Introduction to the session: the trial headlines
The aim of the article is to capture the session at EuroPCR 2017 covering the Compare-Acute trial, communicate the analysis of the trialists, and report the views expressed in the interactive discussion. This article does not constitute an independent review of the topic by the authors.
The objective of the “Will this trial change my practice?” session was to discuss the Compare-Acute randomised trial and the extent to which it would probably change clinical practice1. The trial headlines were outlined succinctly by P.L. L’Allier. Among patients with ST-segment elevation myocardial infarction (STEMI) and multivessel disease undergoing primary percutaneous coronary intervention (PCI) of an infarct-related artery, those patients who underwent fractional flow reserve (FFR)-guided complete revascularisation of non-infarct-related arteries in the acute setting, as compared to those who were treated for the infarct-related artery only, had a lower risk of the composite cardiovascular outcome of death from any cause, non-fatal myocardial infarction (MI), any revascularisation, and cerebrovascular events at 12 months (Figure 1). This finding was mainly supported by a reduction in subsequent revascularisations (5.1% versus 16.6%, p<0.001).
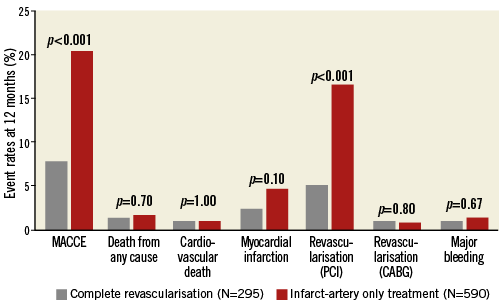
Figure 1. Endpoints at 12 months. MACCE denotes the composite of all-cause mortality, non-fatal myocardial infarction, any revascularisation, and cerebrovascular events. CABG: coronary artery bypass graft surgery; PCI: percutaneous coronary intervention
Case presentation: how should I treat?
To provide a clinical context for the subsequent discussion, F-J. Neumann presented a case that was in the Compare-Acute study. A 61-year-old male presented with an acute anterior STEMI and was randomised to the infarct-related artery only treatment arm. After successful PCI of the left anterior descending artery, as per trial protocol, he underwent FFR measurement of a right coronary artery (RCA) stenosis2. The FFR result was, as per protocol, concealed from the operator and the patient. He was started on guideline-recommended medications and discharged well.
As per standard clinical practice at his institution, the patient underwent exercise stress echocardiography one month after the STEMI presentation. Because the stress test reported significant ischaemia, he proceeded with PCI to the RCA. This PCI procedure was not counted as an endpoint event as per trial protocol. The patient remains well at his latest clinic visit three years after the index event.
“What is common practice?” discussion
The case presentation successfully set the scene for a lively discussion about current clinical practice. The panel and the audience were divided in their opinions as to whether they would have performed PCI of the RCA in the acute setting and, if not, what would be the optimal timing for a staged PCI. The issue of lesion complexity was debated – would it be reasonable to prolong a primary PCI procedure to perform PCI for a complex lesion or would the patient, considering that these were stable lesions, be better served by a strategy of early staged PCI? To what extent would knowing the degree of ischaemia influence this decision? Also, the safety of performing multivessel FFR during a primary PCI was discussed, as was the clinical applicability of its findings in the acute STEMI context.
Background: what was known before the trial?
The issues raised in the discussion following the case presentation presented a perfect platform for T. Engstrøm to outline the background for the Compare-Acute study. We know that, among patients presenting with STEMI, as many as 50% will have multivessel coronary artery disease3,4. Previously, there was a paucity of data to guide treatment and therefore ESC guidelines as recently as 2014 recommended a strategy of primary PCI limited to the culprit vessel, with consideration of staged revascularisation of the non-culprit vessels in the context of symptoms or demonstrable ischaemia5.
However, recent studies have suggested alternative strategies. The Preventive Angioplasty in Acute Myocardial Infarction (PRAMI) trial reported that patients who had “preventive” or “complete” revascularisation during primary PCI had a significantly reduced risk of adverse cardiovascular outcomes, as compared to patients who had PCI limited to the infarct artery6. In PRAMI, patients randomised to the infarct artery arm were permitted to have PCI of the non-infarct vessels only if they had refractory angina with objective evidence of ischaemia. These findings were echoed by the Complete versus Lesion-only Primary PCI (CvLPRIT) trial where patients who had complete revascularisation, as opposed to those who had culprit-artery only PCI, had a lower risk of adverse events within 12 months7. The subtle yet important difference between PRAMI and CvLPRIT was that, in the former, complete revascularisation was performed exclusively during primary PCI, whereas in CvLPRIT staged PCI during the same index hospitalisation was permitted. This therefore raises the issue of optimal timing to complete revascularisation.
The DANAMI-3—PRIMULTI study examined a strategy of FFR-guided PCI during the same hospital admission versus optimal medical therapy only, and reported a significantly reduced risk of future events among patients randomised to the former arm8. This benefit was driven by significantly fewer repeat revascularisations. Importantly, at least half of these repeat revascularisations were performed for acute coronary syndromes.
The issue of the reliability of FFR measurements in the acute MI setting was outlined. Because the coronary microcirculation is jeopardised during an acute MI, the value of FFR measured may differ from that in a more stable setting (smaller flow increase, yet underestimated FFR for any stenosis severity). The limited data available suggest that this may not be a significant issue, but there is still an element of uncertainty as to the generalisability of previous FFR studies in the acute MI setting to guide revascularisation at least in the culprit vessel9.
Hence, the potential importance and relevance for the Compare-Acute trial as a trial to examine FFR-guided revascularisation during the acute primary PCI setting was established.
Trial analysis: summary of the trialists’ critical review
To begin his in-depth and critical review of the trial methodology, results, and conclusions, P. Jüni reminded the panel and the audience that Compare-Acute was a strategy trial, which compared a strategy of early FFR-guided PCI of non-culprit lesions predominantly in patients with FFR ≤0.80 versus a strategy of deferred PCI of non-culprit lesions in selected patients independently of FFR.
The Compare-Acute trial was an investigator-initiated, industry-supported, international, randomised trial designed to demonstrate superiority. In total, 885 patients with STEMI and multivessel disease (with non-infarct-related lesions for which FFR and PCI were deemed appropriate) were randomised by the use of opaque envelopes in a 1:2 fashion to FFR-guided complete revascularisation, or infarct-artery only revascularisation and concealed FFR measurement of non-infarct-artery lesions. P. Jüni commented that it was unclear whether allocation envelopes were sealed and sequentially numbered; therefore, selection bias introduced by potentially inadequate concealment of allocation could not be entirely excluded. Still, he considered that this was unlikely to have affected results to a major extent.
The primary outcome of the trial was a composite of all-cause mortality, non-fatal MI, any revascularisation, or cerebrovascular event at 12 months. Revascularisations were evaluated by an independent clinical evaluation committee with regard to need and indication. With an estimated 14.5% event rate in the control group, and a 3% loss of follow-up, a sample size of 885 patients would yield 80% power to detect a 45% relative risk reduction with the experimental strategy at a two-sided alpha of 5%.
Of the 295 patients randomised to the FFR-guided experimental arm, 163 (55.3%) had PCI to non-infarct-related coronary artery lesions (Figure 2). The majority (83.4%) of these interventions were performed during the index PCI procedure, with the rest performed during the index hospitalisation. In the control arm, 57 patients had PCI performed within 45 days of the index event. These were considered staged PCI procedures, and were not counted in the final adjudication of the primary outcome. Of these 57 patients, 44 patients had PCI performed for lesions that were significant by FFR in the initial index assessment.
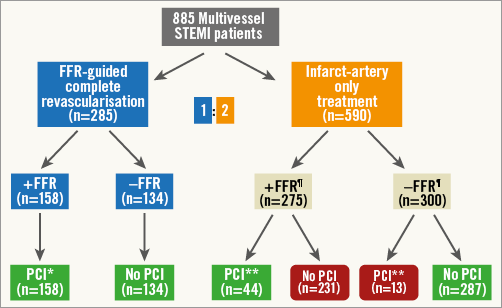
Figure 2. Study population. FFR: fractional flow reserve; FFR¶: FFR procedure with blinded result for treating physicians; PCI: percutaneous coronary intervention; PCI*: FFR-guided PCI of non-infarct-related arteries performed during primary PCI procedure (83%) or within 72 hours after primary PCI procedure (17%); PCI **: staged PCI performed of non-infarct-related arteries within 45 days after primary PCI procedure; STEMI: ST-segment elevation myocardial infarction
P. Jüni therefore emphasised again that the trial compared a strategy of early FFR-guided PCI of non-culprit lesions versus a strategy of deferred PCI of non-culprit lesions in selected patients. Compare-Acute should not be interpreted as a comparison of FFR-guided PCI of non-culprit lesions versus PCI without FFR guidance, of same session PCI versus staged PCI of non-culprit lesions, or even as PCI of non-culprit lesions versus conservative treatment of these lesions.
Nevertheless, the trial reported a significant reduction in the risk of experiencing the primary composite endpoint among patients in the complete revascularisation versus infarct-artery only treatment arms (hazard ratio [HR] 0.35, 95% confidence interval [CI]: 0.22-0.55) (Figure 1). The difference was driven mainly by the greater number of revascularisations in the latter group (HR 0.32, 95% CI: 0.20-0.54). There was no statistical difference among the groups with regard to death from any cause or non-fatal MI, even though there was a non-significant 50% relative risk reduction in MI, which had contributed to the observed difference in the primary composite endpoint, and a formally significant 66% relative risk reduction of revascularisation triggered by an acute coronary syndrome.
As such, P. Jüni concluded his critical review by suggesting that the trial conclusions should be tempered to state that “among patients presenting with STEMI and multivessel disease, FFR-guided complete revascularisation of non-infarct-related lesions in the acute phase of primary PCI reduced the risk of a composite cardiovascular outcome as compared with an initial strategy of treatment of the infarct-related artery only”. Even though this reduction was mainly driven by the decreased need for subsequent revascularisation, a numeric decrease in MI and a significant decrease in revascularisations triggered by an acute coronary syndrome suggested that the experimental strategy could also be associated with an advantage in clinical outcomes that were “harder” than just revascularisations.
“Will this trial change my practice?” discussion
F-J. Neumann then provided the conclusion to the case that he had presented earlier. As the FFR of the non-culprit lesion was significant when measured at the time of the index event, in retrospect this was considered an appropriate staged PCI. He then showed a series of hypothesis-generating results that could be inferred from the published trial manuscript.
Patients with an appropriate revascularisation strategy (defined as having FFR-guided PCI or no PCI), as compared to those with an inappropriate strategy (having no PCI when FFR-positive, or PCI when FFR-negative), had a reduced risk of experiencing the primary composite endpoint, once again driven mainly by unplanned revascularisation.
He also showed that, in the Compare-Acute trial, the chance of having an appropriate revascularisation strategy in the infarct-artery only treatment arm was about 50% (Figure 2). Furthermore, within the infarct-artery only group, only 16% of patients with FFR-positive lesions underwent elective staged PCI. These relatively low proportions imply that the use of stress testing as per current clinical practice has the potential to undertreat patients appropriately as opposed to when FFR is used routinely. Of concern, he also showed that in the Compare-Acute study those patients in the infarct-artery only group who had FFR-significant lesions, yet did not undergo elective staged PCI, had a significantly higher event rate as compared to patients who had PCI for FFR-significant lesions. This result was once again mainly driven by an excess of unplanned revascularisations.
He concluded his analysis by stating that the goal of primary PCI should also include achieving appropriate revascularisation of non-culprit lesions. He opined that FFR guidance enabled appropriate revascularisation during the primary intervention, and that, without FFR guidance, the likelihood of an appropriate revascularisation strategy is reduced.
The Chairperson’s conclusion: where do we stand now?
Thereafter, a lively discussion ensued where the issues raised by the trial were put forth. First, the importance of repeat revascularisation as an endpoint was debated. The consensus of the panel was that, although clinically it may not appear to be as high impact as mortality, repeat revascularisation is a significant event for a patient because it is frequently due to a change in clinical condition and also involves the attendant risks of the procedure, and time and possibly financial costs. Furthermore, it was opined that repeat revascularisation is not such a benign event because upwards of 50% of patients will undergo the repeat procedure due to an acute coronary syndrome event.
Next, the issue of optimal timing for staged PCI was discussed again. It was highlighted that, while current data are insufficient to guide practice, there exist ongoing and planned studies that should hopefully shed some light on this important issue in the future.
With regard to safety, despite two adverse events, including a death, that were directly attributable to the FFR procedure, the panel felt that this study involving 885 participants demonstrated the relative safety and feasibility of performing multivessel FFR in the acute MI setting.
Finally, the Chairperson, G. Olivecrona, concluded the session by summarising the issues raised and discussion points. In his opinion, the Compare-Acute trial would change his clinical practice – he would much more readily perform FFR of non-culprit lesions in STEMI patients directly following PCI of the culprit vessel, and he would feel much more comfortable now to perform PCI of non-culprit lesions during the index primary PCI procedure. The panel endorsed his opinion and the session concluded.
| Summary The Compare-Acute trial demonstrates the relative safety and utility of performing multivessel FFR to examine the significance of non-culprit lesions during primary PCI. Patients who had an FFR-guided PCI strategy for non-culprit lesions during the index hospitalisation had fewer adverse cardiovascular events, essentially unplanned revascularisations, as compared to patients who were treated for the infarct-related artery only. |
Conflict of interest statement
F-J. Neumann has received grants from St. Jude and Abbott Vascular. T. Engstrøm has received a speaker’s fee from St. Jude Medical. P. Jüni has received research grants to the institution from AstraZeneca, Biotronik, Biosensors International, Eli Lilly and The Medicines Company, and serves as unpaid member of the steering group of trials funded by AstraZeneca, Biotronik, Biosensors, St. Jude Medical and The Medicines Company. The other authors have no conflicts of interest to declare.