Abstract
Aims: To assess the procedural feasibility and early safety of hybrid coronary revascularisation, combining off-pump left internal mammary artery grafting to the left descending coronary artery (LAD) through an inferior J-hemisternotomy (JOPCAB) with percutaneous coronary intervention (PCI) of non-LAD lesions.
Methods and results: A total of 100 patients with multivessel coronary artery disease involving LAD were included in this prospective registry. Hybrid revascularisation was performed by JOPCAB, either prior to PCI (89%) or following PCI (11%). In 96% of the cases, the procedure was carried out according to the preoperative strategy and without perioperative (24 hours) major adverse cardiac or cerebral events. At one month, we observed no deaths, one stroke and two procedure-related myocardial infarctions. Five patients underwent reoperation for graft dysfunction, four of whom were identified by angiography without prior signs of ischaemia. Reoperation due to bleeding was necessary in six patients, and nine patients received red blood cell transfusion.
Conclusions: Our prospective registry documented promising procedural feasibility and early safety of coronary hybrid revascularisation combining JOPCAB with PCI. ClinicalTrials.gov identifier: NCT01496664.
Abbreviations
CABG: coronary artery bypass grafting
CAD: coronary artery disease
CK-MB: creatine kinase-myocardial band
Cx: circumflex coronary artery
DES: drug-eluting stent
JOPCAB: off-pump coronary artery bypass grafting through inferior left J-hemisternotomy
LAD: left anterior descending coronary artery
LIMA: left internal mammary artery
MACCE: major adverse cardiac and cerebral events
PCI: percutaneous coronary intervention
RCA: right coronary artery
SYNTAX: SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery
Introduction
In patients with multivessel coronary artery disease (CAD), randomised trials have documented the superiority of coronary artery bypass grafting (CABG) compared to medical therapy and percutaneous coronary intervention (PCI) regarding long-term symptom relief, survival and the need for reintervention1-3. In addition, substantial evidence indicates that left internal mammary artery (LIMA) grafting of the anterior descending coronary artery (LAD) is the main determinant of the beneficial effects of CABG4-6. Therefore, current revascularisation guidelines recommend CABG as the primary treatment in patients with CAD, with the exception of one-vessel and two-vessel disease without proximal LAD involvement7,8. On the other hand, degeneration of saphenous vein grafts (SVG) and other conduits to non-LAD vessels may favour the use of PCI, but this issue remains to be addressed in randomised clinical trials. Opinions on the use of PCI in patients with CAD and involvement of the proximal LAD are split. PCI is an attractive option because of minimal invasiveness, rapid recovery, and few short-term complications. Therefore, PCI is preferred by many interventional cardiologists and patients, even in the case of proximal LAD involvement.
Hybrid coronary revascularisation with a combination of PCI and CABG may be an option to improve outcome, using drug-eluting stents (DES) for significant non-LAD lesion and minimally invasive mammary artery LAD grafting, providing long-term revascularisation of the left ventricular anterior wall and septum.
Minimally invasive off-pump techniques have been developed to reduce the surgical trauma of CABG. The small incision, avoidance of aortic manipulation and cardiopulmonary bypass with cardioplegic arrest serve to reduce the risk of neurologic events, bleeding, infection, and pulmonary complications compared with conventional CABG.
The concept of making decisions on the best option for coronary revascularisation by the Heart Team involving cardiac surgeons and cardiologists is not new, but was revitalised after the SYNTAX trial, setting new standards for coronary revascularisation decision making. In designing hybrid revascularisation procedures, a well-functioning Heart Team is a prerequisite.
At present, there are no larger series of hybrid procedures using a combined minimally invasive LIMA to LAD anastomosis and PCI with DES. The aim of this study was to describe the feasibility and early safety of a hybrid approach in a series of CAD patients, who, according to our practice, would have been treated with either PCI or CABG.
Methods
STUDY DESIGN AND PATIENT POPULATION
Our prospective feasibility study included 100 adult patients with symptomatic multivessel CAD involving a significant stenosis or occlusion of the proximal LAD. The study had an “all-comers” approach with evaluation of all patients referred for coronary revascularisation at Aarhus University Hospital, Skejby, Denmark. The local ethics committee approved the study. Patients were included if the LAD lesion was amenable by surgical revascularisation, and the remaining lesions could be treated by PCI. Exclusion criteria were the need of extensive stenting defined as more than three non-LAD lesions, and complex stenting defined as stenting of bifurcation or severely tortuous and/or calcified coronary lesions. Further exclusion criteria were ST-elevation myocardial infarction within 24 hours, expected survival of less than one year, history of CABG or PCI with use of DES, and contraindication to double antiplatelet treatment or DES. Assessment of the patients and allocation of treatment was made by a Heart Team consisting of invasive cardiologists and cardiac surgeons. We intended to achieve complete revascularisation of all vessels with visually assessed angiographic vessel diameter of ≥2 mm and diameter stenosis of ≥50%.
STUDY OUTCOMES
We assessed the one-month rate of all-cause death, myocardial infarction9, stroke (focal central neurological deficit lasting >24 hours), and reintervention by PCI or CABG (MACCE). We defined acute procedural success as successful LAD grafting and PCI treatment according to the preoperative plan in the absence of MACCE during the first 24 hours after intervention. Finally, we registered reoperation for bleeding, sternum infection, and pulmonary embolism. Procedure-related myocardial infarction was defined as suggested by the Task Force for the Redefinition of Myocardial Infarction9. JOPCAB-related myocardial infarction was defined as biomarker values more than five times the 99th percentile of the upper reference limit during the first 72 hours following surgery, when associated with the appearance of new pathological Q-waves or new left bundle branch block, or angiographically documented new graft or native coronary artery occlusion, or imaging evidence of new loss of viable myocardium.
PCI-related myocardial infarction was defined as biomarker values more than three times the 99th percentile upper reference limit.
LOGISTICS OF HYBRID CORONARY REVASCULARISATION
All patients were admitted to the surgical ward. Two cardiac surgeons with substantial experience in off-pump coronary surgery obtained written informed consent and performed the surgery in all patients. In general, surgery was scheduled to precede PCI by two to five days. In case of chronically occluded non-LAD vessels, PCI was performed prior to surgery to avoid the need of surgical reintervention in case of PCI failure. Consequently, in these patients JOPCAB was carried out on double antiplatelet treatment. Acetylsalicylic acid treatment was continued until surgery in all patients with critical LAD lesion or acute coronary syndrome.
Minimally invasive coronary artery bypass grafting was performed off-pump through an inferior J-hemisternotomy under direct vision (JOPCAB) (Figure 1). After hemisternotomy, we recommended no physical restrictions other than to respect the individual’s pain threshold. Patients, who paused with acetylsalicylic acid therapy prior to surgery, resumed the treatment with a bolus of 300 mg orally six to nine hours postoperatively. Lifelong acetylsalicylic acid 75 mg daily was prescribed in all patients after the operation. Dalteparin 5000 IE was given twice daily to prevent deep venous thrombosis until the day before PCI. Patients on dual antiplatelet therapy after PCI prior to JOPCAB did not receive low molecular heparin therapy postoperatively.
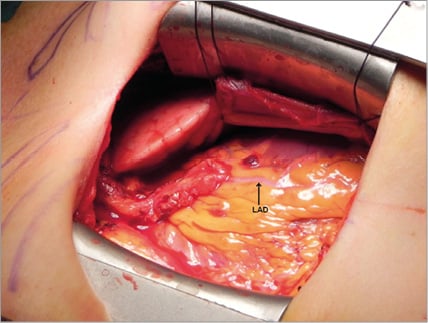
Figure 1. Intraoperative photograph showing completed LIMA-LAD anastomosis.
We used second and third-generation DES. Fractional flow reserve (FFR) measurement was performed in cases of angiographically borderline stenosis. A loading dose of 300 mg clopidogrel was administered the evening before PCI and continued for 12 months at a dose of 75 mg once daily.
Data management and analysis
All data were prospectively entered in EpiData Entry (EpiData Association, Odense, Denmark) applying double entry verification for data quality control. Values are reported as median and range or as percentages.
Results
BASELINE CHARACTERISTICS
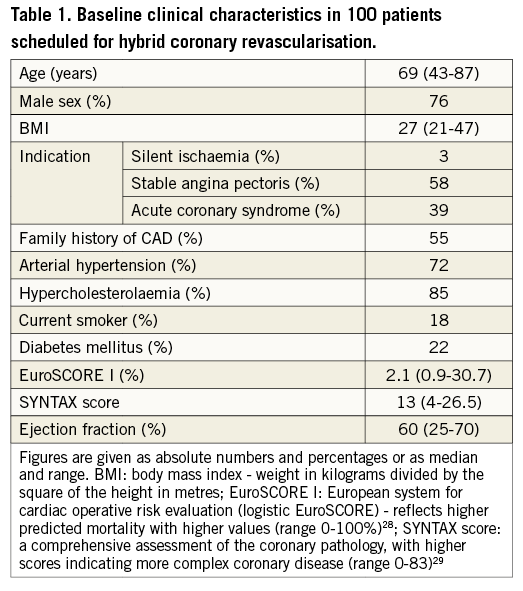
A total of 100 patients were included in the study from October, 2010 to February, 2012. Baseline patient characteristics are given in Table 1. During the study period 308 patients were treated by CABG and 280 by PCI for multivessel disease involving a LAD lesion.
HYBRID REVASCULARISATION
JOPCAB was performed prior to PCI in 89 (89%) patients, and PCI was scheduled prior to surgery in 11 (11%) patients with total occlusion of a non-LAD artery. Two of these patients were treated by CABG, as revascularisation by PCI failed. We chose to reoperate one patient with LIMA graft thrombosis and procedure-related myocardial infarction by conventional CABG, as the LAD had shown diffuse arteriosclerotic disease at JOPCAB. One PCI-related myocardial infarction was observed. Thus, the acute procedural success rate was 96%. The median length of index hospitalisation was eight days (range 5-33).
JOPCAB
JOPCAB was performed in 98 patients with a median operating time of 90 minutes (range 55-180 minutes). Intraoperatively, no haemodynamic instability was observed. Temporary ST-segment elevations were present in three patients. The median length of skin incision was 12 centimetres (range 9-16 centimetres). Intraoperatively, no JOPCAB had to be converted to complete sternotomy.
In two cases, the LIMA was injured at the oblique transection into the third intercostal space. Both grafts could be reconstructed successfully, as demonstrated by postoperative angiography. Five patients underwent reoperation for dysfunction of the LIMA graft (three occlusions, two significant stenoses). Myocardial infarction was diagnosed in one of these patients with postoperative ST-elevation and significant CK-MB release due to LIMA graft occlusion. Notably, LIMA graft dysfunction in the remaining four patients was identified at the prescheduled postoperative coronary angiography without prior signs of ischaemia. In one of these cases, Doppler flow measurement at reoperation revealed no graft dysfunction. In two cases, the steel wires closing the sternal transection had distorted the LIMA. Both grafts were without stenosis at angiography after revision.
Postoperatively, we observed three superficial sternal wound infections and no cases of deep sternal infection or sternal instability. No patient required dialysis or more than one routine overnight intensive care stay. Further, we found JOPCAB feasible in cases of reduced left ventricular ejection fraction, occluded LAD, morbid obesity, pleural adhesions and reduced lung function.
PCI
The procedural and lesion characteristics of the PCI procedures are provided in Table 2. Postoperative FFR measurement documented functionally non-significant stenoses in seven of the 148 non-LAD target lesions (5%). Consequently, five patients needed no further treatment after surgery. PCI was omitted in the patient who was reoperated for LIMA graft dysfunction by conventional CABG.
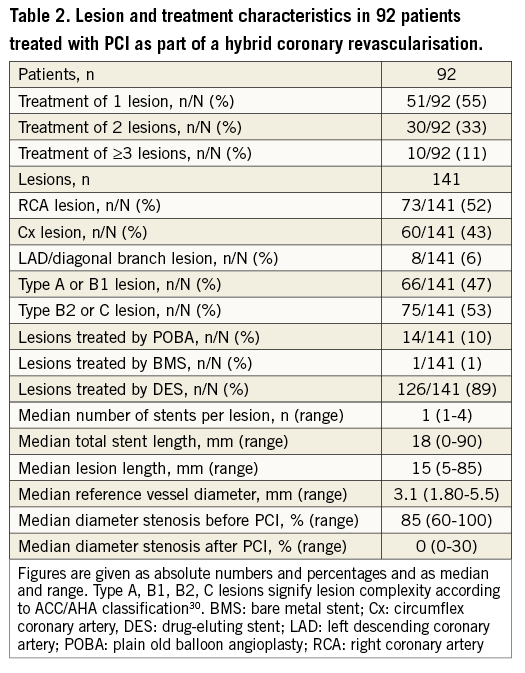
PCI was unsuccessful in one patient with a chronic total occlusion and in another patient with reocclusion after chronic total occlusion treatment. Thus, 141 non-LAD coronary artery lesions were treated by PCI in 92 patients.
SAFETY AT ONE MONTH
One month after completed hybrid intervention, we observed no deaths. There was one stroke on the fourth postoperative day and two procedure-related, but no spontaneous myocardial infarctions (one following JOPCAB with LIMA graft occlusion, one following PCI). LIMA graft dysfunction in five patients led to reoperation before discharge. Thus, the rate of major adverse cerebral and cardiac events (MACCE) was 7%.
ANTIPLATELET THERAPY AND SURGERY
At the time of surgery, 53 patients were on antiplatelet medication prior to surgery: 45 were receiving aspirin 75 mg daily and nine patients were on double antiplatelet medication with 75 mg clopidogrel and 75 mg aspirin following PCI. Following acute coronary syndrome, six patients received additional fondaparinux or low-molecular-weight heparin. Early reintervention because of excessive bleeding postoperatively was required in six patients. One patient developed haematoma in the left pleural cavity after PCI and was treated with a chest tube. Red blood cell transfusion was necessary in nine patients.
Discussion
We assessed the procedural feasibility and early safety of hybrid coronary revascularisation combining JOPCAB with PCI with DES. Our study demonstrated that hybrid coronary revascularisation could be performed with a high rate of procedural success and a low risk.
Our concept of hybrid coronary revascularisation is based on the unproven assumption that LIMA grafting of LAD will improve long-term survival as compared to PCI, and that PCI of non-LAD lesions using DES is non-inferior to grafting of non-LAD lesions using saphenous veins or other graft materials.
Hybrid coronary revascularisation was introduced when off-pump technology enabled LIMA-to-LAD placement through minimally invasive access10-12. Most investigators gained surgical access through a mini-thoracotomy with or without robotic support in order to reduce operative trauma13-18, but, until now, technical issues, time consumption, treatment logistics, and patient selection have been prohibitive for a wide adoption of these procedures.
Riess et al11 demonstrated that JOPCAB was a safe and effective surgical technique for the hybrid approach. Hemisternotomy has been shown to be comparable to mini-thoracotomy with regard to early postoperative pain19. JOPCAB provides excellent exposure of the heart, the technique can be applied under direct vision, and no specialised instrumentation or patient selection is required. It can be considered advantageous that the JOPCAB procedure is technically less challenging than revascularisation through ministernotomy or thoracoscopy. Experience in standard off-pump technique is the only prerequisite.
Functional perfection of the LIMA-to-LAD anastomosis is the essential part of any surgical revascularisation procedure involving LAD. In hybrid coronary revascularisation, the graft function can be controlled angiographically. Here, the frequency of early patency and significant anastomosis stenosis after conventional CABG may serve as a benchmark. Berger et al reported LIMA graft occlusion in 1.3%, and a ≥50% diameter stenosis of the LIMA graft in 7.8% of more than 600 elective CABG patients after 11 days20. In a recent study using routine intraoperative angiography after conventional CABG, 7% of patients needed revision of the LIMA graft21. Similar rates of LIMA dysfunction were identified in the PREVENT IV trial after one year22. Thus, LIMA graft dysfunctions at one year may be correctable at the initial surgical procedure. In the present study, we observed angiographic occlusion in 3%, and significant stenosis in 2% of the LIMA grafts. Our results confirm that early LIMA graft patency following JOPCAB is comparable with the results of conventional surgical techniques. In our series, all patients with LIMA graft dysfunction underwent revision on the basis of the angiographic findings before discharge. At one of these revisions, intraoperative Doppler flow assessment revealed no graft dysfunction. This case illustrates the difficult interpretation of a postoperative angiographic LIMA anastomosis stenosis in the absence of symptoms or signs of ischaemia. The majority of significant stenoses by early angiography are reported to resolve at follow-up23. Therefore, early angiographic findings should be evaluated considering clinical symptoms and possibly FFR measurements.
In the early phase of the study, we saw LIMA graft entrapment by the sternal closure in two patients. An important message from our feasibility study is that special attention must be paid to the LIMA graft placement at the time of chest closure to avoid this specific JOPCAB pitfall.
During the one-month observation period, there was no mortality but we observed one stroke on the fourth postoperative day. Recent multicentre trials have shown that postoperative stroke remains a major drawback of CABG3,24. Evidence is accumulating that the elimination of cardiopulmonary bypass and aortic manipulation can reduce the incidence of early stroke after coronary surgery25-27. The procedural myocardial infarction after JOPCAB was related to LIMA graft occlusion. Thus, leaving significant coronary artery lesions untreated during the surgical intervention and for two to five days between the JOPCAB and PCI procedures did not result in ischaemic events.
The avoidance of a full sternotomy allowed all patients to recover without sternal precautions, and we did not see deep sternal infection or instability. No patients needed dialysis or prolonged mechanical ventilation. Excessive bleeding resulted in reoperation in six (6%) patients. Nine (9%) patients required red blood cell transfusion although more than half of our patients were on antiplatelet medication. Therefore, the general course of the combined treatment seems to be acceptable.
The median SYNTAX score was 13 (4-26.5) in our patients. Omitting the LAD lesion, the SYNTAX score was 5 (0-5) based on the lesions to be treated by PCI. Thus, the PCI part of the combined revascularisation was a low-risk procedure.
Both of the failed PCI procedures were caused by chronic total occlusions, one failed procedure and one early stent thrombosis, where we decided on a conventional CABG operation. We used drug-eluting stents in almost all lesions. Per protocol, FFR measurement was recommended if there was any doubt of stenosis severity. Consequently, PCI was omitted in five patients.
In the present study, JOPCAB was the first procedure in the combined revascularisation in 89 (89%) patients, while we started with PCI in the remaining 11 (11%) patients. A true combined hybrid procedure performed in one session, in a dedicated hybrid laboratory, seems to be an attractive alternative and should be investigated.
Limitations
A limitation of the present study is that we did not routinely apply transit-time flow measurement (TTFM). We will investigate one-year graft patency by angiographic follow-up.
Conclusion
In conclusion, the present prospective registry study documented promising procedural feasibility and one-month safety of hybrid coronary revascularisation combining JOPCAB with PCI of non-LAD lesions.
Acknowledgements
We are grateful to Vibeke Laursen and Helle Bargsteen for their precious logistic and secretarial support.
Conflict of interest statement
The authors have no conflicts of interest to declare.

