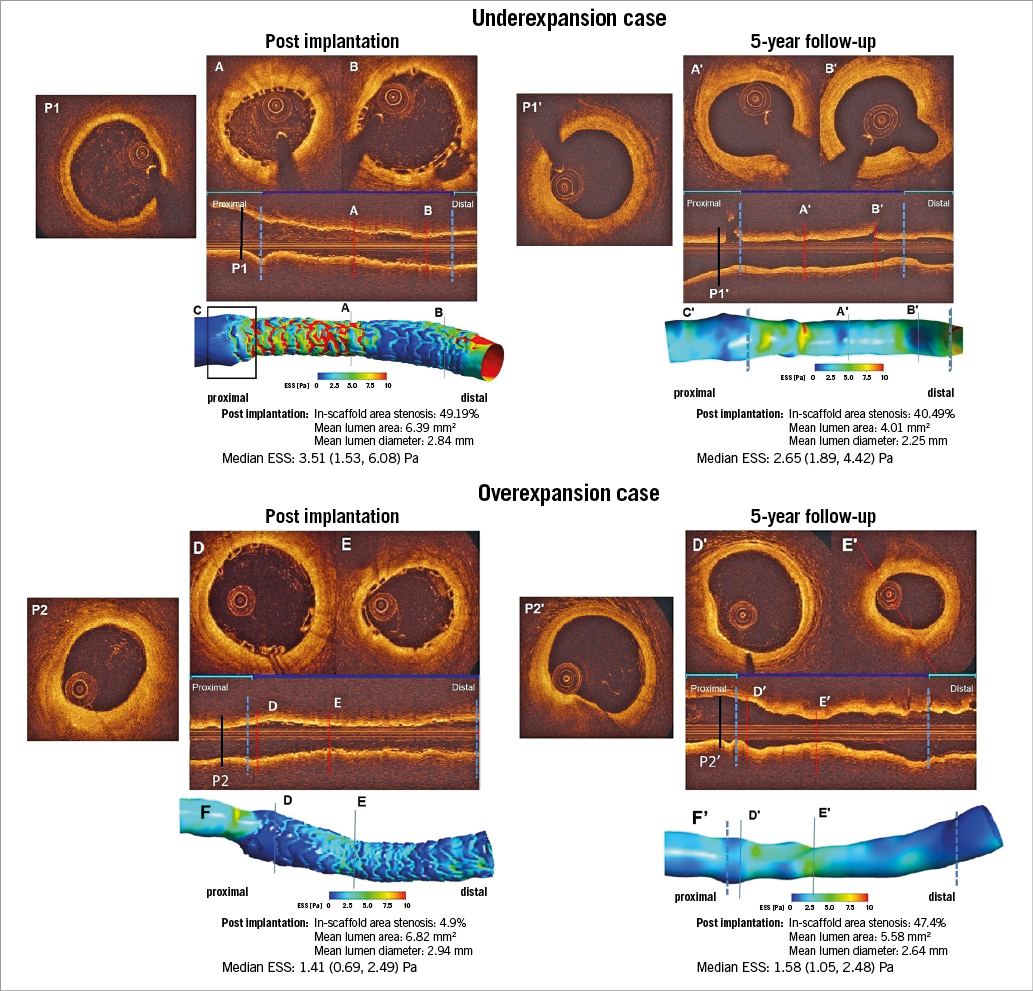
Two patients received 3.0×18 mm Absorb™ bioresorbable vascular scaffolds (Abbott Vascular, Santa Clara, CA, USA), one in the left anterior descending coronary artery, the other in the circumflex coronary artery. Post-implantation OCT (pullback speed: 20 mm/s, acquisition rate: 200 frames/s) and angiographic data were fused to reconstruct the coronary anatomy, and computational fluid dynamic (CFD) techniques were used to simulate Newtonian steady blood flow and estimate endothelial shear stress (ESS) distributions1. Panels A, B, C & P1 show underexpansion of the scaffold (mean expansion index: 0.51). Panels D, E, F & P2 show an overexpanded bioresorbable scaffold (mean expansion index: 1.32).
In the CFD model of the underexpanded case (Panel C), high ESS (in red) was noted on top of the struts which disrupted the flow, creating recirculation zones and low ESS (in dark blue) in the inter-strut zones. Scaffold underexpansion caused a “step-down” at the proximal edge of the scaffolded segment (Panel P1, black box in Panel C). On the five-year OCT, there was attenuation of the step-down appearance with normalised ESS in the proximal edge segment (Panels A’, B’ , C’ & P1’); the luminal surface was smoother and overall the shear stress was more homogeneous and physiological (1.5-3.0 Pa).
In the CFD model of the overexpanded case, low ESS was detected not only in the inter-strut areas but also on top of the struts. Scaffold overexpansion caused a “step-up” at the proximal edge of the scaffolded segment. At the five-year follow-up, the step-up became less prominent and the areas of very low shear stress regressed considerably (Panels D’, E’, F’ & P2’).
These two cases of overexpansion and underexpansion at baseline resulted acutely in two different shear stress distributions. Both increased and decreased ESS appear to induce a biological mechano-transduction process that aims at normalising ESS levels at long-term follow-up to values close to the physiological ranges (1.5-2.5 Pa). The mechanism of “normalisation” seems to be related to a dynamic remodelling, which presumably resulted from shear stress, wall stress, cyclic strain and other important biologic factors2,3.
Practical implication
Underexpansion and overexpansion have been incriminated as causative factors of adverse cardiac events. However, dynamic biological interaction between vessel wall and scaffold may attenuate the adverse haemodynamic impact of overexpansion or underexpansion.
Guest Editor
This paper was guest edited by Lorenz Räber, MD, PhD; Department of Cardiology, Swiss Cardiovascular Center, University Hospital Bern, Switzerland.
Conflict of interest statement
P.W. Serruys and Y. Onuma are members of the International Advisory Board of Abbott Vascular. The other authors have no conflicts of interest to declare. The Guest Editor has no conflicts of interest to declare.