“If you prick us do we not bleed?” – William Shakespeare
Remarkable progress has been made over the last decade with strategies employed to mitigate bleeding in ST-elevation myocardial infarction (STEMI). Still, with advances in more potent pharmacotherapy and developments in sophisticated percutaneous coronary intervention (PCI) techniques (e.g., controlled antegrade and retrograde subintimal tracking/dissection re-entry for chronic total occlusion), bleeding remains a concern1. In recent years, this has become an integral focus in STEMI care, given the association between periprocedural bleeds and survival2,3. Moreover, haemorrhagic complications can lead to longer hospital stay (subjecting patients to nosocomial infection), recurrent cardiovascular events (e.g., subsequent myocardial infarction, stroke, arrhythmias, etc.), renal compromise and re-hospitalisation/re-admission with a direct impact on individual patients as well as healthcare resources2,4-6.
The controversy between culprit-only versus complete revascularisation in STEMI patients with multivessel disease has been recently studied, but clinical interpretation remains a challenge due to the inadequate power of small/moderate sized randomised studies7. The results from the Third Danish Study of Optimal Acute Treatment of Patients with ST-segment Elevation Myocardial Infarction Primary PCI in Multivessel Disease (DANAMI-3-PRIMULTI) trial (n=627 patients) found the primary endpoint of death/MI/revascularisation of a non-infarct-related artery (IRA) lesion reduced with staged in-hospital complete revascularisation compared to culprit-only PCI (without a difference in death/MI)8. With a second procedure performed as a staged approach, do bleeding events occur more commonly?
In this issue of EuroIntervention, Sadjadieh et al9 report a bleeding analysis from the DANAMI-3-PRIMULTI trial assessing the difference and outcomes of bleeding events in STEMI patients with multivessel disease receiving staged complete versus culprit-only revascularisation. Overall, the investigators found no difference in serious bleeding events between both groups enrolled in four experienced primary PCI centres in Denmark.
This is a well conducted secondary analysis examining bleeding events in the context of a clinical trial. In a STEMI population treated successfully undergoing culprit vessel PCI, it is conceivable that a staged complete revascularisation approach may lead to further bleeding events, particularly when vascular access needs to be re-established, recognising that patients are in the acute phase of STEMI on potent oral antiplatelets and that periprocedural anticoagulation needs to be re-administered. While it is reassuring that the current study shows no detrimental effects on Thrombolysis In Myocardial Infarction (TIMI) major/minor or Bleeding Academic Research Consortium (BARC) 3abc/BARC 5 bleeds, it should be noted that clinical trial patients are at lower risk of bleeding and may not be subjected to the same risk. In fact, within this trial, 66 patients were excluded from DANAMI-3 due to haemorrhagic diathesis, known coagulopathy, severe comorbidity/reduced life expectancy or severe renal insufficiency. Moreover, higher rates of “less significant” bleeds were demonstrated with staged complete revascularisation while in-hospital and in the long term.
Pre-procedural bleeding in STEMI has been difficult to define given various standardised definitions, with each being subject to criticism (Figure 1). TIMI and Global Use of Strategies to Open Occluded Coronary Arteries (GUSTO) definitions were extrapolated from fibrinolysis trials performed in the 1980s and 1990s. More contemporary definitions have focused on adjunctive pharmacotherapy with PCI and arguably have been more comprehensive in capturing other “clinically relevant” bleeds. However, the heterogeneity in definitions across STEMI trials has made it increasingly difficult to interpret bleeding results meaningfully. As such, the Bleeding Academic Research Consortium (BARC) definition was created to obviate these concerns and provide a consensus classification10. It is reassuring that the authors provide both TIMI and BARC definitions of non-CABG-related bleeding events in the current study. Although there appeared to be no difference in TIMI major/minor or BARC 3abc/5 bleeds with a staged complete versus culprit-only intervention, differences in minimal/medical and BARC 1/2 bleeds were noted, occurring in approximately 23% of patients receiving a second procedure. Although characterised as “less important” bleeds, these can lead to self-discontinuation of secondary prevention medications, which is an ongoing concern in “real-world” STEMI patients11. In addition, BARC 2 bleeds are not necessarily benign, as these events either require non-surgical medical intervention by a healthcare professional, lead to hospitalisation or an increased level of care, or prompt further evaluation10.
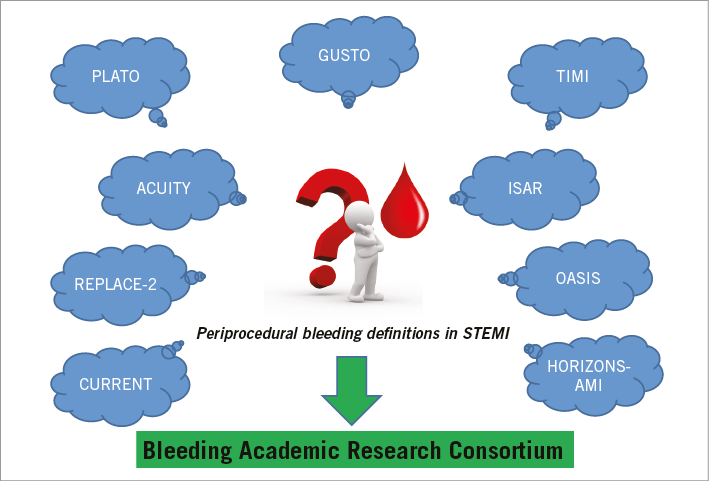
Figure 1. Reflect on various periprocedural bleeding definitions from clinical trials (blue clouds) or consider the Bleeding Academic Research Consortium (BARC) consensus definition (green arrow and box).
Of concern is the “crossover” rate of 26% in the culprit-only randomised patients. This may confound the bleeding risks associated with culprit-only intervention, leading to erroneous conclusions. However, the authors should be congratulated on performing an as-treated analysis, demonstrating similar findings to the intention-to-treat results showing no difference in TIMI major/minor or BARC 3abc/BARC 5 bleeds. While provocative, the results of the current study may not align with contemporary periprocedural management in STEMI. The majority of STEMI procedures were performed using femoral access, and in patients randomised to complete revascularisation the second procedure was again performed most commonly using femoral access (87%) with the contralateral femoral artery used infrequently (10%). In this setting, it is surprising that there were no differences in “significant” bleeds with a second procedure. This may reflect the expertise of four large-volume primary PCI centres enrolling in this study (proficient femoral operators) and may not be generalisable to all STEMI operators, especially those with lower procedural volume.
Roughly one in five patients received a glycoprotein IIb/IIIa antagonist at the time of the index PCI. Although in current practice this rate seems reasonable (particularly with more than half the patients receiving a more potent P2Y12 receptor antagonist in the current study), eptifibatide was the most commonly used agent. Eptifibatide has a relatively short half-life (roughly 2.5 hrs) compared to abciximab, an irreversible monoclonal antibody, where abnormal platelet function persists for up to seven days post infusion (only three patients received it in the current study). Given that the ACCF/AHA and ESC STEMI guidelines support abciximab as the preferred glycoprotein IIb/IIIa antagonist12, it is conceivable that a staged complete revascularisation approach could have resulted in more “complex” bleeds if abciximab had been utilised more frequently.
It is reassuring to note that the current study reaffirms the heightened bleeding risk associated with female gender. However, other well-established predictors of bleeding such as age, serum creatinine and vascular access were not predictors of bleeding events in STEMI. Certainly radial access should have protected against bleeding events, as has been demonstrated in prior randomised studies13. This was not demonstrated in the current study and is probably due to a “healthier” clinical trial patient population with lower than expected bleeding rates limited by the small number of patients enrolled in DANAMI-3-PRIMULTI.
Unfortunately, to date, we are limited by the small number of studies addressing differences in bleeding with a staged PCI approach in STEMI with multivessel disease. Although in the current analysis “significant” bleeds appear to be similar with culprit-only compared to staged multivessel PCI, firm conclusions cannot be substantiated due to the inherent pitfalls of a smaller RCT performed in a single country with established high-volume expertise in STEMI care. As such, the Complete versus Culprit-only Revascularization to Treat Multi-vessel Disease After Primary PCI for STEMI (COMPLETE) trial (ClinicalTrials.gov Identifier: NCT01740479) is an international, multicentre study which will randomise roughly 4,000 patients with multivessel disease who have undergone successful primary PCI to the culprit lesion to receive either staged PCI to the non-culprit lesion(s) or culprit-only intervention. The primary composite of cardiovascular death or new myocardial infarction at four years will be ascertained, with equal emphasis placed on capturing major and minor bleeding events for safety. Until then, we suggest being cautiously optimistic regarding the safety and efficacy of staged multivessel PCI in STEMI.
Conflict of interest statement
Both authors are on the steering committee for the COMPLETE trial.