Abstract
Aims: To assess outcomes of TAVR as a rescue therapy in patients with cardiogenic shock due to acutely decompensated aortic stenosis.
Methods and results: Of 771 high-risk patients who underwent TAVR, 27 (3.5%; 78±9 years; 12 men) were treated emergently due to acutely decompensated aortic stenosis with cardiogenic shock. SAPIEN and CoreValve prostheses were implanted in 11 and 16 patients, respectively: the transfemoral access route was used in 25. Three patients died within 72 hours of successful valve deployment, and a further six died within a month, giving a 30-day mortality of 33.3%, which was significantly higher than in electively treated patients (7.7%, p<0.0001). Univariate predictors of 30-day mortality in cardiogenic-shock patients were baseline cardiac output <3.0 l/min, reduced cardiac power index, impaired renal function, and mechanical ventilation, as well as severe acute kidney injury after TAVR. Estimated one-year survival was 59.3% in emergently and 82.7% in electively treated patients (p=0.0009). However, 30-day landmark analysis showed no difference in cumulative survival between TAVR modalities. In cardiogenic-shock patients without concomitant reduced cardiac output and impaired renal function at baseline (n=22), estimated one-year survival was 72.7%.
Conclusions: TAVR should be considered a reasonable rescue therapy in patients with cardiogenic shock secondary to decompensated aortic stenosis.
Introduction
Calcific aortic stenosis (AS) is the most common acquired valvular heart disease in adults next to mitral regurgitation1. With a mortality risk of up to 50% within 12 months, the prognosis of untreated AS is poor2. Patients in cardiogenic shock due to decompensated severe AS have an even poorer prognosis, and they also have an extremely high operative risk (up to 21% operative mortality) for surgical aortic valve replacement3. Another therapeutic option in such patients is percutaneous balloon aortic valvuloplasty (BAV), first described by Cribier et al in 19864. BAV can be a life-saving treatment option in patients with cardiogenic shock due to severe AS5-7; however, there is still an excessively high in-hospital mortality rate of up to 70% after rescue BAV and also a high incidence of valvular restenosis6,8. Transcatheter aortic valve replacement (TAVR) has been successfully introduced for the treatment of severe valvular aortic stenosis in elective high surgical risk as well as inoperable patients2,9. However, the current guidelines on the management of valvular heart disease consider haemodynamic instability a relative contraindication for TAVR, implying that the intervention may only be performed if the benefits are thought to outweigh the risks10.
The aim of the present study was to assess the periprocedural and one-year outcomes of TAVR as a life-sustaining rescue therapy in patients with acute cardiac decompensation due to severe valvular AS.
Methods
PATIENTS
Between August 2008 and September 2013, a total of 771 high-risk patients underwent TAVR at our institution. With growing experience, starting with patient #165, all consecutive patients in cardiogenic shock due to acutely decompensated AS were also treated; they were all catecholamine (norepinephrine and dobutamine) dependent at baseline and had been transferred from the intensive care unit to undergo TAVR. In cases of hypoxaemia, patients were intubated and mechanically ventilated. The reason for hypoxaemia was the presence of lung oedema and pneumonia. All patients in need of mechanical ventilation were intubated on the intensive care unit before TAVR.
In this study, in accordance with the IABP-SHOCK II trial, a patient was considered to be in cardiogenic shock “if he or she had a systolic blood pressure of less than 90 mmHg for more than 30 minutes or needed infusion of catecholamines to maintain a systolic pressure above 90 mmHg, had clinical signs of pulmonary congestion, and had impaired end-organ perfusion. The diagnosis of impaired end-organ perfusion required at least one of the following: altered mental status; cold, clammy skin and extremities; oliguria with urine output of less than 30 ml/h; or serum lactate level higher than 2.0 mmol/l”11.
TAVR
Decompensated AS was established as the cause of the patients’ haemodynamic predicament by angiographic exclusion of relevant coronary artery stenoses or occlusions immediately before TAVR. There were no patients with decompensated AS and significant untreated coronary artery disease. All patients were discussed within a Heart Team consisting of at least one interventional cardiologist and one cardiac surgeon. All patients had, according to current guidelines, symptomatic severe valvular AS (aortic valve area ≤1.0 cm² or mean transvalvular aortic pressure gradient ≥40 mmHg) and a noticeably raised operative risk (logistic EuroSCORE >20% or the presence of other risk factors contraindicating surgical valve replacement). All procedures were performed in a hybrid operating room. Details of the TAVR procedure using either the balloon-expandable SAPIEN/SAPIEN XT (Edwards Lifesciences Inc., Irvine, CA, USA) or the self-expanding CoreValve® (Medtronic, Minneapolis, MN, USA) prosthesis have been described previously9,12. In short, measurement of the annulus was performed by transoesophageal echocardiography and angiography of the aortic root; a pigtail catheter with radiopaque markers was used for measurement of the iliac arteries. No computed tomography scan was performed in patients with cardiogenic shock because of their haemodynamic instability. The decision on the type of prosthesis was based on anatomical conditions (the CoreValve prosthesis was preferred for smaller vessel or larger annulus sizes). In cases of haemodynamic instability, patients were placed on cardiopulmonary bypass in the hybrid operating room immediately before TAVR at the discretion of the interventionalist; cardiopulmonary bypass was discontinued in the hybrid operating room upon successful deployment of the prosthetic valve. Outcome parameters were classified according to the VARC-2 criteria13.
INVASIVE HAEMODYNAMICS
Right-heart catheterisation was performed in all patients with a 7 Fr Swan-Ganz catheter (Edwards Lifesciences) before and after TAVR. Right atrial pressure, systolic, diastolic and mean pulmonary artery pressures, as well as pulmonary capillary wedge pressure were recorded. Cardiac output and stroke volume were determined using the thermodilution method. For patients in cardiogenic shock, the cardiac power index (CPI) was calculated as CPI [W/m2]=mean arterial pressure [mmHg]×cardiac index [l/min/m2]×0.0022. Mean and maximum transvalvular aortic pressure gradients were measured, and the aortic valve area was calculated immediately before and after TAVR using the Gorlin formula.
FOLLOW-UP
After hospital discharge, follow-up was scheduled at 30 days, six and 12 months.
ETHICS
Written informed consent was obtained from all patients or their representatives.
STATISTICS
Continuous variables are described as means and standard deviations if normally distributed, or as medians plus interquartile range if not. Differences between continuous variables were analysed with t-tests if data were approximately normally distributed, and with the Wilcoxon-Mann-Whitney test in cases of non-normally distributed data and markedly unequal group sizes. Categorical variables are described with absolute and relative frequencies. Differences between categorical variables were evaluated with the chi-square test or with Fisher’s exact test in case of small expected cell frequencies. Fisher’s exact test was also used to compare mortality rates between the emergency and elective TAVR groups at 30 days after TAVR. Survival curves were estimated by the Kaplan-Meier method, and the log-rank test was used to assess survival differences. Binary logistic regression analysis was used to determine variables predictive of 30-day mortality in cardiogenic-shock patients. For overall tests, a two-tailed p-value <0.05 was considered statistically significant. All calculations were performed using the SAS software version 9.3 (SAS Institute, Cary, NC, USA).
Results
PATIENTS
The mean age of the 771 patients (361 men [46.8%]) was 80±7 years. Of these, 27 patients (3.5%) were treated as emergency cases due to acutely decompensated severe AS with cardiogenic shock, whereas 744 patients underwent elective TAVR. Demographic data and comorbidities according to TAVR modality (elective vs. emergent) are presented in Table 1. Patients with cardiogenic shock had a significantly higher logistic EuroSCORE and suffered more often from chronic kidney disease and pulmonary hypertension.
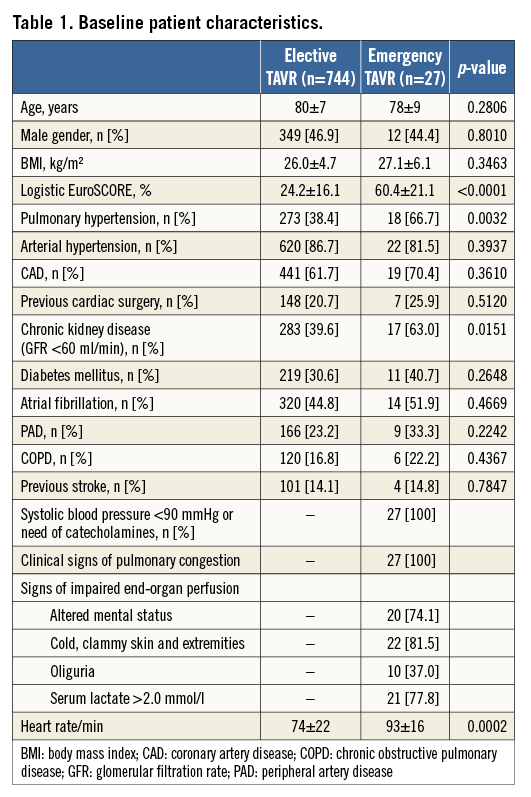
Baseline echocardiographic variables according to TAVR modality are listed in Table 2 and reveal a significantly smaller aortic valve area, as well as a lower prevalence of moderate or severe aortic regurgitation and a lower left ventricular ejection fraction, in emergently treated patients.
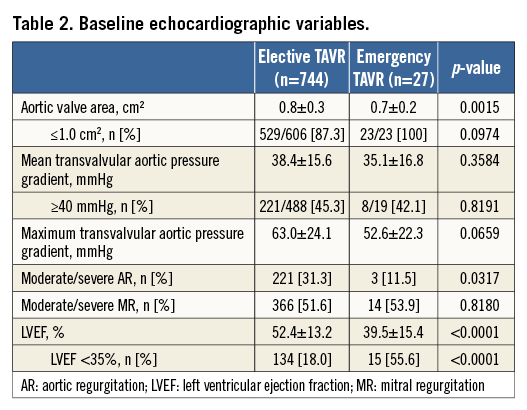
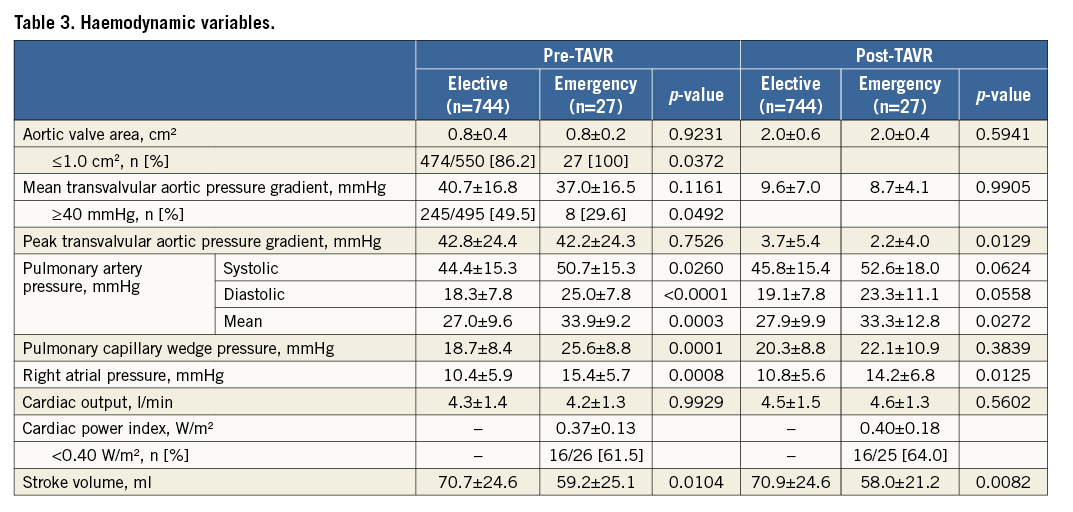
Before TAVR, patients with cardiogenic shock had significantly higher pulmonary artery pressures, higher pulmonary capillary wedge and right atrial pressures, and a significantly lower stroke volume (Table 3). Immediately after TAVR (with cardiogenic-shock patients still on catecholamines), mean pulmonary artery pressure and right atrial pressure were still significantly higher, and stroke volume significantly lower, in patients with cardiogenic shock than in electively treated patients (Table 3). Patients were carefully weaned off catecholamines in the next two to three days after TAVR.
OUTCOMES
Acute device success according to the VARC-2 definition (i.e., correct positioning of single valve prosthesis in proper location, with intended valve performance and no death <72 hours13) was achieved in 24 patients with cardiogenic shock (88.9%) and in 673 electively treated patients (90.5%, p=0.738). The three device failures in the cardiogenic-shock group were due to intraprocedural death (n=1) or post-procedural death within 72 hours (n=2).
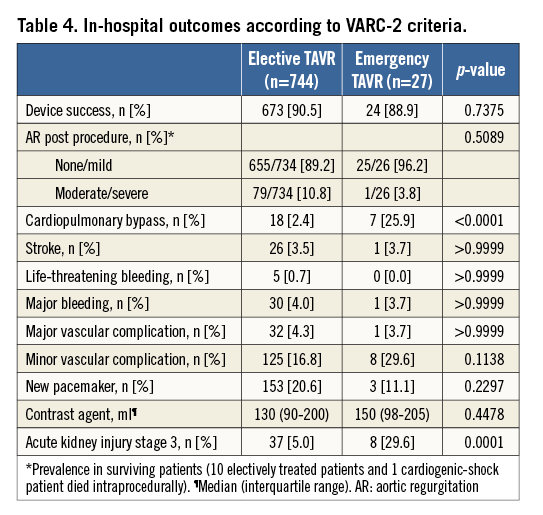
Cardiopulmonary bypass was necessary in 25.9% of the cardiogenic-shock patients yet only 2.4% of electively treated patients (p<0.0001). The types of valve prosthesis and access routes employed in this study are shown in Figure 1. CoreValve and SAPIEN prostheses were implanted in almost equal measure and the transfemoral access route was most frequently used (92.6% of emergently treated and 78.4% of electively treated patients), with no statistically significant difference between the treatment modalities. There were no significant differences in the occurrence of major or minor vascular complications; however, patients with cardiogenic shock significantly more often developed acute kidney injury (AKI) of Acute Kidney Injury Network stage 313 after TAVR (Table 4). The amount of contrast volume administered during the procedures was not different between electively and emergently treated patients (Table 4). Four cardiogenic-shock patients became temporarily dialysis-dependent.
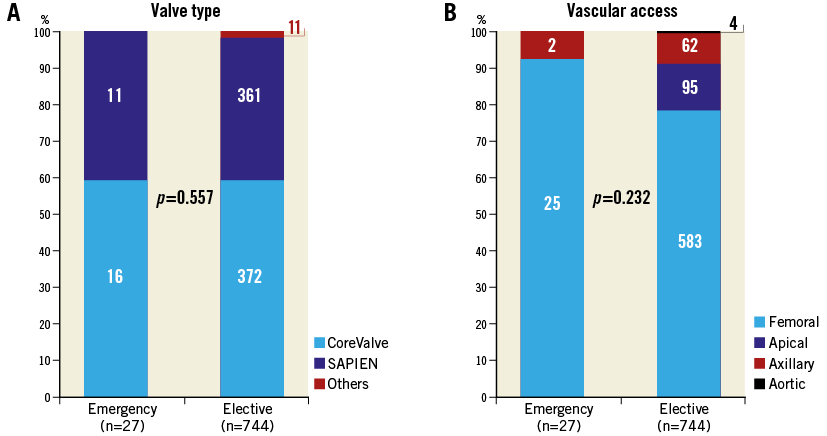
Figure 1. Types of valve prosthesis and vascular access according to TAVR modality. A) Valve prosthesis types were used in almost equal measure in both patient groups. B) Transfemoral vascular access was used in 93% of emergently treated patients and in 78% of electively treated patients.
Survival up to one year was significantly worse in emergently as compared to electively treated patients, with Kaplan-Meier estimates of survival at 30 days of 66.7% and 92.3% and at one year of 59.3% and 82.7%, respectively (Figure 2). The statistically highly significant difference in survival curves (p=0.0009) was apparently due to the significantly increased 30-day mortality rate in emergently treated patients. Within 30 days of TAVR, nine (33.3%) of the 27 cardiogenic-shock patients had died, as opposed to 56 (7.7%) of 729 electively treated patients (p=0.0002). A 30-day landmark analysis of cumulative survival showed no difference between emergently and electively treated patients once they survived 30 days (Figure 3).
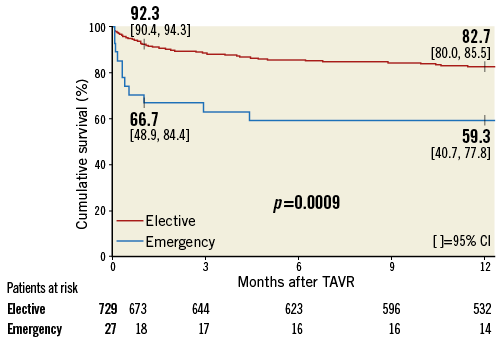
Figure 2. Cumulative survival curves according to TAVR modality. Thirty-day survival in emergently treated patients (blue survival curve) was 66.7%, significantly lower than in electively treated patients (92.3%; red survival curve). The difference in overall survival was maintained at one year. CI: confidence interval
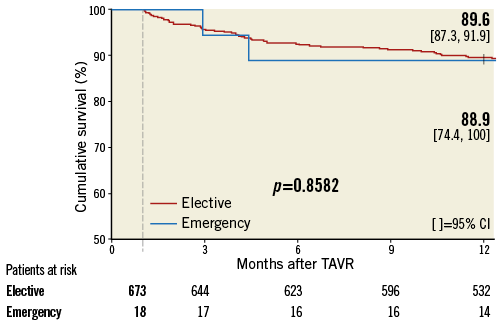
Figure 3. Thirty-day landmark analysis of cumulative survival curves according to TAVR modality. Exclusion of all patients who died within 30 days of TAVR revealed that survival up to one year was not different between treatment modalities once patients survived 30 days. CI: confidence interva
In the nine patients with cardiogenic shock who died within 30 days of TAVR, the predominant cause of death was pneumonia and sepsis (six patients [66.7%]) rather than cardiovascular (three patients). These nine patients differed significantly from the 18 cardiogenic-shock patients who survived 30 days with respect to the prevalence of baseline cardiac output <3 l/min (55.6% vs. 44.4%, p=0.0235), intubation with mechanical ventilation (88.9% vs. 33.3%, p=0.0128), and chronically impaired renal function (100% vs. 55.6%, p=0.0258); moreover, the former patients presented with a significantly lower cardiac power index (0.28 W/m² vs. 0.40 W/m², p=0.0263) (Table 5). Of note, all five cardiogenic-shock patients in whom both reduced cardiac output and impaired renal function were present died within 30 days. In the remaining 22 patients (81.5%), the Kaplan-Meier estimate of one-year survival was 72.7% (95% CI, 54.1%-91.3%).
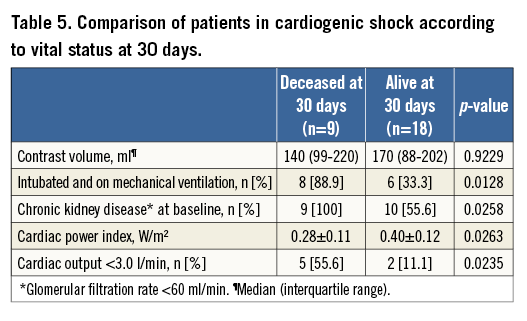
On univariate logistic regression analysis, the odds ratio (OR) of death within 30 days in emergently treated patients was 10.0 (95% CI, 1.39-71.9; p=0.022) for cardiac output <3.0 l/min, 16.0 (95% CI, 1.61-159; p=0.018) for intubation with mechanical ventilation, and 0.39 (95% CI, 0.15-0.97; p=0.043) for a 0.10 W/m² increase in cardiac power index. Since AKI stage 3 occurred in six (66.7%) of the nine patients who had died by 30 days and in only two (11.1%) of the 18 patients who survived 30 days (p=0.0061), this post-TAVR complication was associated with an OR of 16.0 (95% CI, 2.12-121; p=0.007). A multivariate analysis was not possible because of the low number of emergently treated patients.
Functional status at one year was assessed in 14 cardiogenic-shock patients, with 10 patients (71.4%) in New York Heart Association Class I (n=4) or II (n=6), and four in Class III. Two further patients who had survived 30 days did not complete one year of follow-up.
Discussion
MAJOR FINDINGS
The present study has shown that emergency TAVR using predominantly transfemoral access in patients presenting with cardiogenic shock secondary to acutely decompensated valvular AS is feasible, with a device success rate of 89%, no increase in periprocedural complications, and an acceptable 59% probability of one-year survival. Obviously, baseline conditions in emergently treated patients were significantly worse than in electively treated patients, with markedly increased logistic EuroSCORE, a high prevalence of pulmonary hypertension and chronic kidney disease, and compromised left ventricular function in the former. Moreover, all cardiogenic-shock patients were catecholamine-dependent and half of them required mechanical ventilation at the time of TAVR. Despite the patients’ critical condition, a single prosthetic valve was successfully implanted in all, yet three patients died within three days and a further six patients had died by 30 days. These nine deaths were predominantly due to non-cardiovascular causes.
The 30-day mortality rate of 33.3% in cardiogenic-shock patients was significantly higher than the 7.7% observed in electively treated patients; it was the apparent reason for the former patients’ increased mortality up to one year. However, once emergently treated patients survived TAVR for 30 days, no statistical difference in longer-term survival vs. electively treated patients was noted.
The most powerful univariate factors adversely impacting on 30-day mortality in cardiogenic-shock patients were a baseline cardiac output <3.0 l/min and reduced cardiac power index, impaired renal function, the need for mechanical ventilation, and severe AKI post TAVR. The concomitant presence of reduced cardiac output and impaired renal function before TAVR entailed death within 30 days in all cases.
CLINICAL RELEVANCE
The data presented herein suggest that TAVR, in experienced hands, should be considered a reasonable rescue therapy in patients with cardiogenic shock secondary to acutely decompensated valvular aortic stenosis. The only apparent contraindication to this approach appears to be the concomitant presence of reduced cardiac output and impaired renal function. Conversely, the probability of one-year survival, in the roughly 80% of study patients in whom this adverse combination of baseline comorbidities was not present, was 73%. Thus, in the majority of patients with cardiogenic shock, the benefits of the intervention appear to outweigh its risks.
The significantly increased 30-day mortality rate in patients with cardiogenic shock is of major clinical concern and should be prophylactically addressed. The main reason for mortality in our patients with cardiogenic shock was pneumonia and sepsis, concordant with a significantly higher prevalence of mechanical ventilation at baseline in patients who died within 30 days as compared to patients who survived 30 days. Therefore, treatment with broad-spectrum antibiotics and lung-protective ventilation for pneumonia and sepsis should be started as early as possible14.
ALTERNATIVE THERAPEUTIC APPROACHES
In the past, balloon aortic valvuloplasty (BAV) has been regarded as a bridge to surgery or TAVR in haemodynamically unstable patients at high surgical risk, and as palliative treatment in patients in whom neither surgery nor TAVR is an option10. However, the mean post-BAV aortic valve area in cardiogenic-shock patients has been reported at values between 0.80±0.20 cm215 and 0.84±0.27 cm27, which still represents severe AS in most cases; moreover, in such patients in-hospital mortality after BAV was reported to be as high as 71.4%, with an increased restenosis rate6,8. In carefully selected high-risk patients, TAVR has already been shown to be superior, in terms of one-year mortality and functional class, to BAV, surgery, and medication only16. Further study is warranted to clarify whether BAV is beneficial in the apparently few cardiogenic-shock patients with baseline comorbidities that make sustained benefit from TAVR unlikely.
The transapical approach to TAVR is currently the most frequently used after transfemoral vascular access. A surgical team recently reported their experience with transapical TAVR in 186 patients with a logistic EuroSCORE >40% and also in 21 cardiogenic-shock patients with a marginally higher logistic EuroSCORE than in the present study. They observed an overall one-year survival rate of 46% in patients with cardiogenic shock17,18. Since several studies have reported higher mortality rates in patients who underwent transapical rather than transfemoral TAVR19,20, we believe that transfemoral TAVR is a valid choice for patients in cardiogenic shock requiring urgent treatment. In cases where this approach is not feasible (as in two of our patients), the transaxillary route may be contemplated.
Limitations
This is an observational study of 771 consecutive patients from a single centre. In addition, the data represent a retrospective analysis without randomisation. The low number of patients with cardiogenic shock prohibited multivariate analysis of factors impacting on 30-day survival. The retrospective character of our analyses does not take into account that our results may have been affected by unmeasured confounding variables. Ideally, the value of TAVR versus other therapeutic measures in patients with aortic stenosis in cardiogenic shock should be assessed by way of a randomised trial. However, the ethical issues of such a trial involving patients in an emergency situation need to be addressed first.
Conclusions
In patients with cardiogenic shock secondary to acutely decompensated valvular aortic stenosis, TAVR using predominantly transfemoral vascular access should be considered a viable therapeutic option despite a 30-day mortality rate of 33%. Careful patient selection according to baseline comorbidities may lead to cumulative one-year survival in excess of 70%. Prospective validation of our findings is warranted.
| Impact on daily practice Patients with cardiogenic shock due to acutely decompensated aortic stenosis are a highly distinct patient population in daily practice. Treatment of these very sick patients is difficult. In the past, only BAV or cardiac surgery existed as treatment options. However, both approaches were associated with high mortality. Nowadays, in the TAVR era, a new treatment option with acceptable outcome is available for these special patients. |
Conflict of interest statement
U. Schäfer has been working as a proctor for Edwards Lifesciences and Medtronic Inc. K-H. Kuck has received honoraria payments from Edwards Lifesciences and Medtronic Inc. The other authors have no conflicts of interest to declare.
References