Abstract
Aims: To evaluate the feasibility and safety of an anticoagulation adapted regimen for transradial coronary angiography.
Methods and results: We randomly assigned 162 consecutive patients who benefited from an elective transradial approach for coronarography to receive either a standard dose of 5,000 IU heparin or 50 IU/kg with an upper limit of 5,000 IU. Patients under anti-vitamin K therapy were excluded. The TRband® compression system was employed for the entire population after the procedure. Radial artery patency, the primary endpoint, was evaluated with Doppler before discharge from the hospital. Secondary endpoints were: ACT level immediately before sheath removal, compression length and bleeding complications. Both groups were well matched. ACT level is significantly lower in the adjusted anticoagulation group (231.4 min, vs. 265.6 min, p<10-4). Radial compression time was higher in the standard protocol group (235.5 min, vs. 204.5 min, p<10-5). No radial occlusion was noted, whatever the group considered. Local haematoma is less frequent in the 50 IU/kg group, with no statistical difference.
Conclusions: A weight-adjusted heparin dose allows for lower ACT levels and decreases in radial compression time without increase in radial artery occlusion. The impact on bleeding complication needs further evaluation in larger series.
Introduction
First described nearly 20 years ago, the radial approach is now used routinely both for coronarography and coronary angioplasty procedures1,2. The main advantage of the radial approach lies in the reduction of haemorrhagic and vascular complications at the puncture point when compared to the femoral and humeral approaches3. It furthermore enables patients to resume walking sooner, thus improving their comfort. Its main drawbacks, periprocedural radial artery spasm and postprocedural radial artery occlusion, are significantly reduced by the use of a pharmacological cocktail combining an antispasticity agent, nitro compound or calcium inhibitor and an anticoagulant. Though in coronary angioplasty, 70 UI/kg heparin is the commonly accepted dose, in the context of diagnostic procedures, most interventional cardiology teams use a standard, non-adapted dose of 5,000 UI unfractionated heparin, in accordance with published data4. No studies have attempted to optimise this dose of anticoagulant, even though haemorrhagic complications are closely correlated with the activated clotting time (ACT) level reached5. The purpose of our study was to determine whether the use of a weight-adjusted dose of heparin, designed to achieve a lower ACT level, would limit the haemorrhagic risk without compromising radial artery permeability after the procedure.
Population and method
Patients
Between September 2007 and March 2008, all patients hospitalised for elective coronarography, by either the left or right radial artery approach with a 5 Fr catheter, were prospectively and consecutively included. Patients were randomised to two groups according to their year of birth: patients born during an even year were administered a standard 5,000 UI dose of unfractionated heparin (group A), patients in the second group (group B) benefited from a weight-adjusted posology of 50 UI/kg, without however exceeding the maximum dose of 5,000 UI.
Approval was obtained from the establishment’s ethics review board and the patients gave their consent.
Excluded from the study were all patients receiving long-term anti-vitamin K, those having received an injection of low molecular weight heparin during the 12 hours preceding the examination and those for whom an ad hoc angioplasty was performed. Emergency cases were also excluded.
Procedure schedule
All the cardiac catheterisations were performed by an experienced radialist operators (more than one thousands radial coronarography for each interventional cardiologist).
The transfixing radial puncture was performed according to the Seldinger method, using a 20G cathlon® (Smiths Medical International, London, United Kingdom), insertion of a 0.025 inch hydrophilic guide, followed by insertion of a 7 cm long radial sheath (Terumo Corporation, Tokyo, Japan).
All patients were given a combination of verapamil 2.5 mg and unfractionated heparin as per the randomisation protocol. The mixture was directly injected into the sheath upon insertion.
The ACT level was measured at the end of the procedure when the sheath was being removed using a Hemochron signature + instrument (Gamida, Eaubonne, France).
Haemostasis was ensured by means of a TR Band® radial artery compression system, avoiding excessive compression (Terumo Corporation, Tokyo, Japan). The system was precisely positioned using a marker pen; compression was generated by inflation of the balloon with 15 ml air prior to removing the sheath; after removal of the sheath, the balloon was then deflated ml per ml until bleeding occurred; this bleeding was then stopped by inflating with one additional ml; the volume of air injected could not be less than 10 ml.
After three hours, the TR Band® was removed. In the event of persistent bleeding, 30 minutes of additional compression were applied, and repeated until haemostasis was achieved.
All patients underwent Doppler exploration of the radial artery within 24 hours after the procedure, performed by a suitably trained nurse using a Vascutrack 120 instrument fitted with a 5 MHz probe. (Ultrasound Technologies Ltd., Caldicot, South Wales, United Kingdom). The presence of a signal indicative of arterial permeability was sought, both with and without compression of the cubital artery to eliminate any signals from retrograde circulation.
Assessment criteria
Primary criteria
The main study criteria was radial artery permeability during the Doppler examination,
Secondary criteria
The ACT level achieved radial artery compression time and the presence, or absence, of haemorrhagic complications was compared for each of the two groups. Bleeding was considered to be major in the event of loss of at least four haemoglobin points, brain haemorrhage, need for transfusion and/or surgical haemostasis. In all other cases, bleeding was considered to be minor.
Statistical analyses
Categorical variables are presented as both frequency values and number of patients, and were compared with the χ2-test. Continuous values are expressed as mean ±standard deviation and statistical comparisons were performed using Student’s T-test. A p-value ≤0.05 was interpreted as statistically significant.
Results
During the study period, 436 coronarographies were performed. Amongst these coronarographies, 35 were performed by the femoral approach, 180 by ad hoc angioplasty and 59 examinations were conducted with a 6 Fr sheath. Our prospective study concerned the remaining 162 patients, 79 randomised to group A and 83 to group B. The proportion of women, along with biometric data, was identical. Cardiovascular risk factors and previous coronary history were similar for all patients. Nearly one quarter of the patients in both groups had already undergone at least one coronarography via the same radial approach (Table 1).
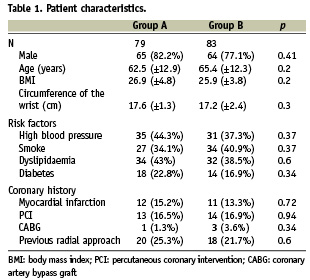
The left radial approach was preferred, though a greater proportion of right radial approaches was observed in the 50 UI/kg group (20.4% vs. 8.8%, p<10–3). The duration of the procedure, along with the volume of air in the TR Band® required for efficient compression, did not differ, whatsoever the group being considered. The radial artery compression time, however, was significantly longer when a non-weight-adjusted dose of heparin was used, p<10–5 (Table 2).
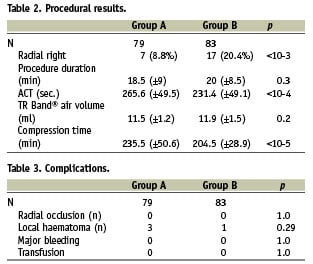
The ACT level was significantly higher in group A (265.6 min vs. 231.4 min, p<10–4). No radial occlusions, however, were observed in either group. Furthermore, no significant haemorrhagic complications affected patient outcome, regardless of the heparin dose used. An increase in local haematomas was observed in the 5,000 UI group, but this difference was not significant (Table 3).
Discussion
Since the first series of patients described by Campeau for diagnostic coronarography procedures1, the use of the radial approach has extended to all clinical situations encountered in interventional cardiology. Thus, many teams have reported their personal experiences, both in the context of elective angioplasty and of primary angioplasty2,6. This approach, more comfortable for patients as well as enabling them to resume walking sooner, is first and foremost the cause of significantly fewer haemorrhagic and vascular complications at the puncture point than the femoral approach, with a reduction in the risk of major bleeding of more than 70% in the meta-analysis of Rao et al7. This is particularly true in situations presenting a high risk of bleeding, especially when glycoprotein IIb/IIIa inhibitors are used, after emergency angioplasty following failed thrombolysis and in patients receiving long-term anti-vitamin K8-11.
The main complication associated with the initial use of this approach is occlusion of the radial artery. Its incidence is significantly reduced by injection of anticoagulant at the start of the procedure. This was seen in the series of Spaulding et al where the occlusion rate in patients not receiving heparin was 71%, dropping to 24% under 2,000 to 3,000 UI heparin, then to 4.3% under 5,000 UI4. Thus, this standard dose has been applied to the majority of work published, frequently reporting occlusion rates below 5%, even in the case of repeat punctures12-15.
Bleeding, whether from the puncture point or elsewhere, significantly alters the prognosis, with aggravation of morbidity and mortality in patients undergoing an interventional cardiology procedure. It therefore appeared important to us to consider the adjustment of the dose of heparin to the patient’s weight in order to limit the post-coronarography haemorrhagic risk.
In our work, the application of a lower dose of heparin adjusted to the patient’s weight did not alter the incidence of radial occlusion. Indeed, no occlusions were reported in either group, significantly lower than the previously reported rate of 3-5% which probably reflects the small number of patients included in the study. However, this result, with anticoagulation remaining effective at the end of the procedure, as shown by the residual ACT level, may be explained by several factors: the great experience of the operators and the use of high-performance equipment such a dedicated sheath for the radial approach, whose profile limits arterial aggression and whose dimensions serve to optimise the ratio between its outer diameter and the inner diameter of the arterial, a measurement that directly influences the risk of post-procedure occlusion16; as well as a limited and compliant compression time, using a radial artery compression system one of whose properties is to allow modulation of the minimum pressure applied to achieve haemostasis, thus allowing the persistence of anterograde arterial blood flow. Sanmartin, however, showed that modulating the force applied to radial compression significantly reduced the risk of radial occlusion17. Similarly, in the RACOMAP study, using the TR Band®, a significant drop in the rate of radial occlusion was observed, dropping from 12 to 1.1% when air volume-mediated pneumatic compression was adjusted to mean arterial blood pressure, compared to standard compression using 15 ml of air, p<0.000118. Furthermore, in the PROPHET study, the short-term risk of radial occlusion was reduced by 59% when a compression system allowing persistent blood flow through the radial artery was used, compared to conventional compression19. Finally, one of the most important predictors of radial artery patency following radial catheterisation is the possibility of not interrupting radial flow during compression.
The advantage of using a weight-adjusted dose of heparin is two fold. First, the results of our study show that the ACT level achieved was significantly lower (265.6 min vs. 231.4 min, p <10–4). There is, however a curvilinear relationship between ACT level and haemorrhagic risk5. There was no increased haemorrhagic risk in group A and there are several explanations: first, major bleeding is rarely expected to occur during 5 Fr radial and scheduled diagnostic catheterisation, second, in trained hands along with proper sheath selection and technique, minor bleeding and haematoma are infrequent and any difference accorded to anticoagulation regimens can be demonstrated only in a powerful trial with many more patients. Nevertheless, there was a tendency towards reducing the number of haematomas in group B. Secondly, the compression time was significantly reduced (204.5 min vs. 235.5 min, p <10–5). Thus, considering that radial artery cannulation time is an occlusion predictive factor20, reducing the dose of heparin should limit the risk of occlusion.
Study limitations
First, the decision to randomise according to age of birth allows some bias because the group is known before the decision to include the patient. However, we randomised all consecutive eligible patients to limit this. Another possibility would be to use other ways of randomisation, by drawing lots, for example. Second, the lack of a formal power calculation to estimate the number of patients needed to be included is a statistical limitation. The major limitation of our study pertained to the small population size preventing us from demonstrating any significant difference in terms of haemorrhagic complications. Furthermore, no late control of permeability was performed, thus ignoring possible delayed occlusions. The different studies that contained early and late radial permeability tests in their protocol, however, have shown that occlusion rates are always lower in the long-term.
Conclusion
The injection of a weight-adjusted dose of unfractionated heparin is safe and efficient, without any increased risk of radial occlusion in elective 5 Fr radial diagnostic coronary angiography. Compared to a single dose of 5,000 UI, it limits the ACT level achieved and significantly reduces the compression time required to achieve haemostasis at the puncture point. The assessment of its actual impact in terms of haemorrhagic events, however, will require a study including a larger number of patients.

