Abstract
Aims: Treatment of the infarct-related artery only (IRA only) in ST-segment elevation myocardial infarction (STEMI) is associated with a significantly higher rate of ischaemia-driven revascularisation (ID-RV) during follow-up than fractional flow reserve-guided complete revascularisation (FFR-CRV). This study aimed to characterise all lesions which underwent ID-RV in the DANAMI-3-PRIMULTI trial with respect to location, stenosis grade and functional significance.
Methods and results: The study included 627 patients with STEMI and multivessel disease; 313 patients were randomised to treatment of the IRA only versus 314 undergoing staged FFR-CRV during the index admission. Rates of admission for suspected cardiac ischaemia (17%) were similar in both groups; however, ID-RV was significantly less frequent in the FFR-CRV group than in the IRA-only group (5% vs. 17%; p<0.001). In both groups, the primary reason for ID-RV was related to non-culprit, non-treated lesions (N=71/82 lesions in IRA-only; N=13/26 in FFR-CRV). De novo lesions or revascularisation of previously treated lesions were rarely causes of ID-RV. In the IRA-only group, there was a trend towards a higher ID-RV rate for lesions with a higher stenosis grade and located in more proximal segments – in particular, ≥80% stenosis of the left anterior descending and right coronary artery also led to angina class IV/unstable angina. In the FFR-CRV group, an FFR value ≤0.80 was shown to be an appropriate threshold for revascularisation.
Conclusions: FFR-CRV in STEMI is associated with a significantly lower rate of ID-RV at follow-up than treatment of the IRA only. This is due to a difference in non-culprit, non-treated lesions between both groups and not in de novo lesions or repeat revascularisation of previously treated lesions. Further considerations are warranted in case of high-grade non-culprit stenosis at proximal coronary segments, borderline FFR values and/or anticipated complex PCI.
Introduction
Primary percutaneous coronary intervention (PCI) is accepted as the standard of care for patients with ST-segment elevation myocardial infarction (STEMI). Over the past few years, different studies have shown the benefits of complete revascularisation of all angiographically or functionally significant lesions in STEMI patients presenting with multivessel disease, during either the index or a staged procedure1,2,3,4. In order to assess which non-culprit lesion(s) should be targeted by complete revascularisation, fractional flow reserve (FFR) has been suggested as an objective measure for the significance of a lesion5. The randomised, controlled DANAMI-3-PRIMULTI trial compared FFR-guided complete revascularisation (FFR-CRV) in STEMI with PCI of the infarct-related artery (IRA) only and showed significantly fewer ischaemia-driven revascularisations (ID-RV) during follow-up in the FFR-CRV group, whereas all-cause mortality and non-fatal reinfarction did not differ significantly between the groups3. This study aimed to characterise all lesions which underwent ID-RV in the DANAMI-3-PRIMULTI trial with respect to location, stenosis grade and functional significance.
Methods
STUDY DESIGN
The present study was performed as a post hoc analysis of the data collected during the DANAMI-3-PRIMULTI trial3. It was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee. All patients provided written informed consent.
The study included 627 patients with STEMI who underwent successful PCI of the culprit lesion within 12 hours from symptom onset and who had at least one additional ≥50% diameter stenosis in a non-infarct-related artery of more than 2.0 mm diameter. The grade of coronary artery stenosis was determined by visual interpretation. Patients were randomised to no further invasive treatment (PCI of the infarct-related artery only, IRA group: N=313) or to FFR-guided, staged complete revascularisation during index admission (FFR-CRV group: N=314). Complete revascularisation targeted all non-culprit lesions with an FFR value ≤0.80 or a visually assessed diameter stenosis ≥90% identified by repeat angiography. Lesions were treated by PCI, unless they were deemed unsuitable for PCI, in which case coronary artery bypass grafting (CABG) was considered.
The present analysis was conducted to characterise the lesions that were treated during ID-RV, as well as the timing and urgency of ID-RV. Assessed lesion characteristics included the lesion status at the initial treatment (treated culprit lesion, treated or non-treated non-culprit lesion, or de novo lesion not identified at the index procedure), lesion location, angiographic diameter stenosis (%) and FFR value at the initial treatment, if available.
DEFINITIONS
Patients were followed after the index procedure and ID-RV during follow-up was performed when required. ID-RV, which was a secondary endpoint of the DANAMI-3-PRIMULTI study, was defined as any coronary revascularisation on the basis of either angina pectoris, a positive non-invasive ischaemia test, or both. The Canadian Cardiovascular Society (CCS) grading system was used to gauge angina symptom severity; there was no recommendation for routine non-invasive ischaemia testing during follow-up. Urgent revascularisation was defined as revascularisation during admission for any acute coronary syndrome (ACS), both unstable angina and troponin-positive ACS3.
STATISTICS
Descriptive statistics were expressed as median and interquartile range (IQR) for continuous variables and as frequency and percentage (%) for discrete variables. The differences in continuous variables between groups were determined using the Student’s t-test or Wilcoxon rank-sum test, whereas the chi-square test or Fisher’s exact test was used to test for associations between discrete variables. A two-tailed p-value <0.05 was considered to indicate statistical significance. Statistical analyses were performed using SPSS software, Version 23.0 (IBM Corp., Armonk, NY, USA).
Results
STUDY POPULATION
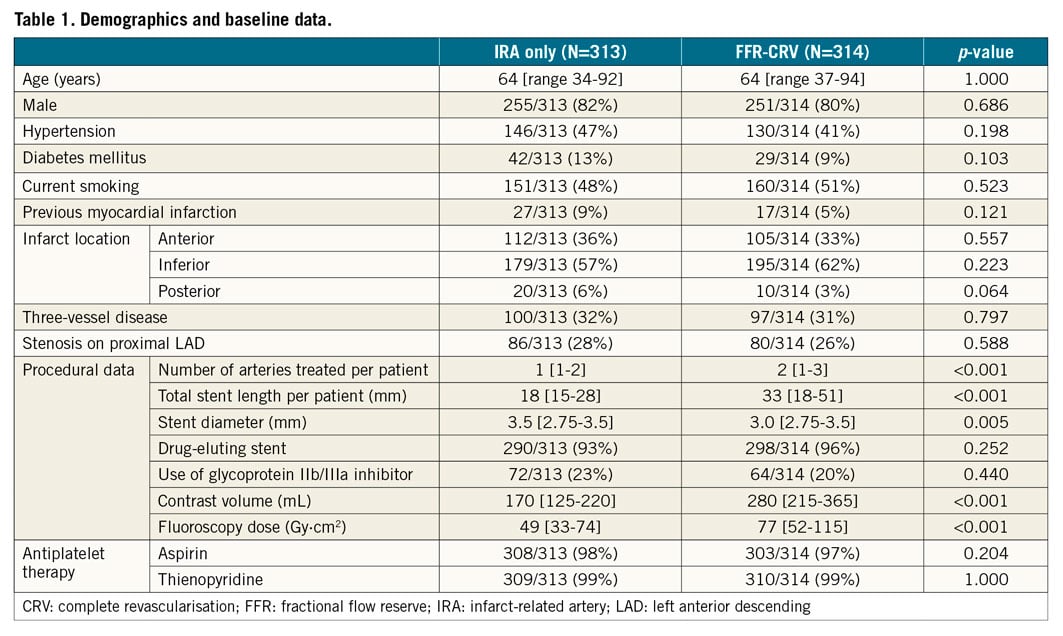
The baseline data of both groups are provided in Table 1. Except for parameters with differences inherent to the randomised treatment, no significant differences were found between the groups.
SUSPECTED CARDIAC ISCHAEMIA AND ID-RV AT FOLLOW-UP
In total, 107 patients were admitted because of suspected cardiac ischaemia at follow-up, involving 54 patients (17%) in the IRA-only group and 53 patients (17%) in the FFR-CRV group (Figure 1). The major reason to suspect cardiac ischaemia in both groups was angina CCS class II (N=66). A total of nine patients (3%) were admitted because of angina class IV or unstable angina in the IRA-only group, whereas no single patient in the FFR-CRV group presented with this degree of angina (N=0; p=0.007). The rate of troponin-positive ACS was not different between the groups (Figure 1B).
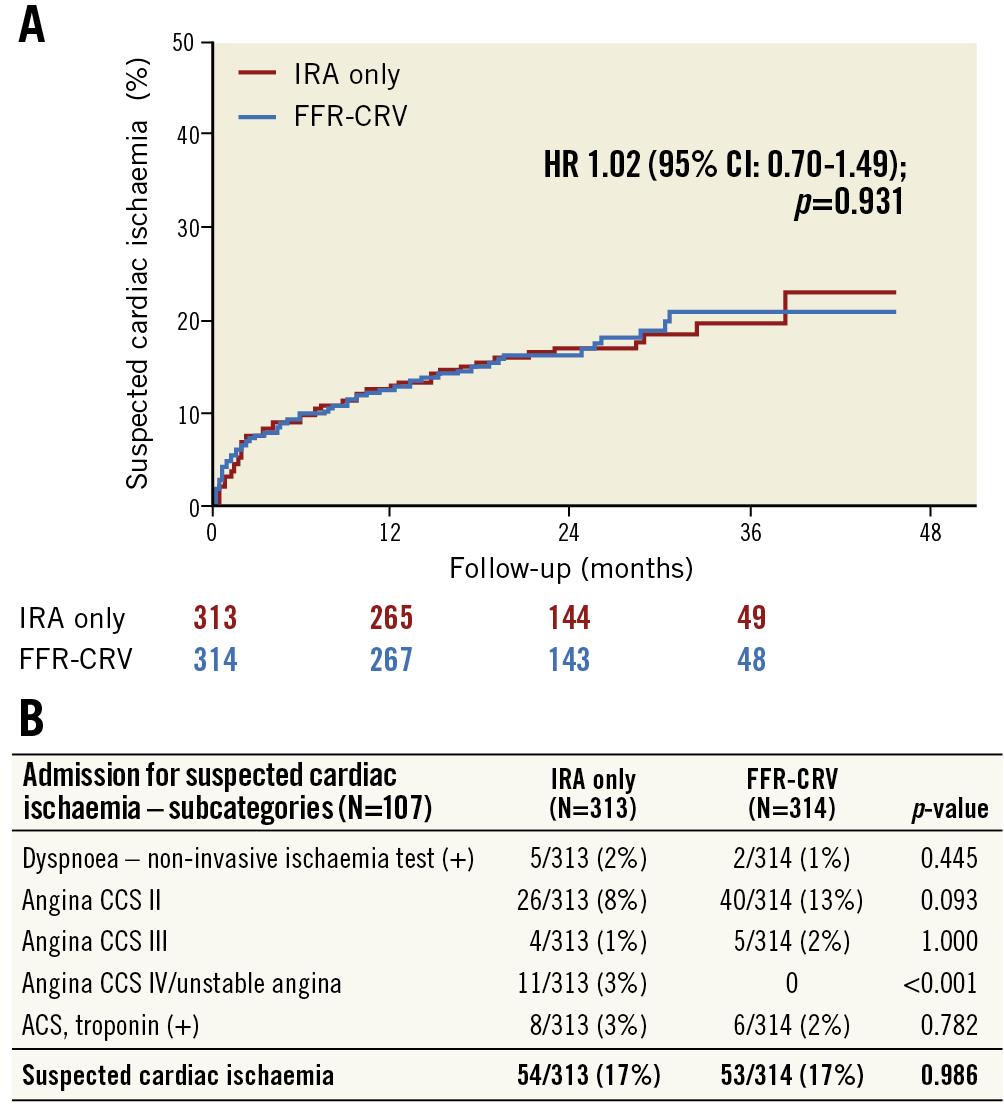
Figure 1. Admission for suspected cardiac ischaemia during follow-up in the DANAMI-3-PRIMULTI trial. A) Cumulative incidence curves for both study groups. B) Analysis of the different causes leading to suspicion of cardiac ischaemia. The Canadian Cardiovascular Society (CCS) grading system was used to gauge angina symptom severity. ACS: acute coronary syndrome; FFR-CRV: fractional flow reserve-guided complete revascularisation; HR: hazard ratio; IRA: infarct-related artery
The strategy of FFR-CRV during the index admission was associated with a significantly lower rate of ID-RV at follow-up as compared to the IRA-only approach (N=17; 5% vs. N=52; 17%, respectively; p<0.001) (Figure 2). Both urgent and non-urgent PCI were more frequently performed in the IRA-only group than in the FFR-CRV group (Figure 2B). The timing of these ID-RVs is shown in Figure 3, revealing that more than 70% of all revascularisations were performed within the first 18 months following the index admission in both groups.
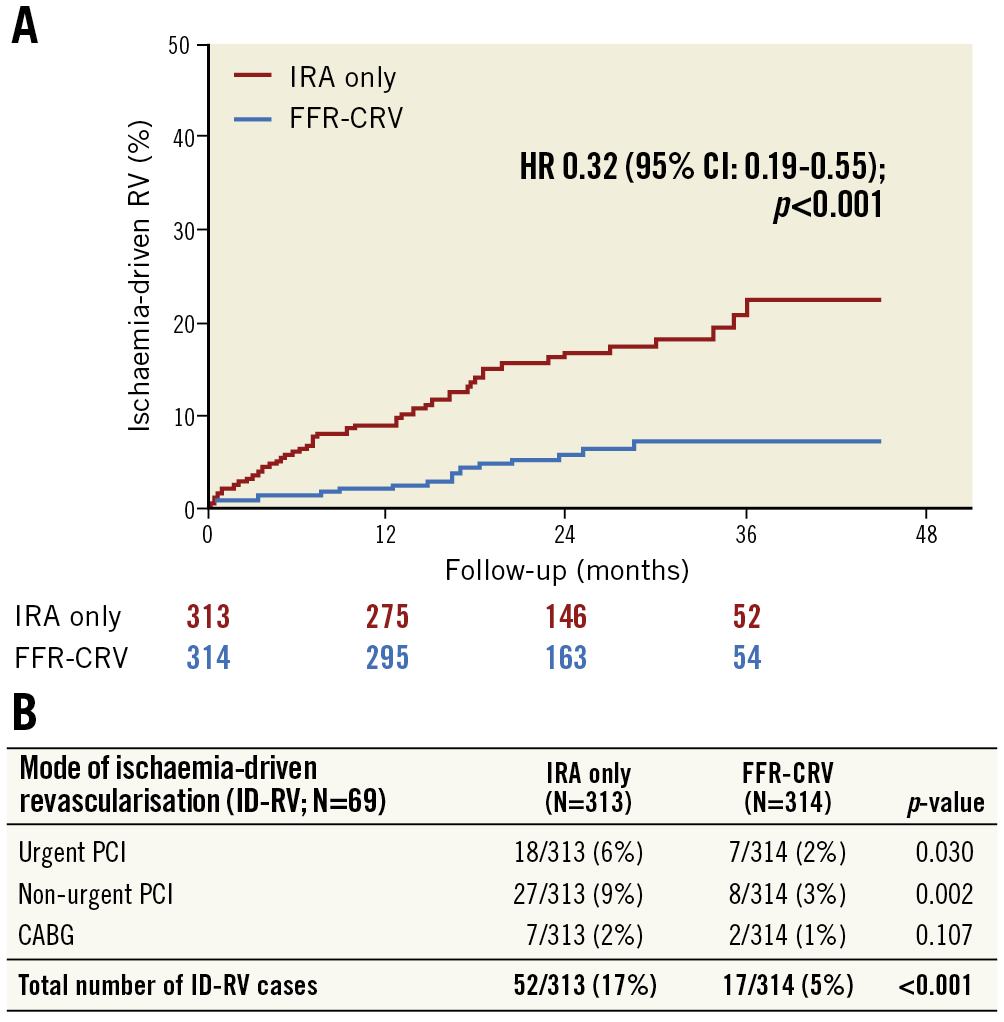
Figure 2. Ischaemia-driven revascularisation (ID-RV) during follow-up in the DANAMI-3-PRIMULTI trial. A) Cumulative incidence curves for both study groups. B) Mode and urgency of ID-RV during follow-up in both study groups. CABG: coronary artery bypass graft; FFR-CRV: fractional flow reserve-guided complete revascularisation; HR: hazard ratio; IRA: infarct-related artery; PCI: percutaneous coronary intervention
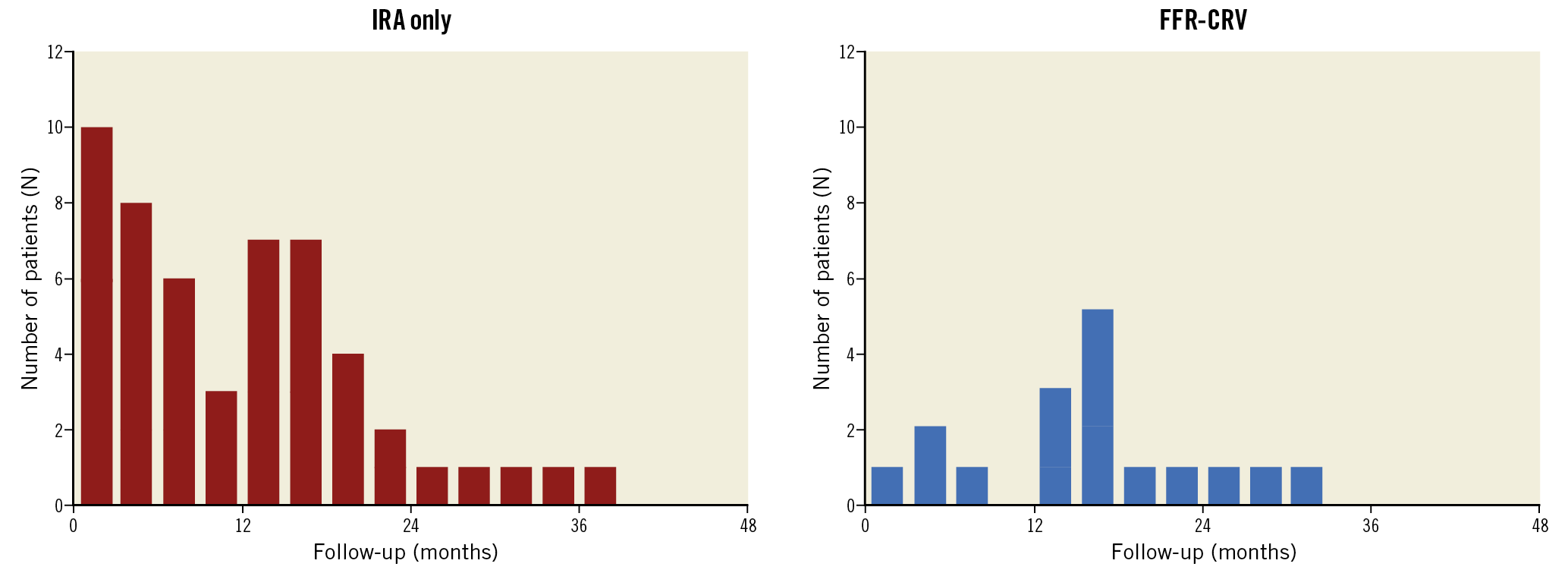
Figure 3. Timing of ischaemia-driven revascularisation (ID-RV; N=69) involving treatment of non-culprit lesions not treated at the index admission, according to protocol. FFR-CRV: fractional flow reserve-guided complete revascularisation; IRA: infarct-related artery
Among all patients undergoing ID-RV (N=69) in this study, 108 lesions were finally revascularised – 82 lesions in the IRA-only group and 26 lesions in the FFR-CRV group (Figure 4). Only a small number of lesions were de novo, not previously identified lesions (N=8 in the IRA-only group vs. N=7 in the FFR-CRV group). Reintervention of previously treated (non)-culprit lesions was rare in both groups. ID-RV most frequently targeted non-culprit lesions that were left untreated at the index admission, with a randomisation-driven larger number of such lesions in the IRA-only group (N=71) than in the FFR-CRV group (N=13) (Figure 4).
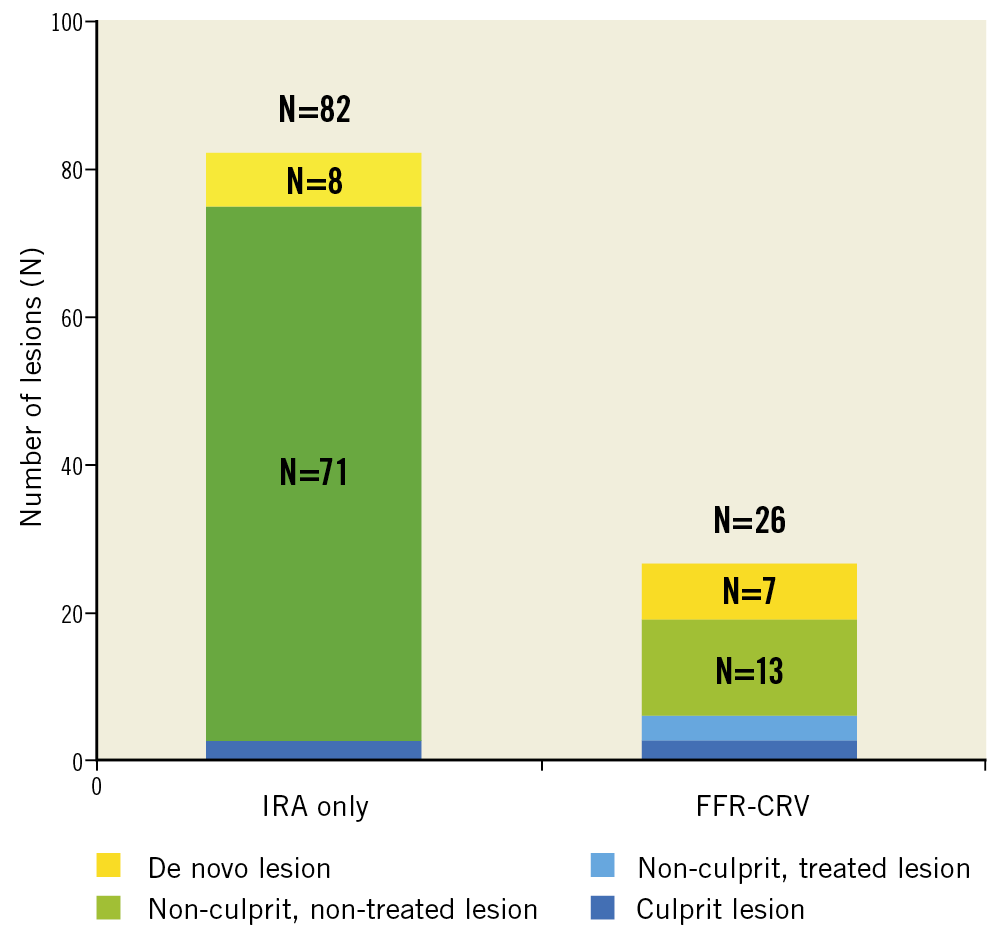
Figure 4. In-depth analysis of all lesions that were revascularised during follow-up in the DANAMI-3-PRIMULTI trial (N=108 lesions in 69 patients), indicating the lesion status at the initial time of randomisation: de novo lesion not identified at the index procedure, non-treated or treated non-culprit lesion, or initially treated culprit lesion. FFR-CRV: fractional flow reserve-guided complete revascularisation; IRA: infarct-related artery
LESION CHARACTERISTICS
In the IRA-only group, ID-RV involved a total of 71 non-culprit lesions that were initially not treated per protocol. The proportion of non-culprit lesions that underwent ID-RV during follow-up was rather similar across various coronary artery segments (Figure 5). Nevertheless, there was a trend towards a higher ID-RV rate of non-culprit lesions in case of a higher stenosis grade and involvement of a more proximal segment (Figure 5A). In particular, ≥80% stenosis of the left anterior descending (LAD) and right coronary artery (RCA) could lead to angina class IV or unstable angina (N=8) (Figure 5B).
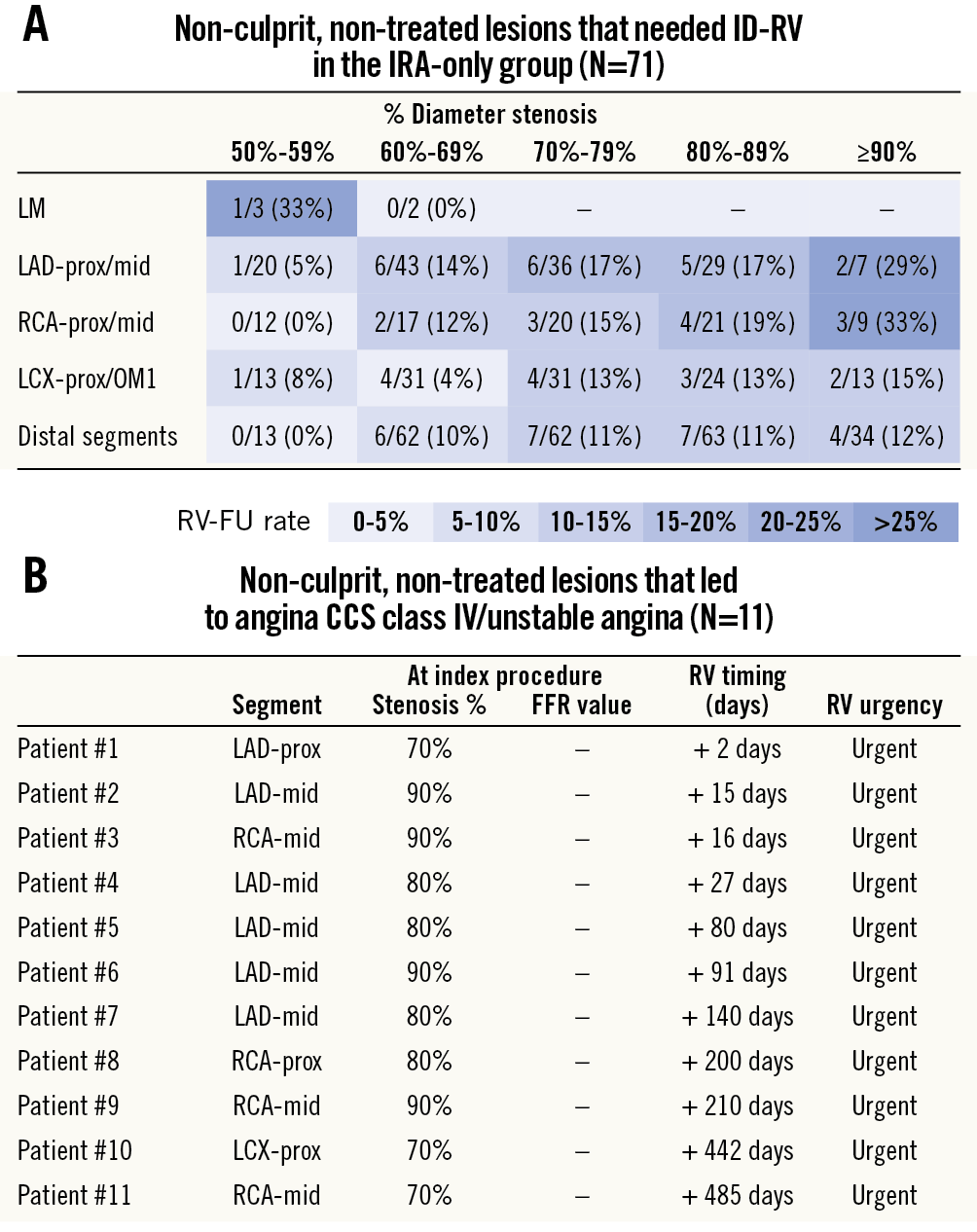
Figure 5. Lesion characteristics of non-culprit, non-treated lesions that were revascularised during follow-up in the IRA-only group (n=71). A) Percentages represent the proportion of all lesions at a specific location (and with a specific % stenosis grade) that were treated during follow-up. B) List of all non-culprit, non-treated lesions that led to angina CCS class IV/unstable angina and urgent ischaemia-driven revascularisation in the IRA-only group (N=11).
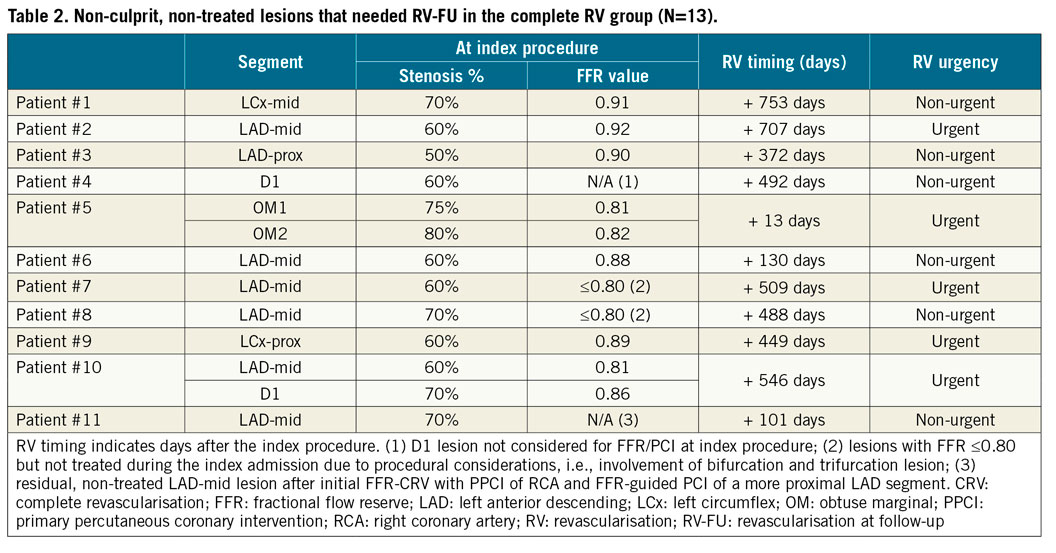
In the FFR-CRV group, ID-RV involved a total of 13 non-culprit lesions that were left untreated during the index admission (Table 2). Two patients were not treated at the index admission due to procedural considerations, although the FFR value at that time was ≤0.80 (patients #7 and #8). One other patient in whom borderline FFR values (0.81-0.82) were measured in obtuse marginal (OM) branches was not revascularised at the index admission; however, the patient was admitted two weeks later with angina CCS class III leading to PCI of these lesions. Importantly, the majority of patients were revascularised beyond one year after the index admission (N=8/11) (Table 2).
PROGRESSION TO MORE COMPLEX LESIONS IN THE IRA-ONLY GROUP
An example of a patient, randomised to the IRA-only group, is shown in Figure 6. At primary PCI, an acute occlusion of the left circumflex artery was opened and a drug-eluting stent was implanted. Per randomisation, stenoses in the mid-LAD and posterior descending artery (PDA) were left untreated. At 274 days after the index procedure, the patient was admitted because of unstable angina pectoris. Angiography showed further progression of non-culprit lesions into a 90% mid-LAD stenosis and complete occlusion of the PDA. Because of this two-vessel disease involving a LAD bifurcation and a chronic total PDA occlusion, CABG was considered the best therapeutic choice for this patient.
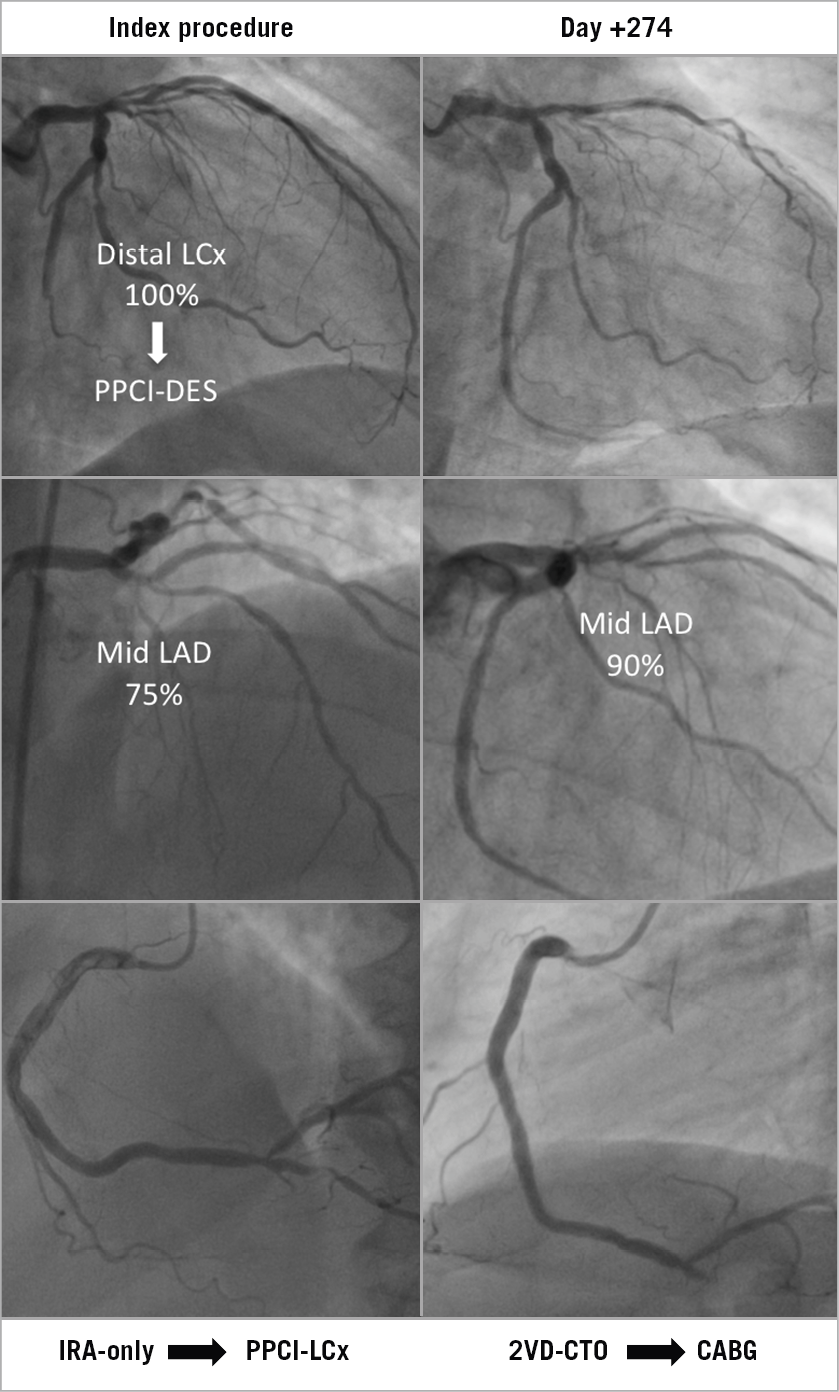
Figure 6. Example of a STEMI patient with an occluded distal LCx artery randomised to IRA-only treatment who required CABG at 274 days after initial treatment. Angiographic images at PPCI (left) and at follow-up (right) are shown. CABG: coronary artery bypass graft; IRA: infarct-related artery; LAD: left anterior descending artery; LCx: left circumflex artery; PPCI: primary percutaneous coronary intervention
Discussion
The present analysis of data from the DANAMI-3-PRIMULTI trial provides further insight into the lesions that led to ID-RV in this STEMI population. As reported in earlier publications from this trial3,6, the rate of ID-RV was significantly lower in patients who underwent FFR-guided complete revascularisation (FFR-CRV) as compared to those receiving no further initial treatment. In-depth analysis shows that this difference can be fully ascribed to the non-culprit lesions that were left untreated during the index admission in the IRA-only group. Repeat revascularisation rates of culprit and non-culprit lesions, treated during index admission, as well as the incidence rates of de novo lesions were low and similar among the randomisation arms – indicating that FFR-CRV with a 0.80 cut-off value can be considered safe and efficacious.
The DANAMI-3-PRIMULTI trial found a significantly lower incidence of the composite of all-cause mortality, reinfarction and repeat revascularisation in patients undergoing complete revascularisation as compared to those with treatment of the IRA only3. This reduction was driven by a difference in revascularisation rates, while mortality and reinfarction were not significantly different between the treatment groups. A post hoc analysis of the DANAMI-3-PRIMULTI data showed that the reduction in the composite endpoint was most pronounced in patients with three-vessel disease combined with non-culprit lesions with ≥90% diameter stenosis6. Our findings are complementary to the results of this earlier post hoc analysis. In particular, they suggest that the decision to treat non-culprit lesions is safe and with documented good outcome. In addition, more nuanced considerations beyond a strict application of the study criteria for revascularisation – inevitably required within the setting of a clinical trial – may be needed in daily clinical practice.
In patients randomised to FFR-CRV, only three out of 314 patients (1%) needed ID-RV of non-culprit, non-treated lesions within one year after the index admission. This finding suggests that an FFR threshold of 0.80 provides adequate guidance for treatment of non-culprit lesions. However, with eight patients undergoing revascularisation more than one year after the initial treatment, it should be acknowledged that FFR in a STEMI setting might not reliably indicate the need for intervention in the medium to long term.
Another observation in this study is that there were hardly any repeat revascularisations of treated, non-culprit lesions (only 2/246 lesions; 0.8%) in the patient cohort randomised to FFR-CRV. This confirms the high safety and success rates reported in prior trials studying complete revascularisation in STEMI1,2,4. Whether the applied staged approach for complete revascularisation in the DANAMI-3-PRIMULTI trial has further contributed to these excellent outcomes is a matter of speculation.
In the context of this study, it is also important to note that true “complete revascularisation” was not obtained in 20 patients in the FFR-CRV group. In 15 patients, treatment with PCI of an FFR-positive lesion was not performed as the operator evaluated the lesion as being too complex and/or too high-risk for PCI and at the same time not eligible for CABG. This underlines that further consideration is warranted regarding treatment of non-infarct-related lesions – especially in case of complex lesions and/or borderline FFR values – and that the decision to perform additional revascularisation in a STEMI setting should not just depend on one isolated FFR value. Other factors such as the operator’s judgement of the technical feasibility of the intervention and overall risk/benefit ratio for the patient (e.g., renal dysfunction, bleeding diathesis, thrombosis risk) should also be taken into consideration.
Although an FFR-CRV approach has been shown to be associated with a significantly lower rate of ID-RV as compared to angiography-guided complete revascularisation – both in stable angina as well as in the setting of acute coronary syndrome7,8 – the use of FFR in a STEMI setting is not always that practical or feasible. Operators could be concerned about prolongation of the index procedure, use of more contrast dye, or unreliable FFR measurements in this acute phase. The staged approach of primary PCI and FFR evaluation of non-culprit lesions (as applied in this study) and/or the use of novel non-hyperaemic indices of coronary artery stenosis severity can be a solution. However, bringing back all STEMI patients with multivessel disease to the catheterisation laboratory for additional FFR measurements in a systematic way will not be feasible in many centres outside a clinical trial. Therefore, it is still interesting to study the IRA-only group in more detail and investigate which lesions led to (urgent) ID-RV in the DANAMI-3-PRIMULTI trial – as was done in this study.
In STEMI patients with treatment of the IRA only, non-culprit lesions were more likely targets for ID-RV when located in the proximal/mid-LAD and RCA segments and when they had a relatively high stenosis grade at initial angiography. Although FFR values of such lesions were not assessed, it may be speculated that FFR would have classified many of these high-grade stenoses as functionally significant9. In particular, ≥80% stenosis of the LAD and RCA left untreated in the IRA-only group led to angina class IV/unstable angina and urgent RV in eight patients, whereas no single patient in the FFR-CRV group presented with this degree of angina. Importantly, one of the patients in the IRA-only group developed a third-degree AV block and in-hospital cardiac arrest a few hours after PCI of a LAD culprit lesion; a residual 90% RCA lesion was left untreated. Consequently, we believe that a more complete revascularisation than IRA only should be considered during the index procedure in case of a high-grade (≥90%) non-culprit stenosis with a large distal supply area.
Although complete revascularisation has been shown to be beneficial and revascularisation of non-culprit lesions is recommended by current guidelines10, a recent large PCI registry showed that 78% of STEMI patients underwent incomplete revascularisation11. The same study reported an increased mortality among STEMI patients who had incomplete revascularisation of two or more vessels or of the LAD. In all patients undergoing PCI, incomplete revascularisation of a vessel with ≥90% stenosis also resulted in a higher risk, although this effect was not significant for STEMI patients only. These findings are consistent with the observations from the DANAMI-3-PRIMULTI trial and indicate the need for careful consideration when treating additional non-culprit lesions in STEMI patients with multivessel disease.
Finally, an interesting observation of this substudy is that ID-RV by CABG was undertaken in seven patients (2.2%) in the IRA-only group vs. only in two patients (0.6%) in the FFR-CRV group (p=0.107). Statistical significance was not reached due to the low incidence rate and a lack of statistical power. In Figure 4, a case example illustrates the potentially negative consequence of incomplete revascularisation: (1) progression of a borderline stenosis into a complex bifurcation lesion, and (2) progression of a high-grade stenosis into a chronic total occlusion. This observation suggests that revascularisation of non-culprit lesions could also be considered if lesions are likely to progress into complex lesions – even in case of a negative, borderline FFR value – or in case of a critical lesion likely to progress into a chronic total occlusion. Although this may not significantly reduce the incidence of hard endpoints such as mortality and reinfarction, we consider it beneficial from a patient’s perspective to avoid ID-RV. This is particularly true if non-culprit, non-treated lesions are likely to progress into complex lesions requiring CABG in the future.
Limitations
A limitation of this analysis, inherent to the protocol of the DANAMI-3-PRIMULTI trial, is the fact that FFR values in non-culprit lesions were not determined in patients randomised to IRA only. We can therefore only speculate how many non-culprit lesions in these patients would have qualified for revascularisation based on their FFR value. On the other hand, for most of the high-grade stenosis (≥90%), it is likely that FFR would have shown the stenosis to be functionally significant4. Another limitation of this study is that data on functional significance (FFR values) were most of the time not available at the time of ID-RV. Finally, our observations are based on a single cohort with a specific risk profile and may not be extrapolated to other populations with different risks for mortality and reinfarction.
Conclusions
Treatment of the IRA only in STEMI is associated with a significantly higher rate of ID-RV as compared to an FFR-CRV approach – this can be ascribed entirely to the non-culprit lesions that were left untreated in the IRA-only group. Repeat revascularisation rates of culprit and non-culprit lesions – treated during index admission – as well as the incidence rates of de novo lesions were very low in both groups, indicating that FFR-CRV in STEMI can be considered safe and efficacious. Higher vigilance is recommended in case of high-grade non-culprit stenosis at more proximal coronary segments, borderline FFR values and/or anticipated complex PCI.
|
Impact on daily practice Treatment of the IRA only in STEMI is associated with a significantly higher rate of ischaemia-driven revascularisation than FFR-guided complete revascularisation. This is due to a difference in non-culprit, non-treated lesions between the groups. In the FFR group, an FFR value ≤0.80 was shown to be an appropriate threshold for revascularisation; however, further consideration is warranted in case of borderline FFR values and/or anticipated complex PCI. |
Funding
Danish Agency for Science, Technology and Innovation and Danish Council for Strategic Research.
Conflict of interest statement
The authors have no conflicts of interest to declare.

