- renal denervation
- resistant hypertension
- transulnar
Abstract
Renal denervation (RDN) has been shown to be safe and efficacious in reducing blood pressure in patients with resistant hypertension. In the present study, we describe a first-in-man report of the Iberis renal denervation device in a patient who underwent two RDN procedures: one via the femoral artery and one via the transulnar approach. RDN was performed in the patient’s right renal artery using an Iberis catheter via the transulnar approach, as the transfemoral or transradial arteries could not be approached due to their anatomic constraints. In summary, RDN via the transulnar approach is feasible and represents a technical alternative solution in certain patients.
Introduction
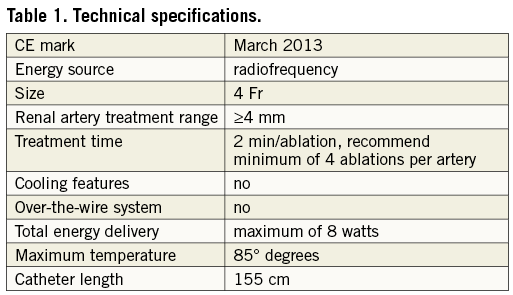
We describe a successful first-in-man case of transulnar renal denervation (RDN) for resistant hypertension using a 155 cm radiofrequency ablation catheter (Iberis™; Shanghai AngioCare Medical Technology, Shanghai, China). The Iberis renal sympathetic denervation system includes a generator and a 4 Fr compatible catheter with single-use radiofrequency probe. Energy is delivered to the renal arterial wall from a monopolar platinum electrode located at the distal tip of the catheter. The system received CE-mark approval in March 2013 (Table 1). The patient was enrolled in the ongoing first-in-man study. In addition, the pivotal trial has been designed to evaluate the effectiveness of the device in a multicentre randomised trial in China.
Case report
A 38-year-old man (height 172 cm, weight 74 kg) with a primary complaint of recurrent dizziness was admitted to our hospital for examination and treatment. The patient had experienced medically resistant hypertension for more than two years despite treatment with four antihypertensive drugs (valsartan 80 mg/day, amlodipine 10 mg/day, metoprolol 100 mg/day, hydrochlorothiazide 25 mg/day). The patient also had left ventricular hypertrophy (left ventricular mass index 132 g/m2) with an ejection fraction of 65%. Renal function was slightly abnormal with microalbuminuria (223.1 mg/L) and estimated glomerular filtration rate of 67.4 ml/min/1.73 m2. Secondary causes of hypertension were excluded.
The mean home and office-based blood pressure was consistently above 160/95 mmHg and mean 24-hour ambulatory blood pressure monitoring (ABPM) was 172/111 mmHg (diurnal 180/117 mmHg, nocturnal 157/100 mmHg) together with administration of antihypertensive medications. Given the uncontrolled nature of the patient’s resistant hypertension and sustained progression of target organ damage, the patient had a clinical indication for RDN1. Computed tomography angiography was performed to evaluate renal artery anatomy. There was no evidence of dual or multiple renal arteries, severe renal artery stenosis, or renal aneurysm. Both renal arteries had a length of >20 mm and lumen diameter of >4 mm. However, the right renal-aorto angle was very acute (almost 0 degrees). The patient underwent RDN via right femoral access according to the procedure described by the Symplicity investigators1. Six ablations were successfully performed, using a 105 cm Iberis catheter in the left renal artery. However, the ablation catheter could not engage into the right renal artery and no ablations were performed in this artery.
Ten days after the left renal artery RDN, mean home-based blood pressure was 150/85 mmHg. Given the availability of a longer radiofrequency ablation catheter at the time the patient returned for follow-up, the patient was scheduled for RDN of the right renal artery via radial access. Under local anaesthesia, a 6 Fr introducer sheath was inserted into the right radial artery. Heparin, 3,000 units, was administered intravenously. A 0.035 inch HiWire® angled hydrophilic guidewire (Cook Medical, Bloomington, IN, USA) could not be advanced past the elbow level. Forearm angiography was performed revealing severe tortuosity of the radial artery. The deep palmar arch supplied by the ulnar artery was clearly visible while there was no flow in the radial artery distal to the sheath. The operator decided to switch the access site to the ulnar artery. Puncture and cannulation of the ulnar artery were successful. An angiogram of the wrist showed that the interosseous artery had scant flow to the hand while the ulnar artery had adequate blood supply to maintain the right hand (Figure 1).
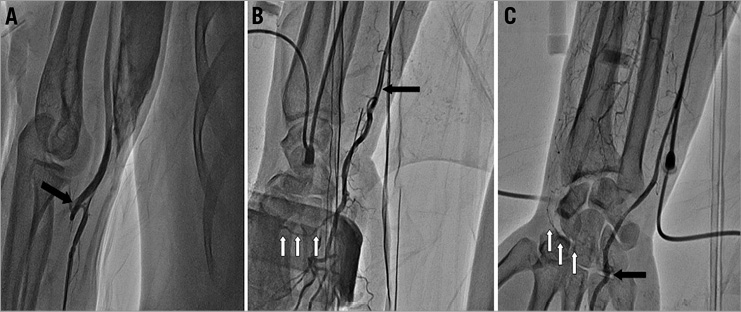
Figure 1. Forearm angiography. A) Forearm angiography showed severe tortuosity of the radial artery at the elbow level (black arrow); B) a large ulnar artery (black arrow) and the deep palmar arch supplied by ulnar artery (white arrow); and C) scant flow of the interosseous artery (white arrow) and adequate flow of ulnar artery (black arrow) to the hand, respectively.
The ablation catheter was inserted into the right renal artery. Eight ablations (8 watts or less, up to 120 seconds for each ablation) were performed. An angiogram of the right renal artery post-ablation was unremarkable (Figure 2). The patient was discharged on the second postoperative day.
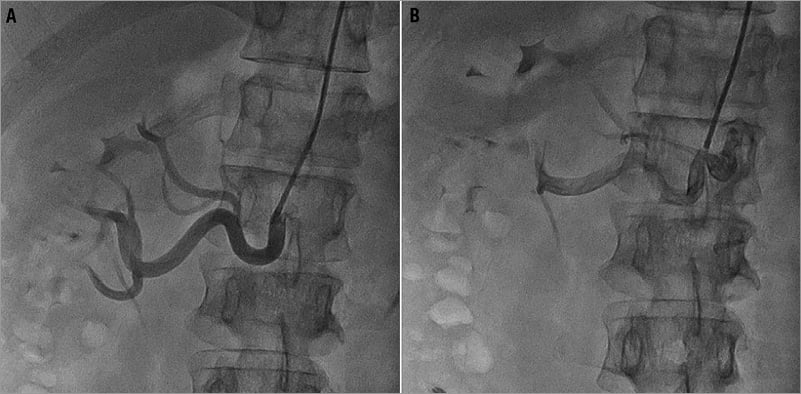
Figure 2. Renal artery angiography. Renal artery angiography before A) and after B) renal nerve ablation showed no anatomical abnormality in the right renal artery through the forearm approach.
At follow-up examination one month after the second RDN, the mean home-based blood pressure was 135/80 mmHg and mean 24-hour ABPM was 132/80 mmHg (diurnal 141/87 mmHg, nocturnal 127/74 mmHg).
Discussion
RDN is a promising device-based intervention for resistant hypertension1,2. This successful case demonstrates the feasibility of the transulnar access to perform RDN. Apart from the availability of this novel longer ablation catheter with its good flexibility, we believe the following points may be critical to perform RDN successfully via forearm access. First, good coaxiality between the guiding catheter and the renal artery is needed to steer the ablation catheter properly3,4. Second, a “curved-tip” shape to the distal portion of the ablation catheter to balance the motion of catheter tip derived from respiration is required. With strict implementation of these two points in the present case, the ablation electrode maintained vessel wall contact for 120 seconds in each ablation. In summary, with the availability of longer ablation catheters, forearm access is an alternative approach for RDN.
Acknowledgement
We are grateful to Dr Yao-Jun Zhang for his advice concerning the preparation of this manuscript.
Conflict of interest statement
The authors have no conflicts of interest to declare.