We read with great interest the article by Korsholm et al about transcatheter left atrial appendage occlusion (LAAO) in patients with atrial fibrillation (AF) and a high bleeding risk using aspirin (ASA) alone for post-implant antithrombotic therapy1. The authors conclude from their findings that LAAO with the AMPLATZER™ Cardiac Plug (ACP) or Amulet™ device (both St. Jude Medical, St. Paul, MN, USA) was safely performed with ASA monotherapy after implantation without an increased risk of device-related thrombosis or stroke. We have the following questions and concerns.
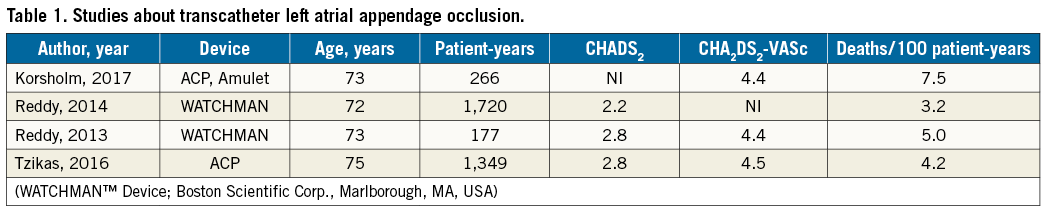
How do the authors explain the high mortality of the patients included in their study? Mortality is much higher than in other studies reporting on LAAO (Table 1) despite similar CHA2DS2-VASc scores2-4. It would be of great interest to know how long the estimated life expectancy was when the patients underwent LAAO.
Although the authors indicate that “none of the 20 deaths was procedure- or device-related”, it is important to know the exact cause of death. The left atrial appendage (LAA) is a structure for release of atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP). In normal human hearts, ANP concentration is 40-fold higher in the LAA than in the rest of the atrial free wall and in the ventricular endocardium. Since natriuretic peptides play an important role in fluid regulation, volume homeostasis, and thirst perception, LAA elimination may impede physiologic regulation of heart failure and thirst perception. A decrease of ANP- and BNP-serum levels after LAAO has been described in small cohorts5,6. Furthermore, dysregulation of ANP and BNP has been associated with obesity, glucose intolerance, type 2 diabetes mellitus, and essential hypertension. Moreover, natriuretic peptides have been implicated in protection against atherosclerosis, thrombosis, and myocardial ischaemia7. Thus, some of these secondary effects might possibly explain the high mortality.
Although follow-up investigations by transoesophageal echocardiography and CT had been carried out in the majority of the study patients, astonishingly no information is given about the rate of leaks between the LAA wall and the devices. The LAA myocardium has a higher distensibility than the left atrial myocardium. Progressive dilation of the LAA is observed in AF and thereby leakage of an initially completely closed LAA may occur8. After surgical LAAO, leaks are associated with thromboembolic events9. Since it is unknown how many “late leaks” develop after interventional LAAO and whether they are clinically relevant, imaging studies later than 12 months post implantation should be implemented.
Conflict of interest statement
The authors have no conflicts of interest to declare.