Abstract
The persistence of high blood pressure under antihypertensive treatment (resistant hypertension) entails an increased cardiovascular risk. It occurs in three of ten treated hypertensive patients, and has several possible contributing factors, notably insufficient therapeutic adherence. There are a number of ways to evaluate whether patients take their medication as prescribed. These include interviewing the patient, pill counting, prescription follow-up, assay of drugs in blood or urine, and use of electronic pill dispensers. None is perfect. However, the essential is to discuss with the patient the importance of complying with the treatment as soon as it is prescribed for the first time, and not waiting for the appearance of resistant hypertension. The measurement of blood pressure outside the medical office and the monitoring of adherence may help to identify patients in whom hypertension is truly resistant and so to tailor the measures required to improve the control of blood pressure in the most appropriate manner.
Introduction
Presently, arterial hypertension is still a major, worldwide public health issue, independent of economic development level1. The lowering of blood pressure through lifestyle modification and the administration of antihypertensive drugs is very efficient at preventing the associated cardiovascular and renal complications. Unfortunately, in spite of the large array of available antihypertensive agents, the control of blood pressure often remains difficult and insufficient in these patients2-6, with important and deleterious consequences on their cardiovascular risk7,8.
According to current guidelines, hypertension is deemed resistant when blood pressure cannot be decreased below 140/90 mmHg despite the administration, at adequate dosage, of at least three drugs, each acting through a different mechanism9,10. Several factors may contribute to this inefficiency. The clinician must exclude a secondary origin11,12, and verify that hypertension is truly resistant, i.e., that blood pressure is high not only in the office but also in daily life13,14. In addition, the possibility that the patient might not take the prescribed medication, or do so only partially, must be considered15.
From treatment initial acceptance to treatment discontinuation
TREATMENT INITIAL ACCEPTANCE
In order to maximise its chances of being accepted, the proposal to start or intensify the antihypertensive treatment must be explained in detail to the patient, who must thoroughly understand the benefits and associated risks16. At this stage, the quality of the patient-doctor relationship is of paramount importance, favouring attendance at follow-up visits, with an expected positive impact on treatment compliance. It is crucial to discuss at this early step the importance of taking the prescribed drugs regularly.
TREATMENT EXECUTION
The patient has accepted the proposed treatment and must now integrate it into his/her daily life, meaning having to take each pill, daily, as prescribed16. The quality of blood pressure control may depend not only on the number of takes, but also on the time interval between them. Ideally, the patient’s compliance to the prescription should be evaluated not only regarding the dosage, but also the timing of drug intake. “Therapeutic compliance” and “adherence” are usual terms to designate the regularity of drug intake, quantified as the percentage of doses taken by the patient in accordance with the recommendations made by the physician. For some authors, adherence, as compared with compliance, is connoted with a more active implication of the patient in his/her treatment17. In general, however, compliance and adherence are considered as synonyms. Another term, although less frequent, is “therapeutic observance”. In the present review, “compliance”, “adherence” and “observance” will be used interchangeably.
Treatment discontinuation
Whether one drug or more than one drug is being used, antihypertensive treatment may be interrupted either on a proposal by the physician or spontaneously by the patient16. The period during which the prescription has been followed is usually designated as “treatment persistence”; it is measured in units of time (days, months or years).
Methods for evaluating therapeutic observance
Unfortunately, there is no ideal method for assessing how regularly patients take their prescribed medication18-20.
REGULARITY OF FOLLOW-UP
The physician may attempt to evaluate the patient’s adherence by considering how regularly he/she shows up at the scheduled follow-up visits. However, this approach is unreliable. For example, some patients may decide to change practitioner, but nevertheless meticulously keep taking their drugs. Indeed, according to the experience accrued by a large clinic specialised in the treatment of hypertension, over a three-year period 25% of patients no longer attended follow-up visits in spite of being sent two reminder letters21.
RESPONSE OF BLOOD PRESSURE
In treated hypertensive patients, the control of blood pressure (or lack thereof) is a poor indicator of therapeutic adherence, because high blood pressure may actually persist even with the regular take of several drugs. This possibility must always be kept in mind when discussing with the patient the possibility of suboptimal compliance.
INTERVIEW
In daily clinical practice, it is simplest to enquire directly about habits regarding compliance. Unfortunately, this approach is quite subjective. Declarations by the patient that pills are being taken very regularly are next to useless, because they cannot be verified. However, if difficulties in this area are spontaneously acknowledged, the physician can take action in order to help22,23. It may be worthwhile to use a simple questionnaire focused on adherence24. Overall, adherence will tend to be overestimated if evaluated solely on the basis of declarations made by the patient25.
PILL COUNTING
In clinical drug trials, pill counting is traditionally considered an objective way of evaluating therapeutic adherence. However, this method is not optimal because some patients will throw away the unused doses before returning the container26. It appears that, when evaluated by pill counting, adherence must exceed 80% in order for a significant drop in blood pressure to be observed27.
ASSAYS FOR DRUGS OR CHEMICAL MARKERS
Adherence to the prescription of some drugs may be evaluated by assaying their level, or that of metabolites in blood or urine. Analysis may also be carried out on chemical markers prescribed in association with the drug and easily assayed in biological fluids. Because they are objective, these methods are attractive. Unfortunately, large-scale application meets with difficulties related to the complexity and cost of some of these laboratory procedures. In addition, assays carried out at a single time point will not tell whether the patient took the medication only in the days preceding sample collection28.
PRESCRIPTION FOLLOW-UP
Prescription follow-up offers an indirect estimation of therapeutic compliance. Quite simply, when writing down a new prescription, the physician looks up the date of the previous one and checks whether the amount of drug mentioned thereon covered the patient’s needs for the elapsed time. Prescription follow-up can possibly be carried out by the pharmacist, or by the insurance companies which keep records on the prescriptions received by all their affiliates29. This latter approach is often used for evaluating persistence regarding a specific regimen in groups of patients30,31, but it does not inform on day-to-day compliance.
ELECTRONIC PILL DISPENSER
Recording each opening of a pill container over weeks or months provides an accurate knowledge on the regularity of drug intake. Useful information is also provided by the timing of successive accesses to the container, making it possible in some cases to adapt the treatment and improve its efficiency over 24 hours. The recording provides an objective basis to discuss the patient’s difficulties with therapeutic adherence, making it easier to propose corrective measures32-34. Importantly, the patient requires instructions on how to use the device, and on its purpose. The opportunity then provided to discuss therapeutic adherence may have a long-lasting positive effect. However, one should remember that, in order to interpret the data in terms of drug intake, one has to assume that the patient has actually ingested the dispensed pill rather than thrown it into the rubbish bin. Also, the device is costly and, when several drugs are being prescribed, one separate dispenser for each is ideally required.
Therapeutic adherence and resistant hypertension
Without doubt, blood pressure control remains insufficient worldwide2-6. Too many patients do not know that they are hypertensive, and blood pressure remains abnormally high in too many treated patients. Among the latter, hypertension is apparently resistant (apparent resistant hypertension) according to the following definition: either a) a blood pressure ≥140/90 mmHg despite the intake of at least three different antihypertensive drugs from different therapeutic classes, with at least one diuretic, or b) the intake of ≥4 antihypertensive drugs, irrespective of blood pressure level with such treatment. This definition of apparent resistant hypertension has been proposed by the American Heart Association11. According to the ESH/ESC hypertension guidelines, however, resistant hypertension refers to the persistence of high blood pressure (>140/90 mmHg) despite the intake of 3 antihypertensive agents, one of them being a diuretic4. The prevalence of resistant hypertension is difficult to assess, because this requires the collection of precise data, in standardised conditions, in large cohorts. In that respect, observations made in the United States in the course of the National Health and Nutrition Examination Surveys give a fair indication of what may be expected in industrialised countries2. Hypertension turned out to be resistant in 28% of treated hypertensive patients, and 11.8% of all participants. However, therapeutic adherence was not evaluated in this study.
Very recently, the possible relationship between poor therapeutic compliance and the prevalence of apparently resistant hypertension was studied in 4,046 hypertensive patients, who originated from 48 states in the continental USA, aged 45 years or more, and receiving ≥3 antihypertensive agents35. This study is interesting mostly because telephone interviews of patients were carried out and focused on observance by means of the Morisky Medication Adherence Scale (MMAS), a questionnaire comprising the following four items24:
1) Do you ever forget to take medications?
2) Are you ever careless in taking your medications?
3) Do you ever miss taking your medications when you are feeling better?
4) Do you ever miss taking any of your medications because you are feeling sick? Each positive answer is counted as one point, and a total score of four points represents the worst observance36. As shown in Figure 1, the prevalence of good blood pressure control decreased from 46.8% in patients presumed to be taking their medication with the greatest regularity to 27.2% in those who complied least.

Figure 1. Relationship between the rate of blood pressure control and the level of adherence to treatment35.
Another very recent study demonstrated that poor observance is the main cause of resistant hypertension, indeed twice as frequent in comparison with secondary hypertension37. In spite of its small size (n=108), this study is very interesting, because the resistant character of hypertension was documented not only in the office (office BP ≥140/90 mmHg) but also with ambulatory blood pressure monitoring (24 hr mean systolic/diastolic BP ≥130/80 mmHg). Of these 108 patients, hypertension was secondary in 15, and blood pressure normalised with treatment intensification in 17. In the remaining 76, blood pressure was persistently uncontrolled despite the prescription and – according to patient’s declaration – regular intake of ≥4 antihypertensive agents. The main originality of this work resides in the fact that the presence of antihypertensive drugs was assayed in the urine of these 76 patients, without informing them that compliance was being investigated. The analyses were carried out with high performance liquid chromatography-mass spectrometry, a method able to detect all prescribed agents except lercanidipine (received by 17 patients) and nitrates (received by three). Patients were considered adherent if all prescribed drugs were detected, which happened in only 36 of them (47.4%), the other 40 (52.6%) thus being non-compliant. No drugs at all were recovered in 12 of these 40 subjects (30%), while non-compliance was less severe in the remaining 28 (70%), as illustrated in Figure 2. Interestingly, most patients identified as non-compliant acknowledged, once informed of the analysis results, that they had taken their prescribed medication irregularly or not at all. These data show that resistant hypertension is often associated with poor adherence, even when the patient declares that his/her medication is being taken regularly.

Figure 2. Fractions of non-adherent patients ranked according to the percentage of prescribed antihypertensive drugs detected in urine37.
Improving blood pressure control by improving adherence
In hypertensive patients, therapeutic adherence may be improved through several approaches17, ranging from educational measures to behavioural interventions aimed at overcoming the patient’s resistance to treatment or support measures designed to facilitate regular drug intake. In fact, strategies must be combined for maximal efficacy.
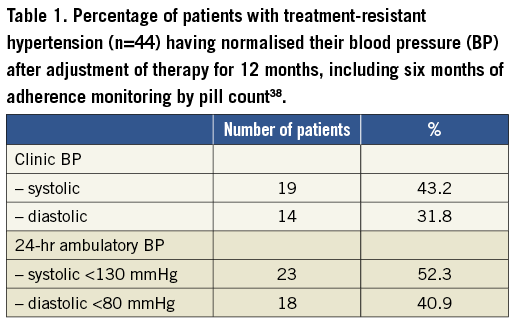
With resistant hypertension, the long-term monitoring of therapeutic adherence has a positive impact on blood pressure. One study carried out in a specialised hypertension clinic enrolled 44 patients referred for persistently high blood pressure (≥140/90 mmHg) despite the prescription of three agents38. These patients were followed for one year, not only with measurements of office blood pressure, but also with 24-hour ambulatory blood pressure monitoring at inclusion in the study, then six and 12 months later. During the whole follow-up, treatment was adjusted with the aim of normalising office blood pressure (<140/90 mmHg). From the sixth month on, compliance was assessed by pill counting. Furthermore, the patients were asked to complete the Morisky questionnaire24 at the beginning and at the end of the adherence monitoring period. On the first return of drugs in the course of the monitoring period, 29 patients (63.6%) were considered adherent based on having consumed (i.e., not returned) ≥80% of doses. This figure increased to 35 (79.5%) at the end of the study. An improvement in adherence was concomitantly supported by the outcome of the Morisky questionnaire, with the maximal score observed in 30 patients (68.2%) at the end of the study, versus 16 (36.4%) six months before. Table 1 shows the percentage of patients who normalised their systolic and diastolic blood pressure in the course of the study.
In another study of 41 patients with resistant hypertension, observance was monitored objectively with pill counting for two months without any change brought to the therapeutic regimen39. Blood pressure decreased significantly (p<0.01) from 156/106 to 146/99 mmHg after the first month, and to 146/97 mmHg after the second one. In the study period, the take of drug was excellent, with the rate of dispenser opening matching on average the prescription in 93% of cases. Overall, systolic pressure normalised (<140 mmHg) in 32% of the patients, and the corresponding figure for diastolic pressure (<90 mmHg) was 34%.
In short, the monitoring of adherence appears to be a useful measure for improving the control of blood pressure in resistant hypertension. Of note, however, blood pressure cannot be normalised in many patients with resistant hypertension, however hard the attempts to improve their therapeutic observance. The practitioner must remember that blood pressure may remain high even when the patient scrupulously abides by the prescribed treatment.
Conclusions
When confronted with resistant hypertension, the practitioner must think of several possible causes, ranging from secondary hypertension to white-coat hypertension and insufficient therapeutic observance. There are several methods to search for irregular drug intake, each with advantages and drawbacks. In practice, it is essential to discuss the importance of observance as soon as an antihypertensive treatment is prescribed, without waiting for the failure to reach the therapeutic objectives. It must also be remembered that such failure is not necessarily synonymous with poor therapeutic observance.
Conflict of interest statement
The authors have no conflicts of interest to declare.

