Abstract
Aims: FFR measurements have been limited by the handling characteristics of pressure wire (PW) systems, and by signal drift. This first-in-human study evaluated the safety and efficacy of a new monorail catheter (Navvus) to assess coronary FFR, compared to a PW system.
Methods and results: Resting measurements were acquired with both systems. After initiating IV adenosine, FFR was measured with the PW alone, simultaneously using both systems, and again with PW alone. Any zero offset of PW or Navvus was then recorded. Navvus measured FFR in all patients in whom a PW recording was obtained (50 of 58 patients); there were no complications related to Navvus. Navvus FFR correlated well with PW FFR (r=0.87, slope 1.0, intercept -0.02). Within PW measurement accuracy, in no cases did Navvus FFR classify lesion significance differently from PW FFR. PW signal drift was significantly greater than Navvus (0.06±0.12 vs. 0.02±0.02, p=0.014).
Conclusions: Navvus and PW FFR correlated well. Navvus had less sensor drift. This new catheter-based system offers an alternative method for measuring FFR, with some potential advantages over PW.
Abbreviations
AV: atrioventricular
FFR: fractional flow reserve
NYHA: New York Heart Association
PCI: percutaneous coronary intervention
PW: pressure wire
TIMI: Thrombolysis In Myocardial Infarction
Introduction
The concept of fractional flow reserve (FFR), initially conceived by Pijls and colleagues1, was developed to assess the physiologic importance of a coronary stenosis by determining myocardial blood flow distal to the stenosis. Many stenotic lesions identified at angiography are of intermediate severity (defined as a percent diameter stenosis ≥40% and ≤70%), where the impact on myocardial perfusion cannot be determined accurately from angiography alone2,3. Despite the results in the FAME trials4,5, the National Cardiovascular Data Registry reported that only 6.1% of patients in the United States of America had a physiologic FFR assessment prior to percutaneous coronary intervention (PCI)6.
One reason for the underutilisation of FFR is that the measurement tools are difficult to use. Nearly all coronary FFR measurements have been performed with a 0.014” pressure wire (PW) incorporating a distal electrically based pressure sensor (e.g., Certus™; St. Jude Medical, St. Paul, MN, USA; Primewire Prestige®; Volcano Corp, San Diego, CA, USA). The need to provide electrical connections to the sensor near the distal end of the guidewire means that the “wire” is actually a thin-walled hollow tube. This PW may be difficult to deliver through tortuous vessels, and is prone to kinking. Moreover, assessment of diffuse disease or multiple lesions requires withdrawal of the PW and may lead to loss of wire position across the stenosis. These limitations of wire-based systems for measurement of intracoronary pressure may have impeded the adoption of FFR.
The RXi™ system (ACIST Medical Systems, Eden Prairie, MN, USA) is a new FFR technology utilising an ultrathin monorail microcatheter (Navvus®; ACIST Medical Systems) with an optical pressure sensor located close to the distal catheter tip (Figure 1). The potential advantages of the monorail system are the ability to use a coronary guidewire appropriate for the patient’s anatomy and with better torque and navigability than a PW, and the ability to move the sensor up and down the artery to determine the site of change in pressure gradient, without losing wire position7. In addition, the optically based pressure sensor may have less signal drift. On the other hand, the larger diameter of the catheter (0.022” mean diameter, compared with the 0.014” guidewire) could influence FFR measurement. The ACCESS-NZ first-in-human study (Australian New Zealand Clinical Trials Registry # ACTRN12612000789864) was designed to determine the safety and efficacy of the Navvus RXi system when FFR was measured with both systems.
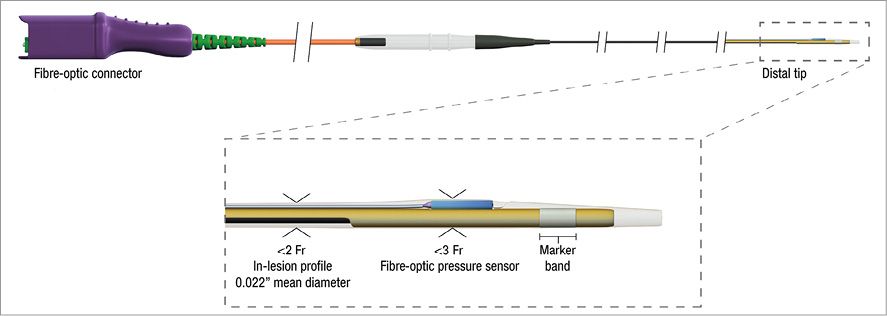
Figure 1. Navvus microcatheter. At the top, the entire device is shown. The distal tip construction is shown in detail.
Methods
PATIENT SELECTION
The study population comprised patients undergoing diagnostic coronary angiography at one of three New Zealand investigational centres. Patients were eligible for study if they were at least 18 years of age and undergoing coronary angiography for the diagnosis of coronary artery disease. Patients with a contraindication to anticoagulation, hypersensitivity to adenosine or contrast media, second or third degree atrioventricular (AV) block, and NYHA Class IV heart failure were excluded.
Diagnostic coronary angiography was performed by radial or femoral access. Patients with a stenosis of intermediate severity where measurement of FFR was thought to be clinically indicated were enrolled in the study, provided that the target stenosis was in a native coronary vessel, had a reference diameter ≥2.5 mm diameter by visual estimation, and had TIMI 3 blood flow. Patients with a stenosis in a bypass graft or intracoronary thrombus (angiographically identified or suspected) were excluded.
STUDY PROTOCOL
The study was approved by the New Zealand Northern Region Ethics Committee, and written, informed consent for the study was obtained from all patients.
Anticoagulation was administered at the investigator’s discretion. The coronary was engaged with a 5 Fr or larger guide catheter and all patients received intracoronary nitroglycerine. Before measuring the FFR, the investigator visually estimated the reference artery diameter and percent lesion stenosis. Blood pressure at the ostium of the coronary artery was measured through the coronary guide catheter using the standard haemodynamic monitoring system.
The study protocol is outlined in Figure 2. In brief, a low-profile monorail pressure catheter (Navvus; ACIST Medical Systems, Eden Prairie, MN, USA) and a PW (Certus™ versions 6, 7 or 8; St. Jude Medical, St. Paul, MN, USA) were prepared and “zeroed” outside the body. Next, the Navvus monorail catheter was mounted onto the PW and both were inserted into the guide catheter. The PW was advanced into the coronary artery such that the pressure sensor was just beyond the distal end of the guide catheter. The PW signal was “equalised” to the aortic pressure measured from the guiding catheter. The PW was then passed across the target stenosis and the pressure sensor positioned 2-4 cm beyond the lesion. Next, the Navvus catheter was advanced into the coronary and the optical pressure sensor positioned just beyond the guide tip. The Navvus catheter signal was then “equalised” to the haemodynamic pressure signal from the guide catheter. A resting transstenotic pressure ratio (Pd/Pa) was measured using the PW. The Navvus catheter was then advanced over the PW through the stenosis and Pd/Pa measured simultaneously using both the Navvus catheter and the PW. The Navvus catheter was then withdrawn into the guide catheter.
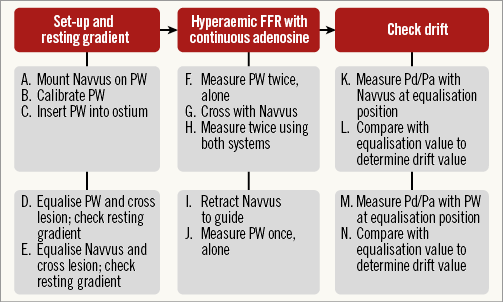
Figure 2. FFR measurement protocol. Resting measurements were acquired with both systems, followed by hyperaemic FFR. Drift in both systems was checked after completion of all measurements.
Following measurement of resting Pd/Pa using both pressure measurement systems, adenosine was administered intravenously at 140 µg/kg/min. After waiting approximately two minutes, FFR was determined twice, in rapid succession, using the PW alone. Next, the Navvus catheter was advanced across the stenosis and FFR determined twice with both the Navvus catheter and the PW across the lesion. The Navvus catheter was then withdrawn to the guide catheter and a final FFR measurement obtained using the PW alone. The PW was withdrawn to the proximal coronary and the baseline drift of both the Navvus and the PW systems recorded (with both sensors just beyond the guide tip). FFR measurements were repeated if Pd/Pa at the equalisation position was outside the 0.95 to 1.05 range.
Statistical methods
Unless otherwise noted, all summed values are presented as mean±one standard deviation (SD). Descriptive statistics were generated using Analyse-it (Analyse-it Software, Ltd., Leeds, United Kingdom).
COMPARISON OF FFR MEASUREMENTS
The paired FFR measurements by Navvus and PW were analysed with Passing-Bablok regression (Analyse-it). FFR repeatability was analysed using the first and second FFR measurements with each system using Bland-Altman analysis. Analysis of the relationship between the difference in FFR measurements and the FFR value was done using Bland-Altman analysis of the Navvus and PW difference, with the average of the two measures.
CLINICAL AGREEMENT BETWEEN PW AND NAVVUS
The clinical agreement between the PW- and Navvus-assessed FFR was determined as the concordance with PW-derived FFR values <0.80 and ≥0.80.
DRIFT MEASUREMENT
Drift was calculated as the difference between the initial equalisation and final check measurements. Values greater than 0.03 were considered clinically significant. Descriptive analyses and a t-test of means were conducted on the drift data.
Results
PATIENT AND PROCEDURE CHARACTERISTICS
Fifty-eight subjects met the enrolment criteria. Eight subjects were excluded from analysis (four for inability of the PW to cross the lesion, one for damage to the PW crossing a tortuous lesion, one with failure of both the PW and Navvus, one for Navvus RXi console use error, and one for patient intolerance of adenosine). FFR was measured in two arteries in two patients. In all patients in whom FFR could be determined by the PW, FFR was also determined using the Navvus catheter (52 lesions in 50 patients).
The 50 subjects ranged in age from 42 to 86 years (average 66±9 years), and 80% were male. Procedures were performed through the femoral or radial artery in 16 (32%) and 34 (68%) patients, respectively. By visual estimation, lesion severity was 40-49% in four (8%), 50-69% in 42 (81%), and 70-99% in six (11%) patients. The vessel reference diameter was 2.5-3.4 mm in 36 (69%), 3.5-3.9 mm in 10 (19%), and 4.0-5.5 mm in six (11%). The median diameter stenosis was 56% and median vessel diameter 3.0 mm. The lesions were in the left main coronary in three (6%), left anterior descending in 29 (56%), circumflex in seven (13%) and right coronary in 13 (25%). The distribution of FFR measurements (Figure 3) was unimodal, with a high percentage close to the 0.80 cut point.
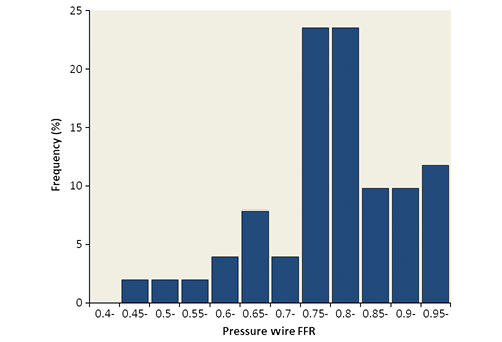
Figure 3. FFR frequency distribution. The frequency distribution of pressure wire FFR measurements is unimodal and shows the highest proportion close to the 0.80 cut-off.
There were no complications or adverse clinical sequelae from FFR assessment using the Navvus catheter. Following the FFR measurements, 17 patients underwent PCI, six had coronary bypass graft surgery, and 29 were treated medically.
COMPARISON OF FFR MEASUREMENTS
The mean FFR assessed using the PW alone and Navvus were 0.81±0.11 (range 0.47-0.99) and 0.79±0.12 (range 0.41-1.00), respectively. Repeatability of FFR measurement was similar between devices (Bland-Altman 95% limits of agreement: -0.04 to 0.04 for PW and -0.03 to 0.04 for Navvus). Figure 4A depicts FFR measured by PW, with and without Navvus in place; Figure 4B shows the correlation between Navvus and PW FFR assessment. No correlation between difference in FFR (PW minus Navvus) and the operator’s assessment of percent diameter stenosis was observed (Figure 5).
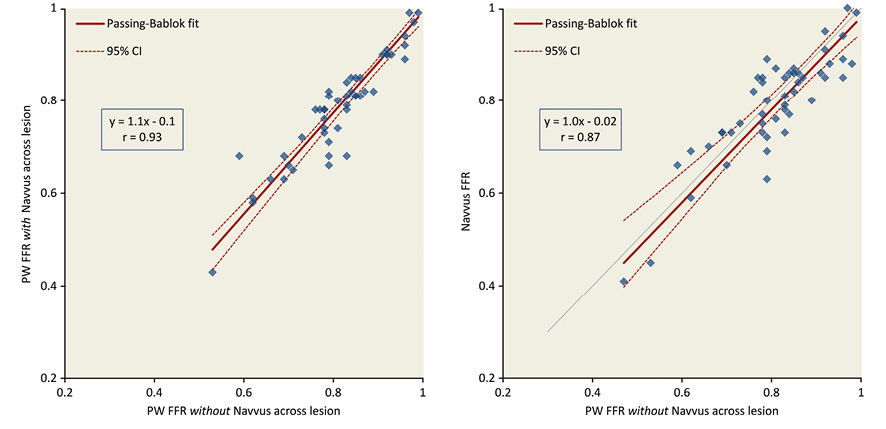
Figure 4. Relationship between measurements. A) Impact of Navvus on PW FFR. Scatter plots with Passing-Bablok fit of FFR values obtained from the PW with and without the Navvus catheter across the lesion. B) FFR comparison between systems. Scatter plots with Passing-Bablok fit of FFR values obtained from the PW and the Navvus catheter.
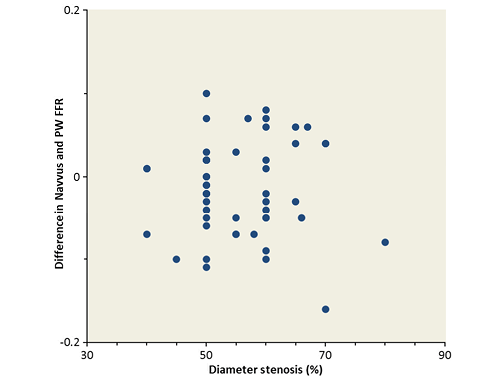
Figure 5. Correlation in FFR difference to operator-assessed %DS. No correlation between difference in FFR and the operator’s assessment of percent diameter stenosis was observed.
Figure 6 shows the concordance between PW and Navvus measurements of FFR in clinical decision making, where FFR <0.80 is used as a cut-off when deciding on revascularisation. The FFR measurement variability for the PW was ±0.045 (1 SD). Navvus assessment of FFR above and below the 0.80 cut-off was concordant with that of PW, within the measurement variability of PW.
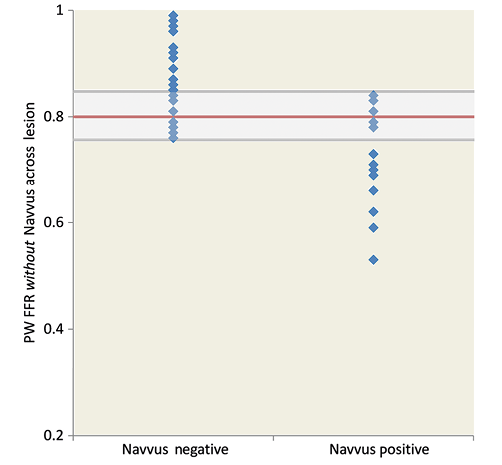
Figure 6. Diagnostic concordance between systems. PW FFR for lesions assessed negative and positive by Navvus, showing concordance within PW variability (indicated by grey band).
PREDICTION OF HYPERAEMIC FFR FROM BASELINE MEASUREMENTS
The Pd/Pa ratio obtained with Navvus at baseline was related to PW-derived FFR (Figure 7). In all 10 vessels with a Navvus Pd/Pa <0.90, the FFR was ≤0.80. Conversely, in all eight vessels with Navvus Pd/Pa >0.97, the FFR was >0.80.
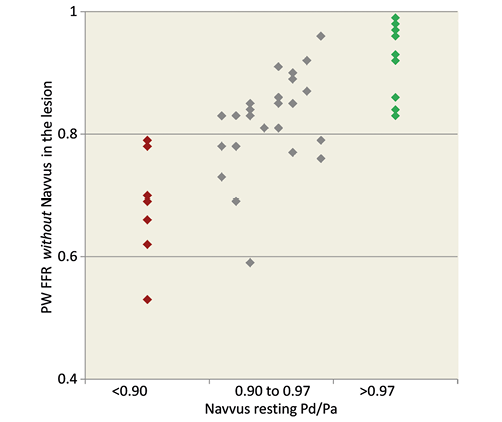
Figure 7. Correlation between Navvus resting Pd/Pa and PW FFR. All Navvus resting Pd/Pa <0.90 were assessed positive by PW, all Navvus resting Pd/Pa >0.97 were assessed negative by PW.
MEASUREMENT DRIFT
There was less sensor drift (Figure 8) with the optically based Navvus catheter than with the PW (0.02±0.02 Navvus vs. 0.06±0.12 PW, p=0.014). In addition, fewer patients had clinically significant (≥0.03) drift with the Navvus catheter (13%) than with the PW (33%).
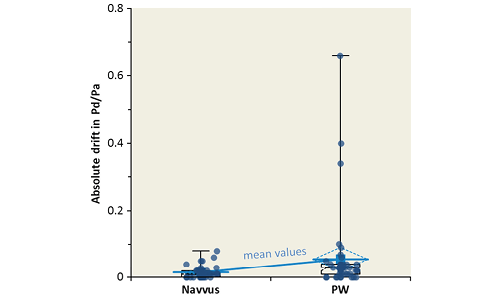
Figure 8. Drift observed in both systems. Drift in Navvus and PW as measured by the absolute change in Pd/Pa ratio with both sensors at the equalisation position. Mean=0.015±0.02 (Navvus), 0.056±0.12 (PW), median=0.01 (Navvus), 0.03 (PW). Data are inclusive of observations where FFR measurement was repeated.
Discussion
This study demonstrates that the low-profile, monorail Navvus catheter can be safely used to assess FFR in a typical patient population undergoing FFR measurement for clinical decision making. Although the study design did not allow determination of whether the Navvus catheter was easier to use than the Certus PW, there were no patients in whom the Certus wire succeeded and the Navvus catheter failed. The Navvus catheter assessment of FFR correlated well with measurements obtained by PW over a wide range of FFR values and arterial diameters (2.5-5.5 mm). The distribution of FFR measurements was appropriate for the study purpose, with a high proportion near the 0.80 cut-off. The measurement repeatability of the Navvus was high and signal drift of the optical sensor low.
Fractional flow reserve has become an important tool in determining the need for revascularisation in patients with stable coronary artery disease. Intervention based on FFR improves PCI outcomes8-11, is equally effective in males and females12, and reduces the costs associated with PCI13. Despite the demonstrated value of FFR measurements in determining therapy, most patients do not undergo FFR measurement prior to percutaneous revascularisation. This may, in part, be due to the perception that pressure measurement coronary wires are less easy to manipulate and position than regular coronary guidewires. This perception is supported by the inability of experienced operators to position the PW in four of 58 patients in this study. While the protocol did not allow crossover to a conventional wire and Navvus in these cases, it is likely that this approach would have facilitated the operator’s ability to obtain an FFR.
The Navvus monorail catheter allows the use of a coronary guidewire best suited to negotiating the patient’s anatomy and providing support for subsequent intervention, if required. The ability to move the pressure sensor within the artery to locate the site of change in pressure gradient, without moving the tip of the wire, is another advantage, particularly in patients with multiple lesions or diffuse disease. Signal drift over time of the PW may reduce the accuracy of measurements. A potential advantage of the Navvus catheter is that it uses an optical pressure sensor and a single optical fibre to transmit the signal. This low-profile construction reduces signal drift and allows the user to make repeated measurements of FFR, without loss of signal accuracy.
The Navvus monorail catheter is larger in cross-section than a PW; it has an oval shape roughly twice the area of a 0.014” wire. A secondary aim of this study was to determine whether that increased profile had a clinically relevant impact on FFR assessment in vessels of at least 2.5 mm diameter, which represent the vast majority of vessels undergoing FFR measurement. There was a good correlation between FFR assessed by PW, with and without the Navvus catheter in place (Figure 4A), and also between FFR assessed by PW and by the Navvus catheter (Figure 4B). While this needs further assessment in a larger patient cohort (only 11 patients in this series had a PW FFR <0.75), an obstructive effect in more severe lesions appears unlikely to affect clinical decision making. The lack of obstructive effect in vessels relevant to FFR is also suggested by the lack of correlation to operator-assessed diameter stenosis. Finally, the effect of the catheter on vessel tortuosity, including creation of pseudo-stenosis, was not specifically assessed in this study, but was not observed. Patients were not excluded based on tortuosity.
An interesting observation was that, if the baseline Navvus Pd/Pa was >0.97, the PW FFR was always normal, and, if the Navvus resting Pd/Pa was <0.90, the PW FFR was always abnormal (Figure 7). Studied previously14,15, this needs further evaluation in a larger patient cohort, but confirms the possibility that adenosine-induced vasodilation might not be needed in all patients.
Study limitations
This study has some limitations. Quantitative coronary angiography was not performed; vessel diameter and lesion severity were visually assessed by the operator.
Different versions of the Certus PW became available and were used over the course of the study, so the comparison was not with a single version. In particular, signal drift might have reduced with later versions of the PW.
The magnitude of PW drift may have been greater during this study than in general clinical use because the study protocol required repeated measurements over time, with and without the Navvus catheter in place. The study design may also have disadvantaged PW compared to Navvus because the PW was introduced and equalised first, and checked for drift last, resulting in an estimated one to two minutes longer time between equalisation and drift check. Nonetheless, less drift was observed with the fibre optic-based system.
Finally, the study population was relatively small, largely had stable coronary disease, and included few lesions with an FFR below the 0.80 cut-off. Additional data points are necessary to determine fully the effect of the Navvus catheter on FFR assessment. The findings cannot be extrapolated to other patient cohorts, such as those with significant left ventricular dysfunction.
Conclusion
Navvus assessments of lesions in vessels of at least 2.5 mm diameter were comparable to those obtained using a PW, but with less signal drift over time.
| Impact on daily practice This study demonstrates that a new, low-profile, optically based monorail catheter can be safely used to measure FFR in a typical patient population requiring functional lesion assessment. The physician now has a device able to measure FFR using standard coronary guidewires. |
Funding
This study was supported by ACIST Medical Systems.
Conflict of interest statement
The authors have no conflicts of interest to declare.

