Abstract
Aims: The present observational case-control study assessed the cost-effectiveness of contemporary vascular closure devices (VCDs) for the prevention of vascular complications in an all-comers transfemoral percutaneous coronary intervention (PCI) population.
Methods and results: A total of 8,292 consecutive PCI patients were enrolled from a single-centre prospective registry from January 2005 to December 2010. VCDs were available from July 2007 and, from that time point, VCDs were implanted in 1,780 of the 5,394 patients (33%). Vascular complications occurred in 221 (2.7%) patients. The use of VCDs was independently associated with a 53% risk reduction (OR 0.47, 95% CI: 0.3-0.7) in vascular complications (3.0% vs. 1.5%) and with a 65% risk reduction (IRR 0.37, 95% CI: 0.32-0.43) in the post-PCI length of hospital stay (LOS) (mean 2.8 vs. 1.5 days). Mainly due to the reduced LOS, the patients with VCDs accrued vascular direct medical costs (VCD, diagnosis and treatment of vascular complications, post-PCI LOS) that were on average 498€ less than those accrued by the non-VCD patients. The cost-effectiveness was present across all vascular risk profiles.
Conclusions: In this large, all-comers transfemoral PCI population, the use of VCDs was independently associated with a reduction in the rate of vascular complications and the post-PCI length of hospital stay and proved to be cost-saving across all vascular risk profiles.
Abbreviations
ACS: acute coronary syndrome
BARC: Bleeding Academic Research Consortium
GP: glycoprotein receptor
IRR: incidence rate ratio
LOS: length of hospital stay
OR: odds ratio
PCI: percutaneous coronary intervention
VCDs: vascular closure devices
Introduction
Arterial access-related vascular complications are among the most common adverse events after transfemoral percutaneous coronary intervention, and these complications occur in 3.5% to 8.4% of cases1-3. Vascular complications are associated with severe in-hospital morbidities, sometimes causing life-threatening bleeding4. Vascular closure devices have emerged as an alternative to conventional mechanical compression after PCI5. These devices potentially reduce the time to haemostasis, facilitate patient mobilisation, decrease the length of hospital stay and improve patient satisfaction6-8. Although randomised and large-scale non-randomised trials with early VCD technology could not demonstrate a benefit with respect to the prevention of vascular complications, more recent registries with more contemporary VCDs have shown a significant reduction in vascular complications2,3,9-12. Nevertheless, despite growing evidence, the adoption rate for VCDs remains below 50%, even in the more recent PCI studies13. Cost concerns may have hampered the widespread use of these closure devices in daily practice. Studies on the health economic implications of VCDs are scarce and have focused mainly on the direct material costs or on the costs related to vascular complications, whereas the cost reduction related to a potentially shorter length of hospital stay should also be considered14,15. In addition, the risk for vascular complications is variable with a higher vascular complication rate particularly in patients of advanced age and female gender16,17. A more in-depth analysis of the cost-effectiveness across different risk profiles may help to define whether VCDs should be recommended for routine use or only for those patients at high vascular risk.
Therefore, this study was designed to assess the cost-effectiveness of currently available vascular closure devices to prevent femoral artery access-related vascular complications in an all-comers PCI population, across the different vascular risk profiles.
Methods
STUDY POPULATION
We evaluated 8,530 consecutive patients who underwent PCI at the Antwerp University Hospital from January 2005 to December 2010. Patients with brachial access (n=77), radial access (n=25) and intra-aortic balloon pump (n=136) were excluded from the analysis. The final study population consisted of 8,292 transfemoral PCI patients, who were subdivided into a study group which received VCDs (n=1,780) and a control group which received conventional compression after sheath removal (n=6,512). VCDs were available in the catheterisation laboratory from July 1, 2007, and were subsequently inserted into 33% of the patients (1,780/5,394).
A prospective catheterisation laboratory database, based on the European CARDS Registry definitions, was used to record the clinical and procedural elements for each case18.
Informed consent was obtained from all patients or from their legal representatives. The study was approved by our institutional review board.
CATHETERISATION PROCEDURE
The PCI was performed by standard techniques using 6 Fr sheaths for the majority of the procedures, and 8 Fr sheaths for the complex bifurcation lesions. All of the PCIs were performed by eight experienced operators, each with an annual PCI volume ranging between 150 and 400 procedures. The antithrombotic regimens included aspirin, clopidogrel and unfractionated heparin, which were adjusted to achieve and maintain an activated clotting time of 250 to 300 seconds (200 to 250 seconds if glycoprotein IIb/IIIa inhibitors were used). Adjunct glycoprotein IIb/IIIa receptor inhibitors were used at the discretion of the operators.
The vascular access after PCI was managed irrespective of the antithrombotic regimen which was chosen. When VCDs were used, femoral angiograms were obtained before their placement to identify any anatomical restrictions, such as punctures at arterial bifurcation sites, the presence of severe calcification or the presence of severe peripheral artery disease. The final decision for insertion of a VCD was based on anatomical and clinical criteria and was left to the discretion of the operator. Among the operators, the proportion of VCD use varied between 13% and 55%, which reflected differences in adoption policy among the different operators.
The majority of the utilised VCDs consisted of a 6 Fr Angio-Seal™ Evolution (81%) (St. Jude Medical, Minneapolis, MN, USA), whereas an 8 Fr Angio-Seal was applied in 8% of the patients, and a 6 Fr StarClose SE® (Abbott Vascular, Santa Clara, CA, USA) was applied in 11% of the patients.
Patients assigned to manual compression underwent sheath removal four hours after PCI and were kept at bed rest overnight. Patients assigned to VCDs underwent immediate sheath control and were ambulated after four hours of bed rest after the procedure. Before discharge, evaluation of the access site was routinely performed and recorded for each patient.
VASCULAR COMPLICATIONS AND MEDICAL CARE COSTS
The vascular complications were reviewed as follows: false aneurysms (confirmed by ultrasonography), arteriovenous fistulas (confirmed by ultrasonography), arterial occlusions with limb ischaemia (confirmed by ultrasonography), arterial infections and severe access-site bleeding (haematoma) confirmed by a Bleeding Academic Research Consortium (BARC) score of >1. The latter category included patients with important blood loss who required prolonged hospitalisation and medical/surgical interventions19.
All of the reported vascular complications were reviewed by an independent clinical events committee and a BARC score was assigned retrospectively to each vascular complication.
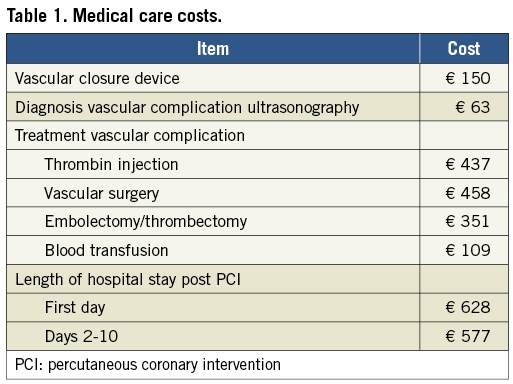
The hospital medical care costs generated up to six weeks post PCI were assessed for all the patients (based upon the hospital billing data) and were expressed in euros (2010 values).
Table 1 describes the most frequently encountered costs, subdivided into the costs related to the VCDs, the diagnosis and treatment of vascular complications and the post-PCI hospital stays.
STATISTICAL ANALYSIS
Continuous variables are presented as mean value (±SD) or as median followed by interquartile ranges (IQR). Baseline characteristics of the patients with VCDs versus those without VCDs were compared using a chi-square analysis or Fisher’s exact test for categorical variables and Mann-Whitney U test for the continuous values. The influence of VCDs on the vascular complications and the post-PCI LOS was determined using logistic and hurdle regression models, respectively, after accounting for the propensity to use VCDs. In addition to the VCD use, the following dependent factors, commonly assessed in post-PCI vascular complications studies, were included in these regression models: age, gender, history of vascular disease, hypertension, hypercholesterolaemia, renal failure (defined as creatinine >2.0 mg/dl), current history of smoking, diabetes mellitus, number of diseased coronary arteries, modalities of PCI (urgent versus elective), cardiogenic shock, resuscitation, ad hoc PCI (defined as PCI and diagnostic coronary angiography within the same procedure) and the use of GP IIb/IIIa receptor antagonists. Weight was not included in the logistic regression model because of too many missing values. Analyses of possible interaction between vascular risk profile and effect of VCDs were performed by entering an interaction term into the regression model.
The vascular direct medical costs (including the VCDs, the diagnosis and treatment of vascular complications and the post-PCI hospital stay) were compared between VCD patients and non-VCD patients. The mean cost differences and confidence intervals were estimated by bootstrapping (10,000 iterations).
All statistical tests are two-sided, and a p-value of <0.05 was considered statistically significant. All of the statistical analyses were performed using SAS version 9.1 software (SAS Institute, Cary, NC, USA).
Results
STUDY POPULATION
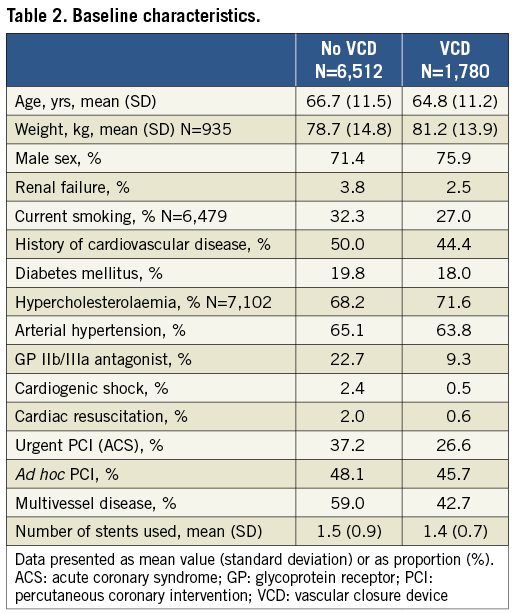
The baseline characteristics of the 1,780 patients with VCDs and the 6,512 patients without VCDs are presented in Table 2. The VCD patients were younger, were more frequently male, had fewer comorbidities and were haemodynamically more stable than the non-VCD patients. Furthermore, more of the urgent PCIs were performed and more glycoprotein IIb/IIIa antagonists were used in the study population which received no VCDs.
VASCULAR COMPLICATIONS
The overall in-hospital vascular complication rate was 3.4% (n=285) and occurred in 221 patients (2.7%). These vascular complications included false aneurysms (58%), major haematomas with a BARC >1 (31%), arteriovenous fistulas (6%), arterial occlusions (1.4%) and arterial infections (0.7%).
The VCD patients exhibited a significantly reduced risk of developing at least one vascular complication, decreasing from 3.0% to 1.5% (p<0.0007). Table 3 lists the vascular complications per study group. The main benefit of using VCDs was the reduction of false aneurysms and of major haematomas (particularly with a BARC >3). By contrast, the use of VCDs was associated with a small increased risk of local infections. Indeed, two VCD patients were readmitted three days after PCI because of local infection at the puncture site for which prolonged IV antibiotic treatment was needed. One of these patients developed an abscess and required surgical excision and drainage.
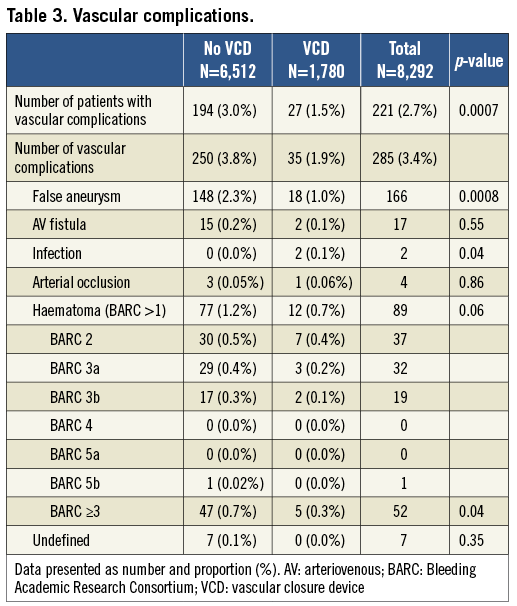
In-hospital mortality related to vascular complications occurred in two patients, both of whom belonged to the study group which received no VCDs.
During the period from January 2005 until June 2007 (before the introduction of the VCDs), the vascular complication rate was 2.7% (81/2,956), whereas during the period from July 2007 to December 2010 (after the introduction of the VCDs) the complication rate was 3.2% (113/3,557) in the non-VCD patients (p=0.3, adjusted OR 1.1, 95% CI: 0.8-1.6).
DETERMINANTS OF VASCULAR COMPLICATIONS AND RISK STRATIFICATION
The most important baseline risk predictors of vascular complications were female gender (OR 2.1, 95% CI: 1.67-3.33) and advanced age (OR 1.027, 95% CI: 1.01-1.04) (Table 4). After correction for differences in the baseline risk profiles between both study groups and after correction for the time period (before vs. after introduction of the VCDs), the use of VCDs was independently associated with a risk reduction of 53% (OR 0.47, 95% CI: 0.3-0.7).
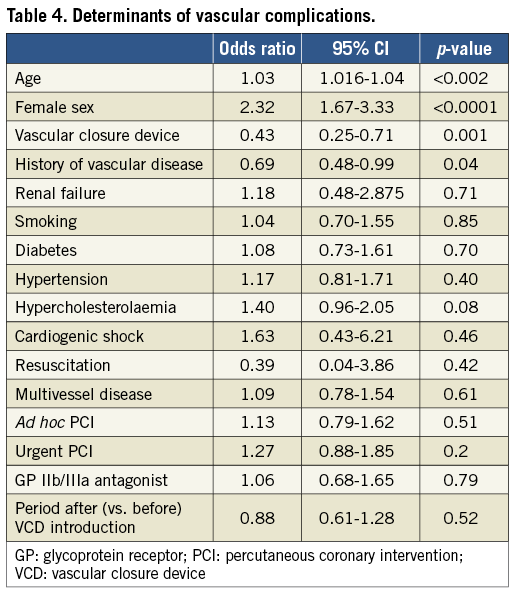
Based on the gender and the ROC curve-derived cut-off value of 75 years (yrs), the total population was further subdivided into low-risk (men <76 yrs, n=4,857), intermediate-risk (men >75 yrs or women <76 yrs, n=2,559) and high-risk (women >75 yrs, n=856) groups. Figure 1 displays the complication rates for the different risk populations, stratified according to VCD use. The vascular complication rate increased from 1.9% for the low-risk group to 7.0% for the high-risk group of patients without VCDs, whereas the vascular complication rate was comparable among the different risk groups of patients with VCDs (1.7% for the low-risk group and 2.2% for the high-risk group, p=0.15). Accordingly, the benefit of the VCDs was the highest in the high-risk group (absolute difference of 4.8%), whereas it was marginal for the low-risk group (absolute difference of 0.1%). Additional analysis revealed a significant interaction between vascular risk profile and VCD effect with stronger adjusted odds ratios for higher-risk patients (OR 0.24, 95% CI: 0.06-0.90) and intermediate-risk patients (OR 0.20, 95% CI: 0.06-0.63) and weaker adjusted RR for lower-risk patients (OR 0.8, 95% CI: 0.44-1.56).
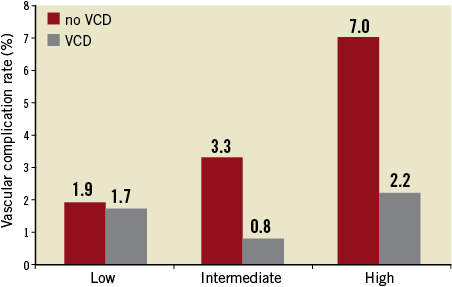
Figure 1. Vascular complication rate (%) for patients with versus without VCDs, according to vascular risk profile (low, intermediate, high).
From the time point at which VCDs were available (July 2008), they were implanted into 24.5% (132/537) of the high-risk patients, 30.1% (499/1,656) of the intermediate-risk patients and 36.6% (1,145/3,129) of the low-risk patients.
LENGTH OF HOSPITAL STAY (LOS) AND VCD USE
The average length of the post-PCI hospital stay was 2.5 (median 1, IQR 1) days. The use of VCDs reduced the LOS from a mean of 2.8 (median 1, IQR 1) days to 1.5 (median 1, IQR 0) days. The incidence of prolonged hospitalisation (>7 days post PCI) decreased from 7.0% for the non-VCD patients to 1.8% for the VCD patients (p<0.0001). This beneficial effect on the LOS was seen in all previously defined vascular risk groups, with an average reduction of 1.2 days (Figure 2). Hurdle regression models revealed that VCD use was independently associated with a 63% reduction in LOS (IRR 0.37, 95% CI: 0.32-0.43) but the effect of VCDs on LOS was significantly stronger in the low-risk (IRR=0.37, 95% CI: 0.30-0.45) and intermediate-risk groups (IRR=0.30, 95% CI: 0.23-0.39) as compared to the high-risk group (IRR=0.59, 95% CI: 0.37-0.93).
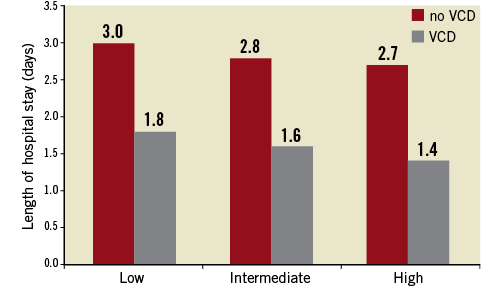
Figure 2. Length of hospital stay (days) for patients with versus without VCDs, according to vascular risk profile.
MEDICAL COSTS
Table 5 provides data on the average cost per patient related to the hospitalisations, vascular complications (diagnosis and treatment) and VCDs. The total average cost was 1,608€ for the non-VCD patients and 1,113€ for the VCD patients. This cost-saving effect was mainly attributable to the reduction in the LOS. Based on the bootstrap simulation, the average cost saving was 498€ (95% CI: -9,088€ +3,037€). In 88% of the pairwise comparisons the VCD excess net cost was less than 151€ (Figure 3). In 29% of the cases the procedure with VCD use was cost-saving. Furthermore, the use of VCDs had a median cost per avoided vascular complication of approximately 10,000€.
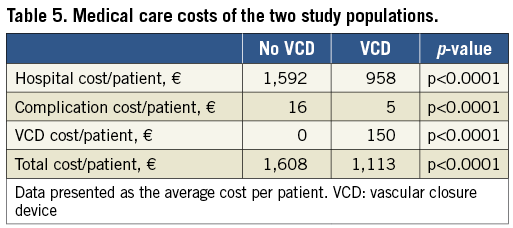
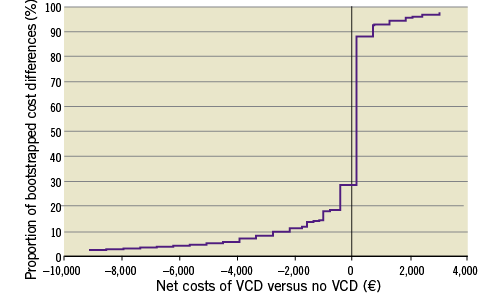
Figure 3. Distribution of total cost differences between patients with and without VCDs based upon 10,000 bootstrapped pairwise comparisons (the 95% distribution around the median is shown).
A subgroup analysis based on the vascular risk profiles revealed comparable cost savings, with an average cost saving of 500€ in the high-risk patients, 510€ in the intermediate-risk patients and 376€ in the low-risk patients.
Discussion
The present study evaluated the cost-effectiveness of contemporary VCDs in an all-comers PCI population. The results revealed that the use of VCDs was associated with a 53% reduction in vascular complications and that these devices were cost-saving for the average patient independently of initial vascular risk profile, mainly through a reduction in the length of hospital stay.
For Angio-Seal, the predominantly used VCD in the present study, early studies revealed no significant benefit as compared to mechanical compression with complication rates of 3.8% (87/2,289) and 4.2% (464/10,975), respectively2,3,9. These previous studies were characterised by a high use (>50%) of 8 Fr sheaths and GP IIb/IIIa antagonists. Over time, VCDs, including the Angio-Seal, have been modified and simplified which has resulted in less vascular closure device failure and a lower risk of vascular complications12. In the present study, 8 Fr sheaths were only used in a minority of cases (only for bifurcation stenting), and GP IIb/IIIa receptor antagonists were administered in fewer than 20% of the patients. This fact might explain the observed lower incidence of local vascular complications not only in our control patient population without VCDs (3.0%) but particularly in the VCD study group (1.5%). Our findings are consistent with a recent observational study by Arora et al that demonstrated a 44% reduction in the incidence of vascular complications with Angio-Seal use compared with manual compression in PCI patients10.
Furthermore, the present study demonstrated that the risk profile might significantly affect any advantages of using VCDs. In accordance with previous reports, female gender and advanced age were the most important risk factors for vascular complication16. Lower body mass index, drug dosing issues related to lower creatinine clearance, and smaller vessel size may contribute to the excess risk seen in women20. In the present study, high-risk patients (females >75 yrs) exhibited the greatest benefit (5% absolute reduction), whereas the benefit of VCDs in the low-risk groups was only marginal (less than 0.5%). Hence, VCD use resulted in an obliteration of the vascular risk categories. Despite the demonstrated benefits, the high-risk patients were the least likely to receive VCDs (only 25%) as compared to the low-risk patients. This apparent risk-treatment paradox has also been observed in other trials targeting PCI bleeding complications13. Several factors may have contributed to the lower use of VCDs in high-risk patients in our study population. First, assessing the risk for bleeding in clinical practice was not commonly used in our daily clinical practice. Secondly, at the time of introduction of the VCD, the prior published data showed conflicting results and this may have hampered the application of VCDs particularly in high-risk patients. Lastly, safe arterial access may be more challenging in elderly women due to smaller and shorter common femoral arteries which might have precluded the use of VCDs in some high-risk patients.
Anyway, these findings reinforce the need to apply a more routine risk stratification when selecting the patients who will benefit most from VCDs. The use of the proposed simplified risk model based upon gender and age may facilitate this pre-procedural risk stratification.
Beyond the prevention of vascular complications, the use of VCDs was also associated with a more than 50% reduction in the post-PCI length of hospital stay. This reduction in the length of stay was independent of the risk profiles of the study groups, indicating that the reduction of LOS is also significant in patients without vascular complications. VCDs have been demonstrated to reduce the time to haemostasis and to facilitate patient mobilisation, which enables their earlier discharge from the hospital6,7.
The reduction of the length of stay was the most important favourable factor for the cost-effectiveness of VCDs. We demonstrated that the VCDs were cost-saving for the total study population (on average, 498€). Studies on the cost-effectiveness of vascular closure devices are scarce and have focused mainly on the direct material costs or on the costs related to vascular complications. The study of Resnic et al demonstrated that the routine use of the Angio-Seal was associated with a lower cost per PCI procedure of 44$14. That study used a decision analytic model with an estimated vascular complication rate based upon a pooled analysis of all randomised studies with the Angio-Seal and did not take into account cost reduction related to a shorter LOS. In fact, in our study population, the cost reductions related to shorter hospital stays were far more important than the cost reductions related to vascular complications. This is also the reason why cost savings were comparable among the different patient risk profiles, which is an argument for a routine use instead of a risk-tailored use of VCDs post PCI.
The present study may foster the debate over whether the radial or the femoral approach is the most appropriate access route for PCI. In the “Radial versus femoral access for coronary angiography and intervention with acute coronary syndromes (RIVAL) study”, vascular complications occurred in 3.7% of the patients with a femoral approach versus 1.4% of the patients with a radial approach (intention-to-treat analysis)21. In the femoral approach group, 25% received a vascular closure device. In view of the beneficial effects of VCDs on vascular complications, as observed in our study, a more systematic use of vascular closure devices would diminish the gap between the radial and the femoral approach. Moreover, the radial approach is problematic in up to 20% due to an abnormal Allen’s test, refractory radial spasm or subclavian tortuosity, and may be less suitable for the more complex PCI procedures16,22. By contrast, VCDs cannot be implanted in as many as 20% of patients because of anatomic restrictions10. Hence, the availability and the expertise in both techniques (radial and femoral approach with VCDs) will ensure the lowest vascular complication rate in a global PCI population.
Limitations
The results of this study should be considered in the context of the following limitations. Because the present study was conducted at a single centre with high-volume operators, the results cannot be automatically translated to other centres. However, a single-centre study design may attenuate the confounding factor of differences in expertise, which are more prevalent in multicentre studies. Furthermore, it should be noted that, due to the non-randomised study design, a selection bias could have influenced the outcome in the two different study populations. We tried to minimise this effect by using multivariate analysis after accounting for the propensity to use VCDs, and we found no evidence that the VCDs were more frequently selected for low-risk patients. In fact, the incidence of vascular complications in the control group (during the period after the introduction of VCDs) was not significantly higher than that in the group before the introduction of VCDs.
In any case, only a randomised clinical trial will be able to overcome this limitation and will allow the accurate assessment of the beneficial effect of VCDs as compared to mechanical compression.
Conclusions
In conclusion, the use of vascular closure devices was shown to be independently associated with a reduction in the overall vascular complication rates and in the length of hospital stay, as well as providing cost-saving benefits.
| Impact on daily practice The widespread use of vascular closure devices after transfemoral PCI has been mainly hampered by cost concerns and by the recent introduction of the transradial approach. However, the transfemoral approach will remain the preferred access route for patients with problematic radial access (due to spasm, tortuosity, abnormal Allen’s test) or for some more complex PCI procedures. In these patients the present study may convince the interventional cardiologist to apply VCD routinely as it will increase patient comfort, reduce the vascular complication rate by 53% and will be cost-saving for the average patient, mainly through a reduction in the length of hospital stay. |
Acknowledgements
We thank Mr L. Avonds (head of the pricing department of the Antwerp University Hospital) for providing us with the billings of all included patients.
Conflict of interest statement
The authors have no conflicts of interest to declare.