Abstract
Aims: The aims of this study were to compare the index of microcirculatory resistance (IMR) and its determinants in diabetes mellitus (DM) and non-DM patients with vascular risk factors, and to evaluate the potential differential involvement of coronary microvascular beds.
Methods and results: Fifty-six patients (32 with DM), without significant epicardial coronary disease, had IMR measured in the anterior and posterior circulations. There was no significant difference in the anterior compared to posterior circulation IMR in the whole group (27 vs. 26, p=0.92) or in the DM subgroup (35 vs. 28, p=0.31). DM patients had higher anterior circulation IMR compared to non-DM patients (27 vs. 15, p=0.009). Posterior circulation IMR was higher than anterior circulation IMR in non-DM patients (25 vs. 16, p=0.01). Multivariate determinants of higher anterior circulation IMR in DM were dyslipidaemia, hypertension, worsening glycaemic control, and higher body mass index; metformin had a protective effect.
Conclusions: There is differential involvement of the coronary microvascular beds. In the presence of risk factors, microvascular function of the posterior circulation was affected before the anterior; DM patients had worse microvascular function in the anterior but not posterior circulation compared to patients without DM. Vascular risk factors, including DM, adversely affect coronary microvascular function, and their treatment was associated with improvement.
Abbreviations
CFR: coronary flow reserve
CT: computed tomography
FFR: fractional flow reserve
IMR: index of microcirculatory resistance
Introduction
Coronary microvascular function is pivotal to local vascular haemostasis by regulating myocardial blood flow. Coronary microvascular dysfunction may be seen without epicardial coronary artery disease or myocardial disease, in the presence of myocardial disease, with obstructive coronary artery disease, and in iatrogenic settings1. Furthermore, the presence and severity of microvascular dysfunction are of prognostic value in a range of cardiovascular conditions2,3.
Clinical assessment of coronary microvascular function is difficult. Non-invasive assessment with transthoracic and contrast echocardiography, computed tomography (CT) scan or nuclear techniques is not applied routinely4. Magnetic resonance imaging and positron emission tomography may assess myocardial blood flow with vasodilator stressors but do not provide information specific to coronary microvascular function, or to the microvascular function of specific coronary territories. Furthermore, no previous studies have compared microvascular function between different vascular beds within the coronary tree. The index of microcirculatory resistance (IMR) is a validated invasive measure of coronary microvascular function. This technique is relatively independent of haemodynamic changes, can be used in the presence of epicardial disease, and provides specific information on coronary microvascular function within a particular vascular bed5.
Patients with type 2 diabetes mellitus (DM) are at risk of developing macrovascular and microvascular complications. While patients with DM without epicardial disease have been shown to have impaired maximal coronary vasodilatory capacity by positron emission tomography6, it is unclear if coronary microvascular dysfunction is present in such patients by more contemporary measures such as the IMR. Furthermore, determinants of IMR, and whether microvascular function in different vascular beds is affected differently in patients with type 2 DM or other risk factors, are unknown. The aims of this study were to evaluate and compare coronary microvascular function in different coronary vascular beds with IMR in patients with DM and in patients without, and to identify determinants of IMR in DM patients.
Methods
PATIENTS
Fifty-six patients referred for elective diagnostic invasive coronary angiography were recruited. Patients were consecutively recruited only after significant coronary artery disease, defined as ≥70% diameter stenosis by computer-assisted quantitative coronary angiography using multiple planes, and fractional flow reserve (FFR) ≤0.75, had been excluded by coronary angiography. Patients with known significant coronary artery disease, acute coronary syndrome, previous myocardial infarction, significant valvular disease, severe hypertension (systolic pressure >200 mmHg and diastolic pressure >120 mmHg at rest), left bundle branch block and rhythm other than sinus were excluded. All subjects recruited had been screened for diabetes by their family physicians. Type 2 DM was diagnosed according to the American Diabetes Association criteria7. All medications were continued. All patients provided written informed consent. The study was approved by the hospital human research ethics committee.
Clinical data including age, height, weight, cardiac risk factors, duration of DM, medications, and presence of clinical microvascular complications were collected. Body mass index and body surface area were calculated. Laboratory data including current and previous glycaemic control, as determined by the average HbA1c results in the year leading up to coronary angiography, were recorded, in addition to lipid profile, creatinine, estimated glomerular filtration rate (measured by Chronic Kidney Disease - Epidemiology Collaboration [CKD-EPI] equation)8, urinary albumin to creatinine ratio, and reasons for referral for angiography.
CORONARY ANGIOGRAPHY AND CORONARY PHYSIOLOGY MEASUREMENTS
Selective coronary angiography was performed in multiple projections according to standard techniques. After conventional diagnostic coronary angiography, a total of 100 U/kg of intravenous heparin was administered. A 6 Fr coronary guiding catheter was used to engage the left main coronary artery to measure the IMR for the anterior circulation. A dose of 200 mcg of intracoronary nitroglycerine was given. A 0.014-inch coronary pressure wire (St. Jude Medical, St. Paul, MN, USA) was calibrated, equalised to the guiding catheter pressure with the sensor positioned just outside the ostium of the guiding catheter, and then advanced to the distal left anterior descending artery. The mean distance from the guide tip to the sensor was 85 mm. Coronary flow reserve (CFR), IMR and FFR were then measured at baseline and at maximal hyperaemia as described below.
The transit time of 3 mL of normal saline at room temperature injected down the coronary artery through the guiding catheter was determined using the thermodilution technique at rest, and again after maximal hyperaemia9. The average of three injections was measured. Steady state maximal hyperaemia was then induced using 140 mcg/kg/min of adenosine infused intravenously through a large-bore cannula in the antecubital fossa. Simultaneous measurements of mean aortic pressure measured at the tip of the guiding catheter and mean distal coronary pressure from the pressure wire were also taken at rest and at maximal hyperaemia. CFR was measured by the transit time at rest divided by the transit time at maximal hyperaemia. IMR was measured by the product of distal coronary pressure and transit time at maximal hyperaemia10. FFR was calculated as the ratio of distal to proximal coronary pressures at maximal hyperaemia.
The procedure was repeated for the posterior circulation after the patient had returned to baseline haemodynamic state after cessation of the adenosine infusion. The posterior circulation IMR was measured in the right coronary artery for a right dominant coronary circulation and in the left circumflex artery for a left dominant circulation. The mean distance from the guide tip to the sensor was 98 mm in the posterior circulation. The posterior circulation IMR was measured in 32 patients.
INTEROBSERVER AND INTRAOBSERVER VARIABILITY ANALYSIS
The interobserver and intraobserver variability of measurements of transit times was assessed in five randomly selected patients. After positioning of the pressure wire in the distal left anterior descending artery, one observer (DL) performed three baseline saline injections and recorded the mean transit time. Following this, a second observer (ML), who was blinded to the first result, then repeated these three measurements to determine intraobserver and interobserver variability.
STATISTICAL ANALYSIS
Continuous variables were presented as mean+SD unless otherwise stated. Continuous variables were compared with the Student’s t-test. Categorical variables were compared with chi-square or Fisher’s exact test where appropriate. Multiple linear regression analysis was used to identify determinants of the IMR with significant univariate predictors entered as independent variables. Normality testing was performed. Variables were transformed when necessary to ensure that the assumptions of linear regression were met. Intraobserver and interobserver variability were expressed as mean differences and Pearson correlation coefficients between the two sets of measurements, and as coefficients of variation. A two-tailed p-value <0.05 was considered significant. All statistical analyses were performed using Stata version 12 (StataCorp, College Station, TX, USA).
Results
The clinical characteristics of the 56 patients, divided into two groups according to whether they were suffering from DM or not, are listed in Table 1. There were 32 patients with DM and 24 patients without. There were more men, and hence a larger body surface area in the DM group. Patients with DM were more likely to be suffering from microalbuminuria. Otherwise, the two groups were well matched. The primary reasons for referral for coronary angiography were similar in the two groups.
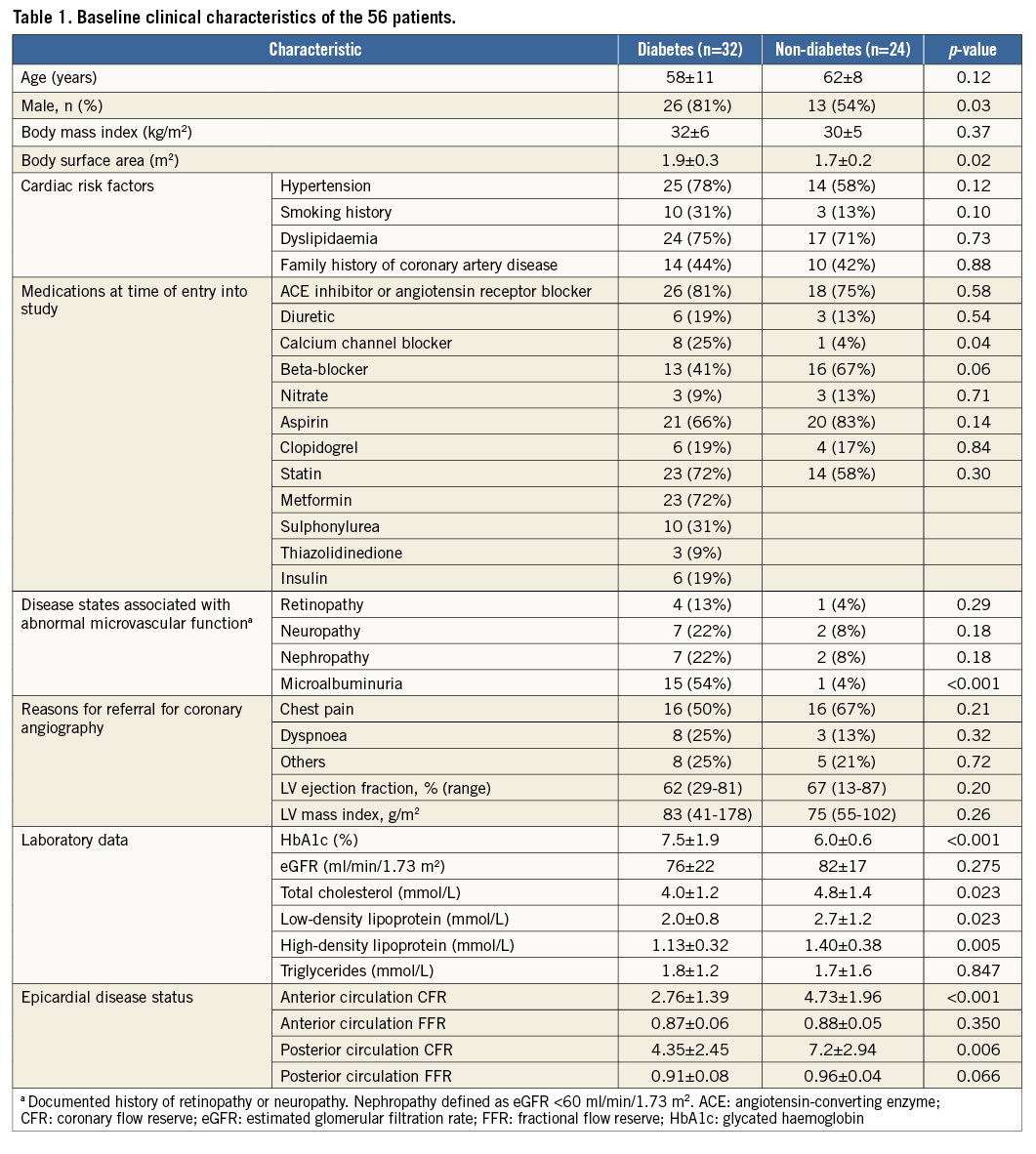
CORONARY MICROVASCULAR FUNCTION
During coronary physiology measurements, the mean blood pressure at rest was 136/74 mmHg. The mean blood pressure during hyperaemia for measurement of IMR for the anterior circulation was 118/64 mmHg and for the posterior circulation was 114/63 mmHg, without any significant differences in either systolic (p=0.09) or diastolic (p=0.35) blood pressures. There was a significant reduction in systolic blood pressure between rest and hyperaemia for both the anterior (p<0.001) and posterior (p<0.001) circulation measurements.
For the whole group of 56 patients, the mean CFR for the anterior circulation was 3.64 (interquartile range [IQR] 1.9-4.8), mean FFR was 0.87 (IQR 0.83-0.92), and mean IMR was 22 (IQR 12-23). The mean CFR for the posterior circulation was 5.69 (IQR 3.4-8.3), mean FFR was 0.94 (IQR 0.92-0.98), and mean IMR was 27 (IQR 14-37).
There was no significant gender difference in either the anterior or posterior IMR. There was also no significant difference in anterior and posterior circulation IMR (27 vs. 26, p=0.92).
In patients without DM, posterior IMR was significantly higher than anterior circulation IMR (25 vs. 16, p=0.01).
In patients with DM, while there was no significant difference in IMR between anterior and posterior circulation (35 vs. 28, p=0.31), the mean posterior circulation IMR was 28.
CORONARY MICROVASCULAR FUNCTION IN THE ANTERIOR CIRCULATION IN DIABETES
Patients with DM had a significantly higher IMR in the anterior circulation (27 vs. 16, p=0.009) compared with patients without DM. The anterior circulation IMR was significantly higher in DM patients with hypertension compared to DM patients without hypertension (31 vs. 14, p=0.007) and in DM patients with dyslipidaemia compared to DM patients without (32 vs. 14, p=0.006). Diabetic patients treated with metformin had a lower IMR compared with DM patients not on metformin (19 vs. 49, p=0.04). There were no differences in IMR when DM patients were subdivided according to other clinical characteristics including the presence or absence of other microvascular diseases or other medications, including insulin therapy. The anterior circulation IMR showed a significant positive correlation with HbA1c averaged over the previous 12 months prior to coronary angiography (p=0.02) and body mass index (p=0.04).
CORONARY MICROVASCULAR FUNCTION IN THE POSTERIOR CIRCULATION IN DIABETES
DM patients had a similarly elevated IMR in the posterior circulation compared to patients without DM (28 vs. 25, p=0.54). The posterior circulation IMR was also significantly higher in DM patients with dyslipidaemia compared to DM patients without (31 vs. 16, p=0.004). There were no differences in posterior circulation IMR when DM patients were subdivided into two groups according to other above-mentioned clinical characteristics.
DETERMINANTS OF CORONARY MICROVASCULAR FUNCTION IN DIABETES
Multivariate analysis identified a history of hypertension (p=0.04) and dyslipidaemia (p=0.05) to be positive predictors, and treatment with metformin (p=0.002) to be a negative predictor of higher anterior circulation IMR (R2=0.54, p=0.0008).
DETERMINANTS OF COMBINED ANTERIOR AND POSTERIOR CORONARY MICROVASCULAR FUNCTION IN ALL PATIENTS
A combined IMR was calculated as the average value of the anterior and posterior circulation IMR in the 32 patients where posterior circulation IMR was available. Multivariate analysis identified a history of hypertension (p=0.015), dyslipidaemia (p=0.002), DM (p=0.05) and body mass index (p=0.017) as being associated with higher combined IMR.
INTEROBSERVER AND INTRAOBSERVER VARIABILITY
The coefficients of variation of coronary transit time measurements at baseline were 4.0%±2.2%, and 5.1%±2.7% at maximal hyperaemia.
Discussion
We evaluated coronary microvascular function in different coronary vascular beds in a group of patients with multiple cardiovascular risk factors, including DM, with the IMR. Our patients represented a high-risk group, having a mean body mass index >30 kg/m2, 32 patients suffering from type 2 DM, and the majority of them suffering from hypertension and dyslipidaemia. We found a differential involvement of coronary vascular beds in patients with vascular risk factors: our patients with DM had worse coronary microvascular function in the anterior circulation than patients without DM. The opposite was observed in our patients without DM: coronary microvascular function was worse in the posterior circulation than in the anterior circulation. DM patients with dyslipidaemia, hypertension, worse glycaemic control and more overweight had worse coronary microvascular function, whereas those treated with metformin had better coronary microvascular function.
THE INDEX OF MICROCIRCULATORY RESISTANCE AS A MEASURE OF CORONARY MICROVASCULAR FUNCTION
The IMR is an established invasive parameter to evaluate coronary microvascular function and has been found to correlate well with true microvascular resistance measured in an animal model11. It is associated with much lower measurement variability and is not significantly affected by changes in haemodynamic conditions10. Whilst short distances of the pressure wire sensor from the guide catheter tip have been associated with time intervals that were too short for adequate curve fitting9, and higher variability in IMR measurements12, when the wire sensor was placed in the distal third of the artery, there was no significant correlation found between transducer distance and mean or resting hyperaemic coronary transit times10. Therefore, the differential finding of IMR in the anterior versus posterior circulations was unlikely to be due to differences in the distances between pressure wire sensor and the guidance catheter tip, and more likely to reflect actual differences in microvascular function between the two territories.
IMR is an indicator of microvascular function in the presence of epicardial coronary artery disease and provides prognostic information10,13,14, and is preferred over older invasive techniques such as CFR. More importantly, unlike other non-invasive methods of assessing coronary microvascular function, IMR can offer information specific to the coronary microvasculature and offers the unique opportunity to evaluate coronary microvascular function in specific coronary vascular beds. No studies, thus far, have utilised IMR to evaluate coronary microvascular function and its determinants in DM.
CORONARY MICROVASCULAR DYSFUNCTION IN DIABETES
Experimental studies on laboratory animals with hyperglycaemia and clinical studies in patients with DM have demonstrated impaired endothelium-dependent vasodilation15. The vast majority of these studies examined vascular reactivity in large conduit vessels like the brachial artery and, in the animal models, thoracic or abdominal aorta or the mesenteric arteries. However, studies have suggested that endothelial function of conduit vessels did not necessarily reflect that of smaller arteries16. As a result of the different physiological roles, endothelial function of conduit vessels may not reflect coronary microvascular function.
Positron emission tomography (PET) has been used to assess myocardial flow reserve in patients with DM17. While myocardial blood flow reserve was found to be reduced in patients with DM, epicardial coronary disease had not been excluded and may have affected the results and interpretation. Maximal myocardial vasodilatory capacity assessed with intracoronary Doppler flow wires was reduced in patients with DM and angiographically normal coronary arteries6. However, the contribution of other vascular risk factors to, and the impact of their treatment on coronary microvascular function are unclear.
Our study demonstrated differential involvement of coronary vascular beds in DM patients. This differential microvascular involvement may be explained by the patchy, uneven, and segmental manner in which diabetic microangiopathy, demonstrated on human biopsy and in animal studies, involves the diabetic myocardium18,19.
DETERMINANTS OF CORONARY MICROVASCULAR FUNCTION AND IMPACT OF TREATMENT IN DIABETES
Evidence for determinants of and impact of treatment on coronary microvascular function in DM was largely derived from animal studies15. Human studies have predominantly examined endothelial function of larger peripheral conduit arteries20 or utilised non-invasive techniques, whose results could have been affected by epicardial coronary disease, which is common in patients with DM17. In our study, patients with significant epicardial coronary artery disease were excluded, and the degree of coronary microvascular dysfunction was found to be related to the averaged glycaemic control, body mass index, and the presence of other vascular risk factors such as dyslipidaemia and hypertension. Metformin therapy appeared to have a protective effect.
We have shown a differential impairment of coronary microvascular function in different coronary vascular beds: DM patients have worse coronary microvascular function in the anterior circulation (mean IMR 27) but not in the posterior circulation compared with patients without DM.
Our non-DM patients were not a low-risk group with the majority of them having multiple coronary risk factors. The IMR of their posterior circulation was higher than that of the anterior circulation. Their mean IMR of the posterior circulation was 28, signifying that they already had significant coronary microvascular dysfunction in that vascular territory, whereas their mean anterior circulation IMR of 16 could still be considered within normal limits. One can postulate that, in all patients, the presence of vascular risk factors, including DM, affects coronary microvascular function in the posterior circulation initially before affecting the anterior circulation.
Metformin treatment in our DM patients appeared to be associated with better coronary microvascular function. Metformin may reduce microvascular dysfunction21. Mather et al also found improved endothelial function in peripheral conduit arteries with metformin in type 2 DM20. Our study further extends the observation of beneficial effects of metformin in coronary microvascular function in humans.
Weight loss and exercise in obese patients with insulin resistance have been shown to improve flow-mediated dilatation of the brachial artery with the main predictor of improvement being percentage change in body weight. Multiple studies have linked body weight to endothelial function of large conduit arteries and the beneficial effects of weight loss in improving endothelial function22,23. The finding from our study that body mass index was a significant multivariate determinant of IMR in our patients may also suggest a potentially beneficial effect of weight loss on coronary microvascular function.
Limitations
Our study was an observational study only: both the level of vascular risk factors and the treatment of the patients were not controlled. Furthermore, in view of the sample size, no attempt was made to relate the findings of the study to clinical outcome. We used only the anterior circulation IMR as the dependent variable in the multivariate model, as only 32 patients had the posterior IMR determined. Posterior circulation IMR was not available in 24 patients mainly due to technical reasons, the length of the procedure and the wishes of the patients. The difference in anterior and posterior circulation IMR was unlikely to be due to difference in hyperaemic response to intravenous adenosine, as the same dosage protocol was used and the drop in blood pressure was similar between the two measurements. As there were no previous studies comparing IMR between DM and non-DM patients and comparing the IMR between the anterior and posterior circulation, we were not able to estimate the required sample size reliably. A combined IMR, provided by the average of anterior and posterior circulation IMR, was used as a measure of global cardiac microvascular function. Given that the posterior circulation IMR measurement was that of the dominant posterior vessel (right coronary artery or left circumflex artery), this combined measure was thought to reflect the microvascular function of the majority of the myocardium. The microvascular function within the territory of the non-dominant posterior vessel was not included in this measure, as these non-dominant vessels were small and were supplying only a small amount of myocardium.
Conclusions
This study used IMR to evaluate specifically the coronary microvascular function in a high-risk group of patients. There was differential involvement of coronary vascular beds, with DM patients having worse microvascular function in the anterior circulation than the posterior circulation, whilst the converse was found to be true for non-DM patients. Determinants of worse coronary microvascular function in DM patients were found to be dyslipidaemia, hypertension, worse glycaemic control, and obesity, whilst metformin was associated with better microvascular function.
| Impact on daily practice Coronary microvascular function is adversely affected by vascular risk factors, including diabetes, even in the absence of significant epicardial coronary artery disease. There is differential involvement of different coronary vascular beds in the presence of vascular risk factors, with the microvascular function of the posterior circulation being affected before the anterior circulation. Assessment of both anterior and posterior circulation microvascular function is warranted. In daily practice, risk factor modification including treatment of hypercholesterolaemia, hypertension, weight loss and treatment with metformin may lead to improvement of microvascular function. |
Acknowledgements
The authors wish to thank Dr Yian Ping Lee, our registered nurse, Maria Rodrigues, scientific officer, Tony Yu, and the nursing staff in the cardiac catheterisation laboratory for their technical assistance and support.
Funding
The study was partially funded by a Pfizer Cardiovascular Lipid Research Grant.
Conflict of interest statement
The authors have no conflicts of interest to declare.