The PRAMI trial, published in the New England Journal of Medicine, investigated in a multicentric randomised fashion whether “on the spot full revascularisation” provides outcome benefits in patients with multivessel disease presenting with a ST-elevation myocardial infarction (STEMI), as compared to a “culprit alone strategy”1. The study enrolled 465 patients with acute STEMI, who underwent primary PCI of the culprit lesion and were randomly assigned 1:1 either to “preventive PCI” of all non-culprit lesions with more than 50% diameter stenosis during the same procedure (234 patients) or to “no preventive PCI” (231 patients).
The study was terminated early on the advice of the data and safety monitoring committee. At mean follow-up of 23 months, a significant difference was observed in the primary composite endpoint of cardiac death, non-fatal myocardial infarction and refractory angina. A significant difference was observed separately in the occurrence of non-fatal myocardial infarction, as well as of refractory angina; however, the difference was not maintained in terms of cardiac death (Figure 1).
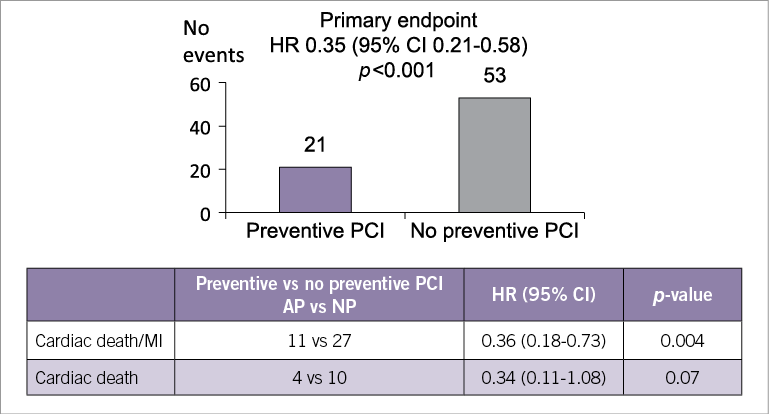
Figure 1. Summary slide taken from PCR trials book.
During the session, Keith G. Oldroyd, who represented the PRAMI investigators, identified three typical examples from the control group for the discussion. Interestingly, the vast majority of the audience agreed that, that in the pre-PRAMI era no “preventive PCI” during the same procedure would have been performed, the audience would now not have left these patients without further evaluation or staged revascularisation , as represented by the control arm.
As an expert trialist, Alexandra Lansky delivered a detailed insight of the published data contributing to better understanding of the results and and their scientific merit. Firstly, she emphasised that the results show a clear benefit in favour of preventive PCI, but this significant difference between the two groups in the composite primary endpoint was dominated by soft events. Specifically consistent trends were observed in all three components of the endpoint, but refractory angina represented more than half of the events, while hard events were under-represented. Lansky highlighted also that the definition of myocardial infarction was rather diverse: during the first 14 post-procedural days the criteria were strict, including either new ST-elevation or angiographic proof of coronary occlusion, after the 14th day the criteria became much more liberal, constituting purely symptoms and troponin rise. In addition, it was shown that the Kaplan-Meier curves started to deviate very early after the index procedure. Finally, Lansky underlined that, since the study was stopped prematurely by the data and safety monitoring committee, the low overall event rate and under-represented hard events resulted in a considerable overestimation of the difference between the two groups.
Despite the potential weaknesses described above, the faculty agreed, as Oldroyd concluded, that PRAMI is an important trial which not only generates discussions and debates but also sets the stage for a generation of future studies in the field.
Addressing the question as to whether PRAMI itself will change our practice, attendees would still elect to follow the current practice of staged evaluation and revascularisation in patients with STEMI and multivessel disease and avoid performing complete revascularisation on the spot. However, they all agreed that, since in PRAMI events occurred from very quickly after the index procedure, staging should not be scheduled unnecessarily late.
In conclusion, PRAMI is a landmark study, confirming that revascularisation is necessary not only for culprit lesions but also for non-culprit lesions in patients with STEMI and multivessel disease. However, the best timing and the best guidance of the revascularisation still remain the target of future studies.
Conflict of interest statement
A. Baumbach has received Speakers Fees from Astra Zeneca. The other authors have no conflicts of interest to declare.
Reference