procedure.
A 77-year-old man with a history of coronary artery bypass surgery including a left internal thoracic artery graft had undergone thoracic endovascular aortic repair (TEVAR) for a penetrating aortic ulcer at an external hospital. The left subclavian artery (LSA) had been covered (Figure 1A). The patient was admitted to our institution four months after TEVAR for shortness of breath and worsening of left ventricular ejection fraction. After multidisciplinary discussion we decided to fenestrate the previously implanted graft percutaneously.
Left brachial access was used for penetration of the TEVAR graft and right femoral access was used for delivery of stents. A 6 Fr JR4 diagnostic catheter was placed in the LSA ostium via the left brachial access. A Confianza Pro 12 wire (Asahi Intecc, Aichi, Japan) was preloaded into a PiggyBack® wire converter (Teleflex Medical, Wayne, PA, USA) and inserted into the JR4 catheter (Figure 1B). The wire was directed to transverse the graft under biplanar fluoroscopy guidance (Figure 1C). Using pecking motions of the wire we ensured that the perforation point was away from the stent skeleton of the graft and that the wire direction was perpendicular to the graft’s fabric. The wire was then clamped to an electrosurgery pencil outside the patient’s body and electrified with “cutting” energy of 80 W (Figure 1D). Using a neutral electrode of the monopolar electrosurgery on the patient’s hip, radiofrequency energy within the insulating PiggyBack was thereby conducted to the wire’s tip. Gentle pushing advanced the wire through the graft into the aorta without noticeable resistance. The PiggyBack device easily followed the wire across the wall of the graft. The wire was exchanged for a 0.014-inch 300 cm workhorse wire (BMW Universal; Abbott Vascular, Santa Clara, CA, USA), snared and externalised via the femoral sheath. The crossing site of the graft was predilated and a balloon-expandable stent graft 8x38 mm (Advanta™ V12; Atrium Medical Corporation, Hudson, NH, USA) and an additional 8×15 mm balloon-expandable non-covered stent (PALMAZ GENESIS™; Cordis, Cardinal Health, Milpitas, CA, USA) were introduced via the transfemoral route and implanted in the LSA with slight protrusion into the aorta (Figure 1E, Figure 1F). Post-interventional measurement revealed no pressure gradient between left brachial artery and aorta.
The presented technique has been used in a similar fashion in electrified guidewire-assisted transseptal puncture, transcaval access, aortic valve laceration, or the LAMPOON technique1,2,3,4. The procedure described enables ad hoc in situ fenestration of TEVAR grafts even in urgent cases and allows an extension of the aortic arch landing zone by intentional LSA coverage.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.