Futility or lack of improvement in quality of life and survival after transcatheter aortic valve implantation (TAVI) procedures is a subject of major interest1,2. One reason why patients may not benefit fully from treatment is frailty. Frailty is a relatively common condition among elderly patients undergoing TAVI and is associated with an increased risk of adverse outcome3. Frailty is a multidimensional geriatric syndrome characterised by a decline in overall function and loss of resistance to stressors. It is associated with increased morbidity, intensification of healthcare utilisation, and mortality among older adults4,5. Frail patients are prone to poor outcomes and high mortality, procedural complications, prolonged recovery and functional decline6. A recent systematic review demonstrated a relationship between preoperative frailty and outcomes following TAVI, with a mortality rate of 34 deaths per 100 patients annually in frail individuals undergoing TAVI compared with 19 deaths per 100 patients annually in non-frail patients3.
The surgical risk scores commonly used to estimate perioperative morbidity and mortality in coronary heart surgery may not be ideally suited to predicting the real operative risk in patients undergoing TAVI. These scores are based on overall assessment of age and comorbidities and have not been designed for or tested in elderly patients being considered for TAVI7,8. By omitting an assessment of frailty, such scores are not always able to identify patients who are likely to benefit in terms of both survival and quality of life after TAVI6.
Both European and US guidelines recommend the assessment of frailty evaluating cognition and physical function using validated checklists9,10. Although multiple studies have shown the importance of frailty, there is a lack of consensus regarding the optimum method to measure it. The lack of a clear and objective evaluation of frailty is a major barrier limiting its use and the reason for the different rates of prevalence reported across various studies11 (Figure 1). To date, the frailty indices most commonly used in clinical evaluation of patients with aortic stenosis are the Katz Index, elderly mobility scale, Canadian Study of Health and Aging, five-metre walking test and hand grip strength test which measure mobility, strength, nutritional status and habitual activity6. However, limited data are available on which of these tests best predicts clinical outcomes in vulnerable patients.
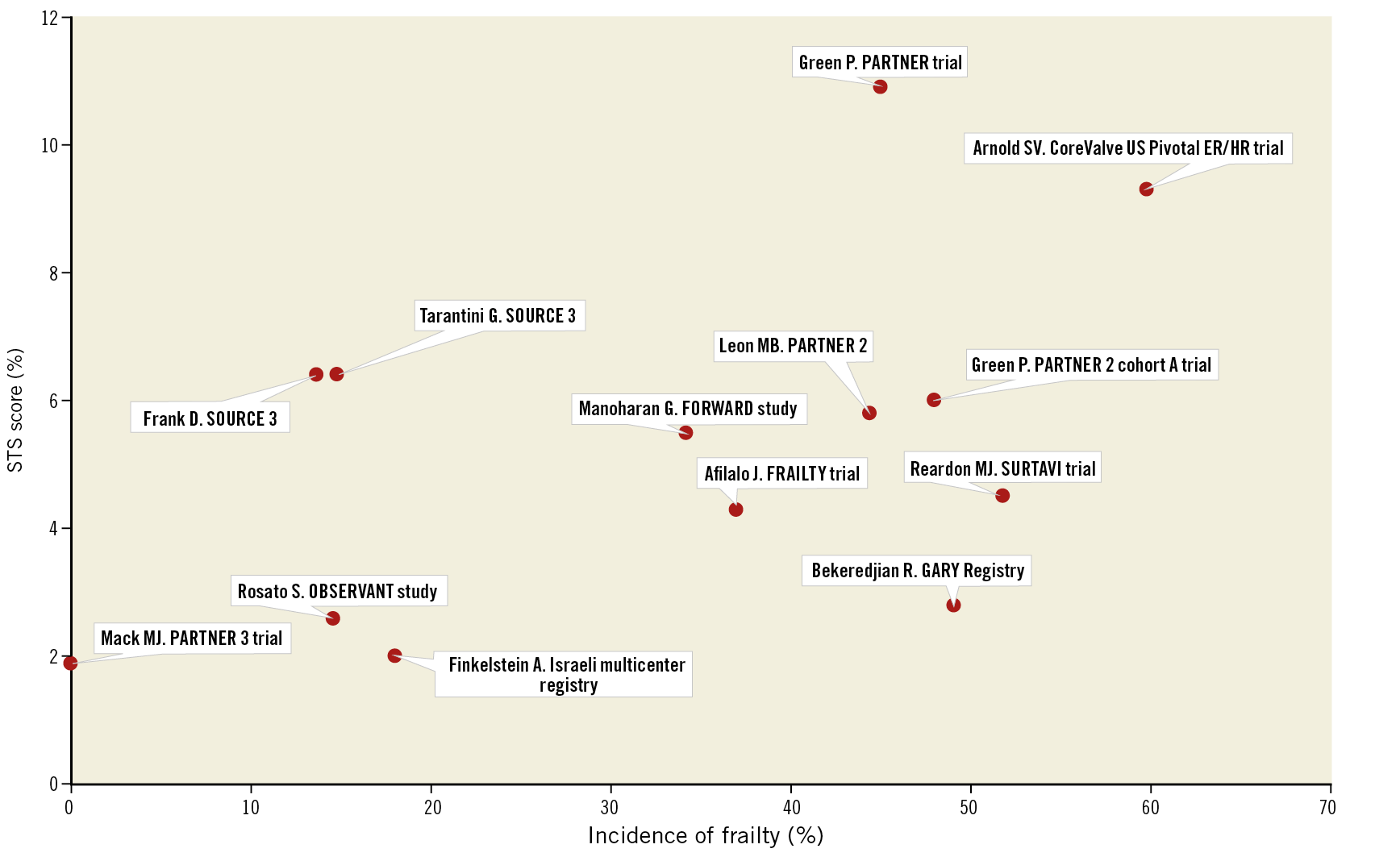
Figure 1. Incidence of frailty according to STS score across studies. The wide variability in the prevalence of frailty across the spectrum of surgical risk scores may be due to the different methods used to measure frailty in individual studies.
In the FRAILTY-AVR (Frailty Assessment Before Cardiac Surgery & Transcatheter Interventions) prospective study, the investigators evaluated the incremental value of seven different frailty scales to a standard risk algorithm in predicting poor outcomes following TAVI and surgical aortic valve replacement (SAVR)11. The authors found that within the same cohort of patients the prevalence of frailty ranged from 26% to 68%, depending on the score used. Moreover, among the scores tested, the Essential Frailty Toolset (one of the seven frailty scales compared in the FRAILTY study) was the strongest predictor of death and worsening disability at one year in patients undergoing both TAVI and SAVR. Recently, Skaar et al developed a novel eight-element frailty score – incorporating comprehensive geriatric assessment – able to identify patients less likely to benefit from TAVI. According to this study, a frailty score ≥4 could identify patients with a high two-year mortality after TAVI12.
Most available data about frailty among TAVI candidates refer to high/intermediate surgical risk patients13,14,15,16. In low surgical risk patients, data about frailty are somewhat confusing17,18. Randomised clinical trials such as the NOTION trial and the Evolut Low Risk trial did not measure the prevalence of frailty among low surgical risk patients19,20. In other trials, such as the multicentre United States trial, frail patients were excluded at screening21. Furthermore, a sub-analysis of studies which focused on low-risk patients discovered a high prevalence of frailty among these patients (up to almost 50%), presumably because they underwent TAVI instead of SAVR, due to their frailty status22.
On the spectrum of the frailty syndrome, part of this intricate “mosaic” is sarcopaenia, defined by the European Working Group on Sarcopenia in Older People (EWGSOP) as a progressive and generalised muscle disorder characterised by adverse muscle changes across a lifetime with low muscle quantity and quality, ending in muscle failure and associated with increased likelihood of adverse outcomes including falls, fractures, physical disability and mortality5. The physical phenotype of frailty shows significant overlap with sarcopaenia: low grip strength and slow gait speed are characteristic of both. Sarcopaenia is common among adults of older age but can also occur earlier in life.
Severe sarcopaenia is diagnosed when all of the following features are detected together: low muscle strength, low muscle quantity/quality, and low physical performance. Magnetic resonance imaging (MRI) and computed tomography (CT) are the gold standard for a non-invasive evaluation of muscle quantity/mass5. In particular, measurement of muscle mass using a CT scan at the level of the L3 vertebra has been correlated with long-term mortality in patients treated with TAVI6. Kleczynski et al evaluated the value of psoas muscle area and psoas muscle volume measured with a validated CT method to predict long-term mortality in patients who underwent TAVI6. Interestingly, both psoas muscle area and psoas muscle volume values normalised for body surface area (BSA) had the highest discrimination ability among all the tested frailty scores in the receiver operating characteristic analysis for 12-month all-cause mortality.
In the current issue of EuroIntervention, Heidari et al compared in-hospital adverse outcomes and overall mortality in sarcopaenic and non-sarcopaenic patients undergoing TAVI23.
Although sarcopaenia was found to be an independent predictor of midterm mortality, sarcopaenic patients had similar in-hospital clinical outcomes to non-sarcopaenic patients, suggesting the appropriateness of TAVI treatment in these patients. According to these results, the authors proposed a systematic evaluation of sarcopaenia using a CT scan prior to TAVI in order to decide the best treatment pathway, identifying patients who may benefit from additional nutritional support, cardiac rehabilitation or an exercise programme. Moreover, compared to the case of overall frailty, diagnosing sarcopaenia with a CT scan is an objective method that is available in all centres without substantial additional resources.
The presence of sarcopaenia has proven to be important for risk assessment in many other clinical settings and it is worth underlining that sarcopaenia often coexists with obesity (usually defined as body mass index [BMI] ≥30 kg/m2). Sarcopaenic obesity is high adiposity coupled with low muscle mass and seems to be associated with higher levels of metabolic disorders and increased risk of mortality than simple obesity or sarcopaenia alone24.
So, can we rely on sarcopaenia alone for risk assessment or is it only one important piece of our puzzle? We believe that, in patients at risk of frailty, screening with multifactorial evaluation supported by prudent use of clinical and imaging resources is the best approach. This offers the opportunity both to assess suitability for and appropriateness of treatment and to plan the optimal periprocedural and post-procedural care to ensure the best possible outcomes. Ideally, we should understand when we need to set up a specific and tailored programme for our patients and consider special rehabilitation and nutritional programmes in these vulnerable patients23.
Nowadays, TAVI is a well accepted alternative for treating patients across the spectrum of surgical risk. The expansion of TAVI indications, as well as the ageing of the population, will lead to an increase in the number of TAVI procedures performed in the coming decades25,26. Hence, there is a need for a simplified and fast-track TAVI approach with the aim of an earlier discharge. A multiparametric evaluation and assessment of frailty is essential because frail patients are frequently encountered. In order to improve TAVI outcomes, it is essential to identify the patient’s profile for the best management, reduced duration of hospitalisation, and reduction of costs, without compromising the safety and the efficacy of the procedure. Systematic use of multidisciplinary evaluation can guide us towards the best care pathway for the individual patients we treat.
Conflict of interest statement
A. S. Petronio is a consultant to and has received research funding from Medtronic, Boston Scientific, Abbott and GADA. C. Giannini has no conflicts of interest to declare.