Drug-eluting stents (DES) have substantially decreased in-stent restenosis (ISR) rates compared to bare metal stents (BMS); however, ISR has not been eradicated completely. The halt of neointimal tissue growth with delayed endothelialisation by antiproliferative drugs creates uncovered struts which become well established sites for thrombus formation and ISR1. As a “fear” for the interventional cardiologists, ISR has been a hurdle that had to be overcome. Using a metallic DES implanted in a segment with a previous metallic cage implies its own risk of restenosis2. Adding a metallic layer induces inflammation within the vessel wall which can trigger a new proliferative process in the previously stented vessel segments. Furthermore, arterial inflammation with giant cells shows an increase in neointimal tissue at follow-up. Additionally, the permanent coating of the metallic DES may trigger an eosinophilic reaction in the arterial wall, representing a hypersensitive response which has been observed mostly with sirolimus-eluting stents and their methacrylate coating3. Although new-generation DES have more compatible coatings and thinner struts, DES for the treatment of restenosis create a “double caged” vessel4. Instead of layering a second metallic structure in restenotic segments, alternative treatment options have now emerged.
In the search for a new treatment option for ISR, drug-eluting balloons (DEB) have been introduced into the armamentarium. Devoid of metal, DEB release an antiproliferative drug without implantation of a new permanent foreign body that triggers inflammation, thrombus formation and intimal hyperplasia. However, the main shortcomings of DEB are dissections, ultimately requiring a new stent during or after the balloon inflation, and limited transfer of the drug5,6. Using DEB in the treatment of ISR also provides less acute gain after the procedure compared to metallic stents7,8. Indeed, the residual percentage diameter stenosis is significantly higher in DEB compared to metallic EES7. Insufficient luminal gain can induce higher shear stress over the diseased segment that may engender platelet activation at these sites which may culminate in thrombus formation and acute/subacute stent thrombosis and neointimal hyperplasia resulting in recurrence of the ISR9. At follow-up after stent implantation, although not statistically significant, “in-segment” restenosis rates and late loss (mm) were fairly different between the DEB and EES groups (p=0.06 for restenosis and p=0.06 for late loss) in favour of EES in the RIBS IV Randomised Clinical Trial7. At follow-up, the “in-lesion” restenosis rate was significantly higher in patients treated with DEB in ISR lesions7. In summary, compared to metallic EES, DEB have resulted in lower minimal lumen diameter, lower net luminal gain, higher percent diameter stenosis and binary stenosis rates. At one-year follow-up, the main clinical outcome measure (composite of cardiac death, myocardial infarction, and target vessel revascularisation) was significantly lower in the metallic EES group compared to the DEB group7.
Bioresorbable scaffolds (BRS) are the most recent evolutionary step in “stent technology”. Studies are ongoing to evaluate the efficacy of these biodegradable devices not only in simple lesions but also in complex lesions10. Patients with ISR have become one of the target populations for BRS. From scant cases to multicentre registries, BRS have been under evaluation in patients with ISR11,12. Contrary to expectations, BRS have demonstrated good results: procedural success was satisfactory and there were no reported intra-procedural or acute in-stent thromboses in patients treated with BRS. At long-term follow-up, BRS have resulted in acceptable major adverse cardiovascular and cerebral events rates compared to metallic DES and DEB13. In a multicentre prospective registry, Moscarella and colleagues have demonstrated technical feasibility and safety in the treatment of ISR. The favourable clinical outcomes were independent of the type of ISR lesion (focal or diffuse, first or second recurrence, BMS or DES ISR)13. In the experience of Colombo et al, from 25 patients there was one periprocedural myocardial infarction (MI). At follow-up, only one MI and one target vessel revascularisation occurred12. Another recent prospective study by Rivero et al has confirmed the efficacy of BRS in the treatment of ISR: the results were in favour of BRS in this challenging patient population. It is noticeable that optical coherence tomography (OCT) was used for implantation guidance14.
In the treatment of ISR, directional atherectomy (DA), rotational atherectomy (RA) and cutting balloon (CB) have been studied in selected cases. DA is able to remove intra-stent neointimal tissue and provide higher luminal gain than balloon angioplasty15. However, an increased risk of stent strut deterioration has restrained its use in ISR. RA can eliminate neointimal tissue followed by expansion of the stent with a balloon that extrudes the residual neointimal tissue outside the stent. Despite encouraging initial results16,17, the angiographic ISR recurrence rate was higher with RA18. Another attractive and simple technique for the treatment of ISR is the CB. Besides protection against the “watermelon seeding” phenomenon (displacement of the balloon during inflation), the device incises the neointimal tissue and facilitates the extrusion of the obstructive tissue. Compared to balloon angioplasty, CB has demonstrated lower target lesion revascularisation at late follow-up19. After extrusion of the neointimal tissue (OCT can provide an unsurpassed assessment of the expansion of the device [Figure 1]), BRS may emerge as an attractive treatment choice, avoiding the need for an additional metal layer on the vessel wall while eluting the appropriate dose of cytostatic to the neointimal tissue and the vessel wall.
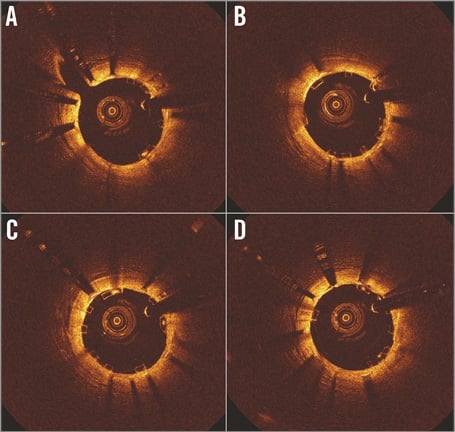
Figure 1. In-stent restenosis in the mid RCA was treated with Absorb BVS (Abbott Vascular, Santa Clara, CA, USA). OCT cross-sections of an ISR lesion post BVS implantation after non-compliant balloon post-dilatation. After extrusion of the residual neointimal tissue, the Absorb BVS was fully expanded and apposed (A,B,C,D).
Despite the observational character of their single-centre study and the small number of patients enrolled, Jamshidi et al20 attempted to demonstrate the potential of BRS utility in ISR lesions. In this trial, the majority of the ISR lesions occurred in the latest-generation DES group20. No scaffold thrombosis was reported. The results of this small exploratory study have demonstrated that BRS is an attractive alternative for treating ISR: they were comparable with the DEB arm from the RIBS IV trial.
In other words, BRS could become an alternative in the treatment of ISR lesions. With the adjunct of intracoronary imaging modalities, performing aggressive predilatation and post-dilatation during PCI and with optimal dual antiplatelet treatment, BRS seems to be a promising treatment option for ISR.
Conflict of interest statement
The authors have no conflicts of interest to declare.