Introduction
Increased procedural safety and improved patient comfort are the two key advantages of the transradial approach (TRA) over traditional femoral access (FA)1, which has led to its growing popularity2,3. While the favourable safety profile of the TRA is reflected in the high-level recommendations for its use in cardiology, the relatively high rate of radial artery occlusions (RAO) remains an important concern4. The distal transradial approach (DTRA) was developed to address the issue of RAO without compromising efficacy or patient comfort.
Encouraged by the initial data published on the DTRA for percutaneous coronary interventions (PCI)5, we decided to test its feasibility for carotid interventions in an all-comer population using a sheathless coronary guiding system, as a continuation of our previous research work in the application of TRA for carotid artery stenting (CAS)6. To our knowledge, this is the first report on the use of DTRA for the treatment of carotid artery disease.
Methods
STUDY POPULATION AND OUTCOME MEASURES
Two hundred and nine consecutive CAS cases with high risk for surgery were evaluated. Fifty-eight patients were treated using the DTRA between January and September 2018, while the control group consisted of 151 conventional TRA CAS patients treated between January 2016 and December 2017. The procedures were performed by three skilled operators.
Major adverse cardiac and cerebral events (MACCE), major and minor access-site complications, and the procedural data were compared between the non-randomised study groups according to the methods of the RADCAR study6. The ethics committee approved the investigations.
CAS PROCEDURES
TRA cases were performed according to our published protocol following a positive Allen test6. All DTRA cannulations were performed with ultrasonography guidance (Vivid-I; General Electric, Boston, MA, USA) (Figure 1) using 4-5 Fr transradial sheaths (Terumo Corp., Tokyo, Japan). After an exchange manoeuvre, the carotid artery was accessed by 6.5 Fr JR5 sheathless guiding (SG) (Asahi Intecc, Aichi, Japan). In complex aortic arches, a 125 cm long multipurpose catheter was applied to prevent SG protrusion into the aorta. A filter wire was used in all cases. As proximal embolic protection cannot be applied to prevent embolisation, dual layer stents were more frequently implanted using the DTRA (48.28% vs 30.46%, p=0.023). The Seal-One® haemostatic device (Perouse Medical, Ivry-le-Temple, France) was used for compression. The follow-up included clinical examinations during the hospital stay and at one month. All DTRA patients and TRA patients without a palpable radial artery (RA) underwent control ultrasound (US).
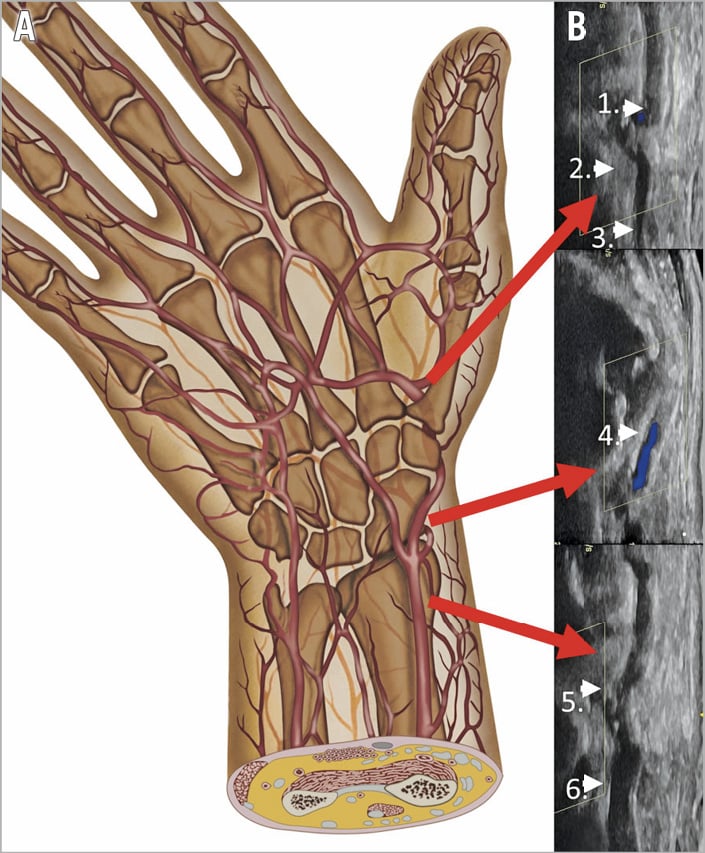
Figure 1. Vascular anatomy of the “snuffbox area”. Anatomic drawing of the right hand (A) with the corresponding vascular ultrasound image of the radial artery (B). The usual puncture site of the radial artery is shown at the wrist level (6). Above it lies the origin of the superficial palmar arch (5). The optimal puncture point for the DTRA is in the descending section of the artery underneath the snuffbox area (4). Distally, the ascending section of the distal radial artery (3), the origin of the deep palmar arch (2) and the princeps pollicis artery (1) can be identified.
Results
Baseline clinical characteristics were similar across treatment groups, except for the significant difference in symptomatic presentations (DTRA: 75.86% vs TRA: 46.36%, p<0.001). Procedural success from the primary access was achieved in all patients in the DTRA group and in 94% of the TRA cohort (p=0.065). We found no statistically significant difference in the safety and efficacy of the two access sites, and no transient neurological deficit or stroke was documented. A major access-site complication was encountered in one patient (1.72%; 1/58) in the DTRA group (an arterioventricular [AV] fistula requiring surgical reconstruction), while only asymptomatic RAOs occurred in the TRA group (3.31%; 5/151).
The overall procedure length (p<0.001) and fluoroscopy times (p=0.005) were higher for DTRA, while the contrast consumption (p=0.912), cumulative X-ray dose (p=0.811) and the length of hospital stay were similar (Figure 2).
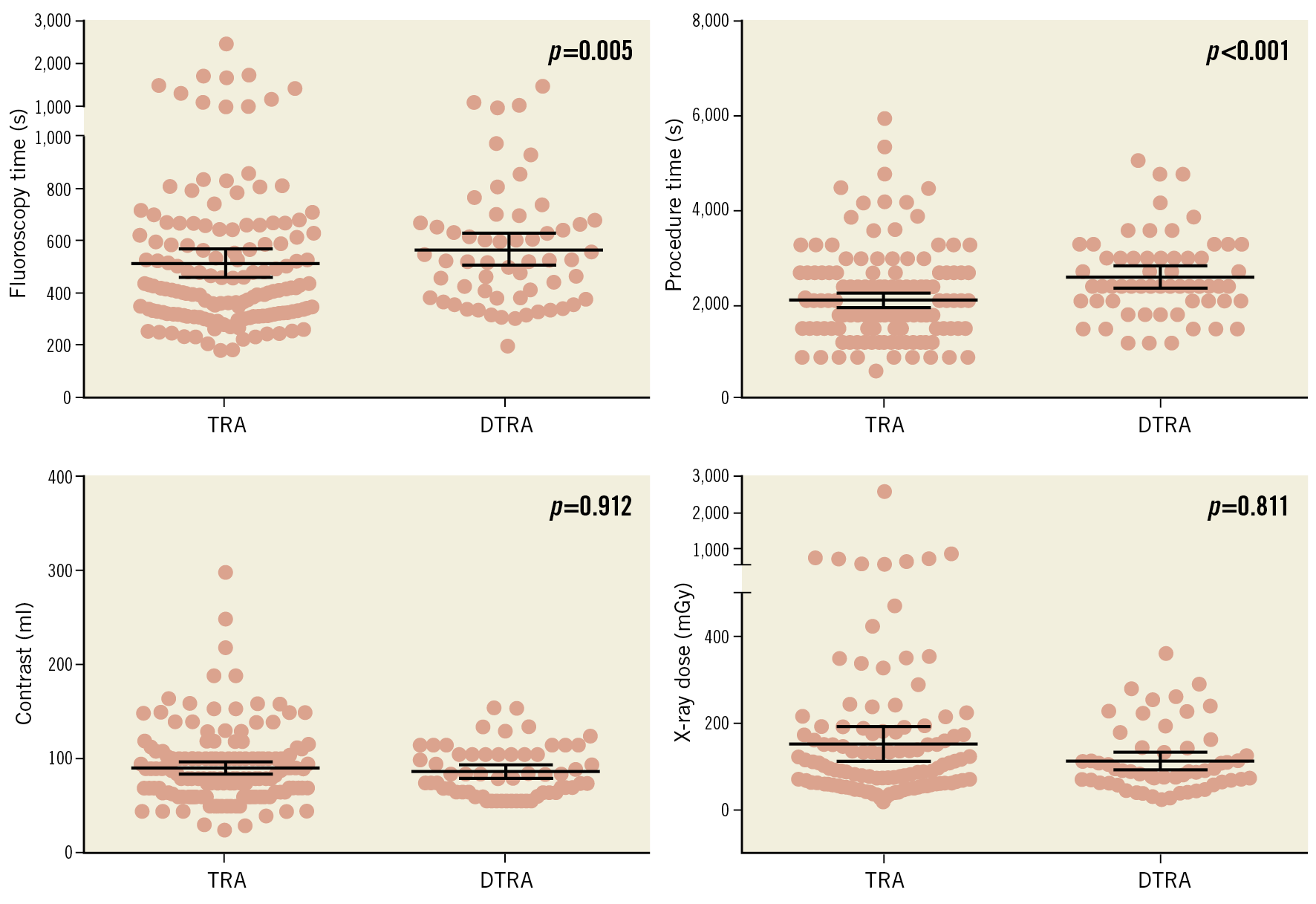
Figure 2. Comparative analysis of the procedural data for CAS using DTRA and TRA. Fluoroscopy (A) and procedure times (B), contrast consumption (C) and cumulative X-ray dose (D) are shown. Grey dots represent the individual values, lines with error bars represent the means with 95% confidence interval.
Discussion
Carotid artery stenting has become a tenable alternative to carotid endarterectomy (CEA) for occlusive carotid disease in high-risk patients7. TRA for CAS is characterised by similar efficacy and earlier ambulation compared to the FA6; however, concerns about RAO limit its widespread use. To help prevent this complication, we used DTRA for CAS, by adopting the sheathless guiding approach previously published for complex PCI8. The main rationale behind the use of DTRA instead of cannulating at wrist level is to limit the haemodynamic effect of a potential occlusion at the puncture site. Before the radial artery arrives in the snuffbox area it already gives rise to multiple side branches, including the superficial palmar arch. These vessels can alleviate the effect of an eventual distal occlusion on the transradial blood flow in the forearm, and on the distal blood supply of the hand. Our results with DTRA were comparable to TRA controls, although we noted higher initial fluoroscopy and procedural times. This can be explained by the learning curve of the operators.
Limitations
We recognise that the retrospective study design and the relatively low number of subjects included in our analysis represent important limitations to our study; however, we believe that our data confirm the feasibility of this potentially useful new approach.
Conclusion
Our data indicate the applicability of DTRA for CAS. Randomised trials are needed to prove the potentially better safety profile of this approach.
|
Impact on daily practice DTRA can be adopted for carotid interventions with comparable safety and efficacy to the routine TRA. Slightly elevated procedure times are seen in the learning phase, but DTRA was not associated with excess radiation exposure or increased contrast consumption. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.