Abstract
Since their introduction in the clinical setting home and ambulatory blood pressure measurements have gained growing popularity in the diagnosis and treatment of essential hypertension for a number of reasons. These reasons include: 1) the lack of the so-called “white-coat effect”, 2) the ability of the two approaches to provide information on blood pressure phenomena of prognostic value, and 3) the close relationship of the derived values with the risk of developing fatal and non-fatal cardiovascular events. These features also apply to resistant hypertension, in which these approaches allow a precise definition of the diagnosis of this clinical condition, by excluding the presence of white-coat hypertension. Assessment of “out-of-office” blood pressure also allows us to define the patterns of blood pressure variability in this clinical condition as well as its relationships with target organ damage. Finally, home as well as ambulatory blood pressure measurements allow us to investigate the effects of therapeutic interventions, including those associated with the radiofrequency ablation of renal nerves. The present paper will provide a critical review of the main features of home and ambulatory blood pressure measurement in resistant hypertension, highlighting their main advantages as compared to office blood pressure. The prognostic significance, relationships with target organ damage and implications for treatment will also be discussed.
Introduction
Much of the evidence documenting the importance of hypertension as a cardiovascular risk factor as well as the benefits of antihypertensive therapy in decreasing the risk of cardiovascular events has been based on measurement of clinic blood pressure value1. However, there is overwhelming evidence that blood pressure values measured “out-of-office” (ambulatory and home) are also important determinants of cardiovascular risk and that their reduction by antihypertensive treatment may provide a control of the risk profile similar or even superior to the one guaranteed by office blood pressure2-4. Important insights into the clinical value of “out-of-office” blood pressure measurements were achieved in the past two decades from the results of the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) Study, in which office, home, and 24-hour ambulatory blood pressure values were monitored for more than 12 years in about two thousand subjects recruited from the general population living in Monza (Milan, Italy)5-6. In one of the substudies of the PAMELA project it was possible to show that the relationship between blood pressure and cardiovascular mortality is exponential and that the steepest relationship with fatal events is detectable with 24-hour blood pressure, followed by home and then office blood pressure measurements5. Thus, “out-of-office” blood pressure measurements provide complementary prognostic information to office blood pressure. This implies that, while control of office blood pressure is clearly important for decreasing cardiovascular risk, treatment should ideally also be aimed at controlling “out-of-office” blood pressure values.
The present paper will provide a critical review of the position of home and ambulatory blood pressure measurements in resistant hypertension by discussing in sequence three sets of data: first, the importance of “out-of-office” blood pressure in essential hypertension and then, more specifically, in resistant hypertension; second, the role of home and ambulatory blood pressure in defining the patterns of blood pressure variability in this clinical condition; finally, the relevance of these measurements for assessing the effects of therapeutic interventions in resistant hypertensive patients. Over the past two years this last issue has attracted growing interest due to the availability of new non-pharmacological techniques, such as the radiofrequency ablation of renal nerves, capable of lowering elevated blood values in this very high-risk clinical condition.
“Out-of-office” blood pressure measurements in hypertension: general aspects
Self-measurement of blood pressure at home has gained increasing interest in clinical practice for a number of reasons2. First, self-measured blood pressure in the home environment is much less affected by the so-called “white-coat effect” than blood pressure values obtained by a doctor or a nurse in the clinic environment, which is known to be associated with an “alarm reaction” to blood pressure assessment mediated by the sympathetic nervous system7. The lack of this effect makes home blood pressure values closer to the blood pressure load prevailing in daily life. By minimising the highly variable cardiovascular effects of emotion, it also makes it more reproducible than clinic blood pressure, particularly when a suitable number of values are made available, which can be achieved rather easily2. Second, although home blood pressure cannot provide information on blood pressure phenomena of prognostic significance identifiable by ambulatory monitoring (for example, night-time blood pressure fall, short-term blood pressure variability and morning blood pressure rise), its relationship with the risk of cardiovascular morbidity and mortality has been clearly documented in several observational studies2. As already mentioned in the introduction, these studies have also shown that the relationship with cardiovascular risk is steeper for home than for clinic blood pressure5-6. In addition, they have provided conclusive evidence that home blood pressure changes induced by treatment are also prognostically superior to clinic blood pressure changes, at least when prognosis is inferred from the ability to predict the effect of treatment on clinically relevant organ damage such as left ventricular hypertrophy or carotid media-to-intima vascular thickness5,6,8.
During the past twenty years the use of ambulatory blood pressure monitoring has allowed us to gain a large amount of important information on the behaviour of the blood pressure profile over the 24-hour period as well as on the main features of the blood pressure load to the heart during the daytime, night-time or morning hours1,9. Additionally, it has allowed us to determine the superiority of ambulatory blood pressure values as compared to clinic blood pressure in 1) reflecting the hypertension-related end-organ damage and its modifications induced by antihypertensive drug treatment, 2) predicting the development and progression of end-organ damage as well as the occurrence of cardiovascular events both in treated and untreated hypertensive patients, and 3) monitoring the blood pressure lowering effects of a given non-pharmacological or pharmacological intervention in a fashion more accurate and reproducible than the one based on traditional clinic blood pressure measurements1,9. At least two further unique features of the approach deserve to be mentioned. The first one refers to the finding that the technique allows us to gain information on 24-hour blood pressure variability (so-called “short-term” variability) and also its relationships with end-organ damage and cardiovascular events10-14. The second one concerns the usefulness of the approach for the diagnosis of two clinical conditions that were unknown when blood pressure measurements were limited to the clinical environment, namely “white-coat” and “masked” hypertension15.
“Out-of-office” blood pressure measurements in resistant hypertension
Home and ambulatory blood pressure measurements represent important diagnostic tools allowing us to perform a correct diagnosis of true resistant hypertension16-19. Although the definition and diagnosis of this clinical condition are based on clinic blood pressure20, the systematic use of “out-of-office” blood pressure values in patients with uncontrolled blood pressure values and under at least three antihypertensive drugs at full dosage (i.e., the condition recognised as “resistant hypertension”) has allowed us to exclude a consistent number of patients originally labelled as resistant hypertensives. Indeed, these patients showed elevated clinic blood pressure values but normal home and/or 24-hour blood pressure values, and thus they were more properly defined as affected by white-coat hypertension. Threshold values of clinic, home and ambulatory blood pressure for defining hypertension are reported in Table 11. Data from different studies16-19,21, including a recent one from Spain analysing the national data concerning patients with resistant hypertension, showed that one-third of these patients had normal 24-hour ambulatory blood pressure values22 and thus were incorrectly classified as “true” resistant hypertensives. Further, epidemiological insights into resistant hypertension were recently obtained in the context of the Blood Pressure control rate and CArdiovascular Risk profilE (BP-CARE) study, performed in nine central and eastern European countries and aimed at determining the main features of blood pressure control in Eastern Europe23. Indeed, at the initial evaluation based only on clinic blood pressure values, 423 patients of the 7,983 patients originally enrolled in the survey were defined as “apparent” resistant hypertensives24. However, following an accurate assessment of the main patterns of treatment compliance as well as of 24-hour ambulatory blood pressure values, it was possible to define 70 patients as non-compliant, 64 as white-coat hypertensives and 34 concomitantly showing a poor adherence to treatment and a normal 24-hour ambulatory blood pressure profile. Thus, the number of “true” resistant hypertensive patients was about half of the original sample. Similar figures have been reported when home blood pressure measurements are used instead of ambulatory blood pressure values for validating the clinical diagnosis of resistant hypertension based on office blood pressure. This is shown by the results of the large database study “Japan Home versus Office blood pressure Measurement Evaluation (J-HOME)”25,26, which was carried out in 3,400 patients with essential hypertension and under antihypertensive drug treatment. Of the 528 patients under three or more medications potentially affected by resistant hypertension, about 40% were classified as having white-coat hypertension, about 20% as controlled hypertensives and about 40% as sustained resistant hypertensives. Taken together the findings of these two large-scale observational studies provide evidence on the value of ambulatory and home blood pressure measurement in defining “true” resistant hypertension.
The already mentioned PAMELA study, in which clinic, home and ambulatory blood pressure values were concomitantly measured in the same patients, is one of the few investigations available capable of comparing “office” and “out-of-office” blood pressure values in resistant hypertension. About four hundred of the recruited subjects were treated hypertensive patients27. Of these, 84 were controlled hypertensives, 251 were uncontrolled hypertensives and 48 were apparent resistant hypertensives. The behaviour of clinic, home and 24-hour ambulatory blood pressure and heart rate in these three groups are shown in Figure 1. However, when the data derived from home or ambulatory blood pressure monitoring were taken into account for defining “true resistant” hypertension, a much lower number of cases was detected. Indeed, based on home blood pressure values only 38 of the original 48 patients (about 79%) with apparent resistant hypertension displayed elevated home blood pressure, while 10 showed normal “out-of-office” values and were thus identified as white-coat hypertensives (Figure 2). When the data analysis was based on ambulatory blood pressure values, a slightly higher number of patients were detected as white-coat hypertensives and a slightly lower number as true resistant hypertensives (Figure 3). Although the number of cases examined does not allow us to draw any definite conclusion, the above-mentioned data may suggest that ambulatory blood pressure monitoring may provide a more precise definition of resistant hypertensive patients than that obtained by home blood pressure measurements.
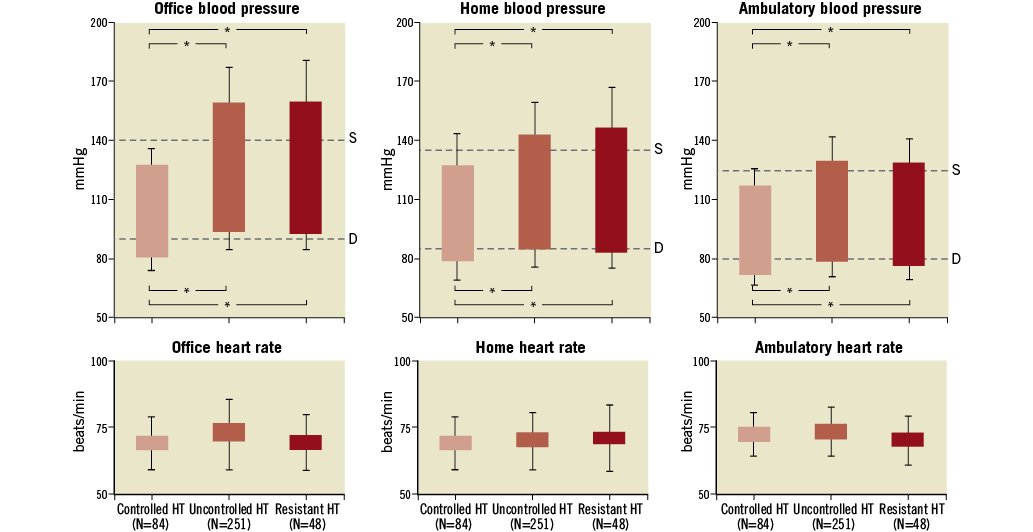
Figure 1. Office, home and ambulatory blood pressure and heart rate (upper and lower panels, respectively) in controlled, uncontrolled and resistant hypertensives (HT). Values are shown as means±standard errors. The definition of resistant hypertension was based on clinic blood pressure. Asterisks refer to the statistical significance between groups (** p<0.01, * p<0.05). S: systolic; D: diastolic
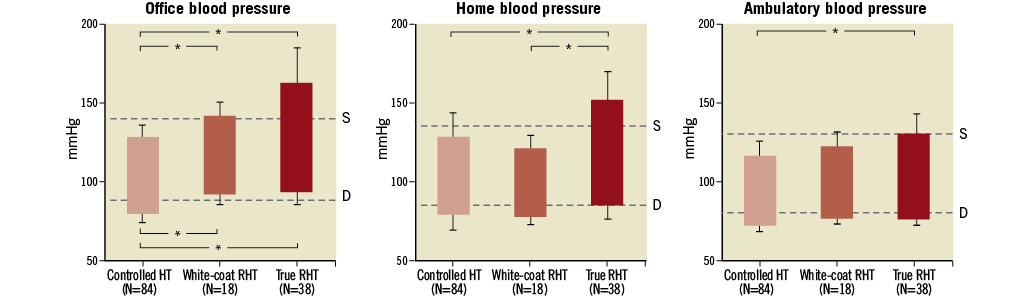
Figure 2. Office, home and ambulatory blood pressure in controlled, white-coat resistant hypertensives (RHT) and true RHT. The definition of resistant hypertension was based on home blood pressure. Values are shown as means±standard errors. Asterisks refer to the statistical significance between groups (* p<0.05). S: systolic; D: diastolic
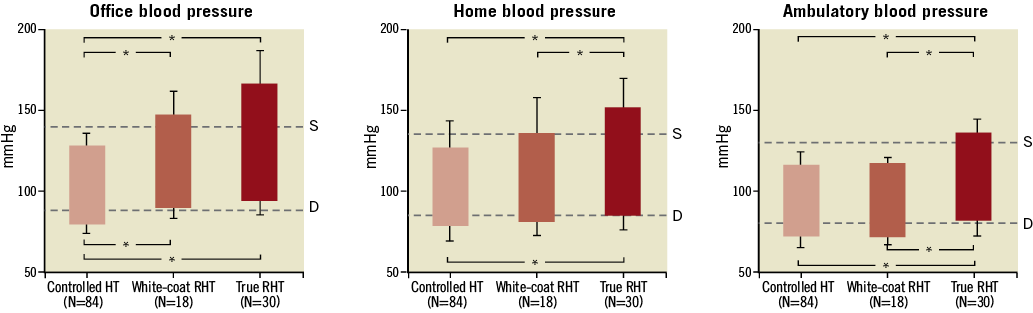
Figure 3. Office, home and ambulatory blood pressure in controlled, white-coat resistant hypertensives (RHT) and true RHT. The definition of resistant hypertension was based on ambulatory blood pressure. Values are shown as means±standard errors. Asterisks refer to the statistical significance between groups (* p<0.05). S: systolic; D: diastolic
Blood pressure variability in resistant hypertension
It has long been known that blood pressure is characterised by an array of spontaneous variations28. That is, blood pressure values vary markedly within a 24-hour period not only because of day/night changes but also because of differences among hours, minutes, and even cardiac beats28. They also show variations over more prolonged periods because of differences among days, months and seasons, with a trend for systolic blood pressure to increase over the years and for diastolic blood pressure to display an age-related biphasic change. Both short-term and long-term values of blood pressure variability are increased in essential hypertensive patients and have prognostic relevance, representing a risk for cardiovascular morbidity and mortality28,29. The evidence so far obtained can be summarised as follows. First, 24-hour blood pressure variability has been shown to relate closely to target organ damage, particularly at cardiac (left ventricular hypertrophy and left ventricular diastolic dysfunction) and vascular (carotid artery thickening and plaques) levels13,28. Second, blood pressure variability is associated with a greater incidence of fatal as well as non-fatal cardiovascular events14,30. Finally, the so-called long-term blood pressure variability, and particularly the recently identified visit-to-visit (day-to-day) blood pressure variability, appears, although not uniformly in the different studies performed so far, to have an important effect on an individual’s long-term risk of cardiovascular events31-33.
The behaviour of blood pressure variability in true resistant hypertension has been investigated in only a few studies. In the case of the already mentioned PAMELA study, we found that systolic blood pressure variability, when expressed as standard deviation of the 24-hour blood pressure values, as variation coefficient (percent values of the standard deviation) or weighted standard deviation (standard deviation which takes into account the day/night blood pressure excursion), was significantly greater in resistant hypertensive patients as compared to the values detected in hypertensive patients controlled or uncontrolled by antihypertensive drugs27. The difference remained significant even after data adjustment for confounders, such as age and 24-hour systolic blood pressure load. Interestingly, the difference in the behaviour of 24-hour systolic blood pressure variability was not paralleled by a similar pattern of diastolic blood pressure variability, whose values were superimposable in the different patient groups.
In the assessment of blood pressure variability, however, a further analysis is represented by the evaluation of the cyclic and residual (or erratic) systo-diastolic components via the Fourier analysis of the 24-hour blood pressure recording. The cyclic components correspond to day/night and pre/postprandial blood pressure difference, while the residual components represent the blood pressure oscillation unexplained by the cyclic components27. The clinical relevance of such blood pressure variations is based on the evidence, again in the PAMELA study, that they have been found to be a potent predictor of fatal cardiovascular events14. As shown in Table 2, the so-called “residual” non-cyclic components appear to be significantly greater in resistant hypertension as compared to what happens in controlled and uncontrolled hypertension34. This potentiation may participate in the increased cardiovascular risk displayed by the resistant hypertensive patients.
Assessment of the blood pressure lowering effects of therapeutic interventions in resistant hypertension
So far, much of the information obtained concerning the blood pressure lowering interventions employed in the treatment of resistant hypertension has largely been based on clinic blood pressure. In the two trials published so far looking at the effects of renal denervation on blood pressure, the Symplicity HTN 1 and 2 trials, the magnitude of the blood pressure fall detected at the 24-hour blood pressure monitoring evaluation was remarkably less (about 30% to 40%) than that seen via clinic blood pressure measurements35,36. This finding is in line with the results of several studies showing that the blood pressure lowering effects of antihypertensive drugs are far less pronounced when evaluated by ambulatory rather by clinic blood pressure measurements. As shown in Figure 4, which is derived from the data presented in a meta-analysis of 44 studies published in the past few years37, the difference between pre-treatment and on-treatment blood pressure values was much less consistent (on average –30%) when based on ambulatory rather than on sphygmomanometric blood pressure measurements. This discrepancy may depend on several factors, including the possibility that, because ambulatory blood pressure monitoring values include night-time blood pressure, which is lower than day-time blood pressure, the difference between pre- and on-treatment values appears smaller than that found with office blood pressure measurements (performed during the daytime). Finally, no study has so far provided any information on the effects of renal denervation on home blood pressure values. In the near future this will be an important area of investigation allowing us to determine the possibility of using home blood pressure as a surrogate of 24-hour ambulatory blood pressure in assessing the blood pressure lowering effects of the intervention.
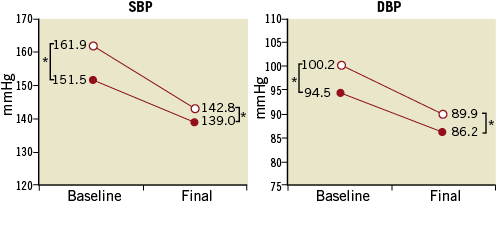
Figure 4. Office (open circles) and ambulatory (closed circles) systolic (SBP) and diastolic (DBP) blood pressure values before (baseline) and during (final) antihypertensive drug treatment. Note the statistically significant difference (*p<0.001) between the values measured in each condition by the two techniques37.
Finally there is some preliminary information on the effects of renal denervation on blood pressure variability. In the only study published so far38, blood pressure variability was assessed as: 1) standard deviation of 24-hour systolic arterial blood pressure; 2) maximum systolic blood pressure; and 3) maximum difference between two consecutive readings of systolic blood pressure over a 24-hour period. Along with the reduction in 24-hour systolic and diastolic blood pressure load, renal denervation triggered a reduction in systolic blood pressure variability in about 90% of the patients, when expressed as standard deviation, maximum systolic blood pressure and maximum systolic blood pressure difference between two readings. However, these data were obtained in a very small group of patients (eleven subjects). Additional studies in larger population samples are therefore called for.
Conclusions
Out-of-office blood pressure measurements represent an important technical advancement in the field of hypertension in general and, specifically, in resistant hypertension. The systematic use of these techniques has allowed an improvement in the diagnostic approach to the resistant hypertensive state and a better definition of the effects of new therapeutic interventions, such as the renal denervation procedure. “Out-of-office” blood pressure measurements have also allowed us to collect information on new cardiovascular risk markers in the resistant hypertensive state, such as blood pressure variability. However, future studies are needed for better definition of the potentials of home and ambulatory blood pressure in this regard.
Conflict of interest statement
The authors have no conflicts of interest to declare.