Calcification is visualised by optical coherence tomography (OCT) as a well-delineated, signal-poor region with sharp borders.
A 63-year-old female patient with stable angina underwent percutaneous coronary intervention. OCT (C7 Dragonfly™, ILUMIEN™ OCT system; St. Jude Medical, St. Paul, MN, USA) showed lumen narrowing with heavily calcified plaque (Figure 1A). Rotational atherectomy (RA) was performed using a 2 mm burr (Rotablator™ Rotational Atherectomy System; Boston Scientific, Marlborough, MA, USA). After RA, OCT clearly visualised the calcified segment ablated by the 2 mm burr as a circular hole (Figure 1B and Figure 1C, dotted line indicates the size of the 2 mm Rotablator burr, Moving image 1).
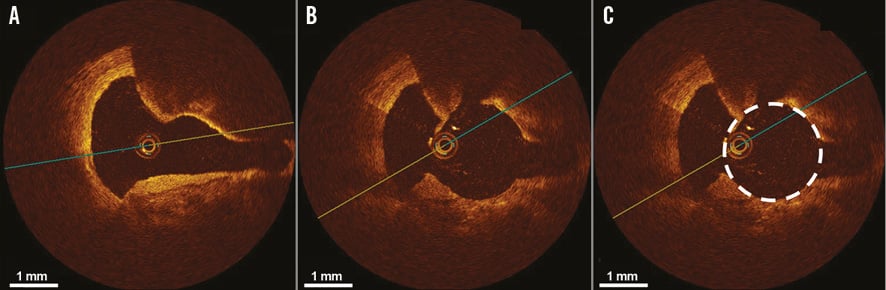
Figure 1. Calcified plaque ablated by rotational atherectomy visualised by optical coherence tomography. A) Optical coherence tomography (OCT) showing lumen narrowing with heavily calcified plaque before rotational atherectomy. After rotational atherectomy, the calcified segment ablated by a 2 mm burr (B) & (C) (dotted line indicates the size of the 2 mm burr).
OCT delineates calcified plaque without acoustic shadowing like intravascular ultrasound. Therefore, OCT is the best intracoronary imaging modality to select the appropriate burr size for RA and also to confirm the efficacy of RA after ablation.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Optical coherence tomography after rotational atherectomy clearly visualising ablated calcified plaque.
Supplementary data
To read the full content of this article, please download the PDF.
Optical coherence tomography after rotational atherectomy clearly visualising ablated calcified plaque.

