Abstract
Aims: Our aim was to evaluate stent expansion and acute recoil at deployment and post-dilatation, and the impact of post-dilatation strategies on final stent dimensions.
Methods and results: Optical coherence tomography (OCT) was performed on eight bare metal platforms of drug-eluting stents (3.0 mm diameter, n=6 for each) during and after balloon inflation in a silicone mock vessel. After nominal-pressure deployment, a single long (30 sec) vs. multiple short (10 sec x3) post-dilatations were performed using a non-compliant balloon (3.25 mm, 20 atm). Stent areas during deployment with original delivery systems were smaller in stainless steel stents than in cobalt-chromium and platinum-chromium stents (p<0.001), whereas subsequent acute recoil was comparable among the three materials. At post-dilatation, acute recoil was greater in cobalt-chromium and platinum-chromium stents than in stainless steel stents (p<0.001), resulting in smaller final stent areas in cobalt-chromium and platinum-chromium stents than in stainless steel stents (p<0.001). In comparison between conventional and latest-generation cobalt-chromium stents, stent areas were not significantly different after both deployment and post-dilatation. With multiple short post-dilatations, acute recoil was significantly improved from first to third short inflation (p<0.001), achieving larger final area than a single long inflation, despite stent materials/designs (p<0.001).
Conclusions: Real-time OCT revealed significant acute recoil in all stent types. Both stent materials/designs and post-dilatation strategies showed a significant impact on final stent expansion.
Introduction
While drug-eluting stents (DES) have substantially reduced in-stent neointimal hyperplasia, there is compelling clinical evidence that mechanical or procedure-related factors remain important contributors to the development of both restenosis and thrombosis after DES implantation. In particular, the most consistent risk factor reported in clinical DES studies has been suboptimal stent expansion1, potential causes of which include underexpansion during balloon inflation, acute stent recoil, or a combination thereof. In a given target lesion, these mechanisms are contingent on stent designs and materials as well as the performance of the stent delivery balloons. The strategy for post-deployment high-pressure balloon dilatation can also determine final stent dimensions.
To date, various stent designs and materials have been employed for DES platforms to improve acute stent performance (e.g., flexibility, conformability, and deliverability) as well as long-term outcomes (e.g., strut fracture and restenosis)2. Although several in vivo studies have attempted to evaluate the effect of prolonged delivery inflation time in certain types of DES3-7, detailed mechanical responses of contemporary stent platforms to balloon inflations have not been systematically investigated. Furthermore, the optimal post-dilatation strategy specific to stent designs/materials remains unknown.
The aim of this study was to evaluate: 1) stent expansion and acute recoil, at both deployment and post-dilatation; and 2) the impact of post-deployment balloon dilatation strategies on final stent dimensions in different stent designs/materials. To overcome the limitations of angiography and intravascular ultrasound (IVUS) in the precise evaluation of acute stent recoil, this study utilised real-time optical coherence tomography (OCT) with a dedicated imaging wire inserted into the guidewire lumen of the balloon catheters, allowing continuous monitoring of stent expansion through balloon inflation and deflation.
Methods
STENT PLATFORMS
Stents examined in this study included Driver™ (Medtronic Vascular, Santa Rosa, CA, USA), MULTI-LINK (ML) VISION (Abbott Vascular, Santa Clara, CA, USA), Select (Cordis Corporation, Miami, FL, USA), Liberté™ (Boston Scientific, Marlborough, MA, USA), S-Stent™ (Biosensors International, Newport Beach, CA, USA), Integrity® (Medtronic Vascular), MULTI-LINK 8 (ML-8; Abbott Vascular), and OMEGA™ (Boston Scientific). The corresponding DES are Endeavor® (Medtronic Vascular), XIENCE V® (Abbott Vascular) or PROMUS™ (Boston Scientific), CYPHER SELECT® (Cordis), TAXUS™ Liberté (Boston Scientific), Nobori® (Terumo Corporation, Tokyo, Japan), Resolute Integrity® (Medtronic Vascular), XIENCE Prime (Abbott Vascular), and TAXUS Element or PROMUS Element™ (Boston Scientific), respectively. Table 1 summarises the key characteristics of each stent design. The stents were divided into three groups according to their material: stainless steel, cobalt-chromium, and platinum-chromium stents. Although the Driver stent technically consists of cobalt (35%), nickel (35%) and chromium (20%), it was treated as a cobalt-chromium stent as widely recognised. In addition, we defined the Integrity and ML-8 stents as the latest-generation cobalt-chromium stents, in comparison with the Driver and ML VISION stents, defined as conventional cobalt-chromium stents.
EXPERIMENTAL STRATEGIES
Experimental strategies are described in Figure 1. Six samples of each stent design with a diameter of 3 mm were investigated. All stents were deployed with their original delivery balloon (3.0 mm) at nominal pressure (Table 1) for 15 seconds in silicone-tube mock vessels (3.0 mm ID±0.2 mm, 30 mm length, 5-7% radial compliance per 100 mmHg; Dynatek Dalta, Galena, MO, USA) (Figure 2) immersed in 37°C saline, in order first to focus on intrinsic elastic recoil of the stent. After stent deployment, post-dilatation was performed using a non-compliant balloon larger than the internal diameter of the silicone tube (3.25×18 mm, Powered Lacrosse®; Goodman, Nagoya, Japan), mainly to compare radial strength of the stent against compressive external force from the tube. The length of the non-compliant balloon was longer than all types of stent to cover the entire stent at inflation, and a brand-new balloon was used for each post-dilatation procedure. The balloon was inflated to 20 atmospheres per inflation. Each stent group was divided into two subgroups by post-dilatation strategy: single long inflation (30 seconds) vs. multiple short inflations (10 seconds × 3 times). Measurement of each balloon inflation time was started when the objective pressure was achieved. Then, the inflation pressure was kept stable at the objective pressure as much as possible by manually adjusting the balloon inflation device to compensate for a declined pressure during each assigned time period.
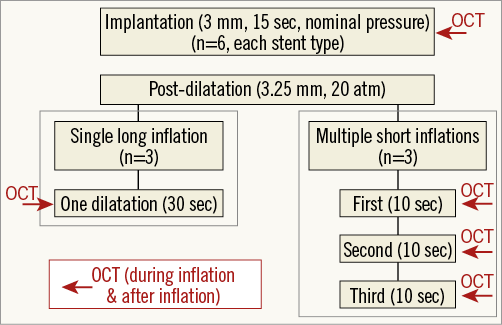
Figure 1. Experimental strategies. Each stent group was divided into two subgroups by post-dilatation strategy: single long inflation (30 seconds) vs. multiple short inflations (10 seconds×3).
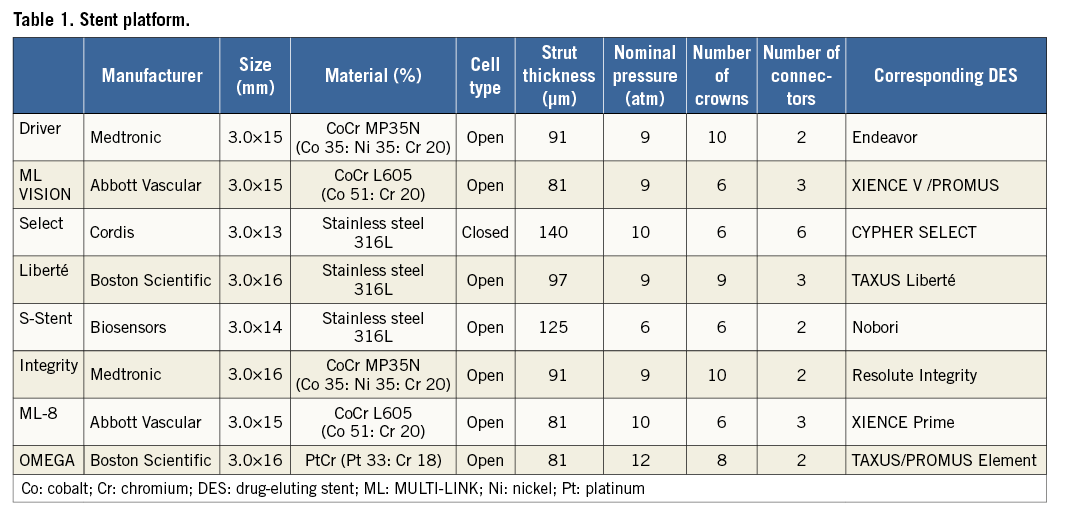
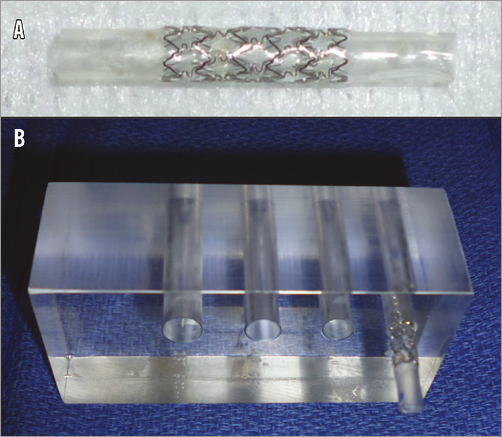
Figure 2. Bench test model. A) All stents were deployed in silicone mock vessels (3.0 mm ID±0.2 mm, 30 mm length, 5-7% radial compliance per 100 mmHg). B) All procedures were performed on the inside of the phantom model with a diameter of 4.57 mm as a calibration.
OCT IMAGE ACQUISITION AND QUANTITATIVE ANALYSIS
OCT imaging was performed using a dedicated OCT wire (0.014 inches in diameter; LightLab Imaging LLC, Westford, MA, USA) inserted into the guidewire lumen of the balloon catheter. Real-time imaging was continuously recorded during balloon inflation and after deflation at both deployment and post-dilatation. The OCT wire was pulled back manually during recording. In order to achieve accurate measurements, all procedures were performed on the inside of the phantom model with a diameter of 4.57 mm as a calibration. OCT images were analysed using commercially available software (echoPlaque™; Indec Systems, Inc., Santa Clara, CA, USA). Stent area was computed by planimetry at three cross-sections (proximal, mid and distal) within each stent (Figure 3), and the averaged stent area was used for subsequent analyses.
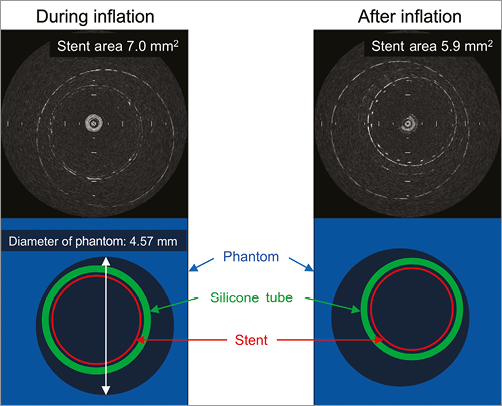
Figure 3. Example of an OCT image. Stent areas during inflation and after deflation at deployment were analysed. In this particular case, stent areas were 7.0 mm2 during inflation and 5.9 mm2 after deflation. Percent acute recoil was 15.7%.
Statistical analysis
Statistical analysis was performed using StatView 5.0 (SAS Institute, Cary, NC, USA). Continuous variables were presented as mean±SD. Comparisons among the individual stents or among the three design/material groups were performed using analysis of variance (ANOVA) with post hoc comparison using the Bonferroni correction, and comparisons between two continuous variables were carried out with a two-tailed, unpaired t-test. Serial changes in stent area (during balloon inflation to post deflation) were evaluated with a paired t-test. Differences in the degree of stent recoil from the first to the third inflation during multiple short inflations were analysed with two-factor ANOVA. A value of p<0.05 was considered statistically significant.
Results
STENT DEPLOYMENT
Using their original delivery system at nominal pressure, stent areas during inflation were considerably different among all stent types (p<0.001) (Table 2). Significant acute recoil was subsequently observed in all stent types but in varying degrees (p<0.001). As a result, stent areas after deflation were also considerably different among all stent types (p<0.001).
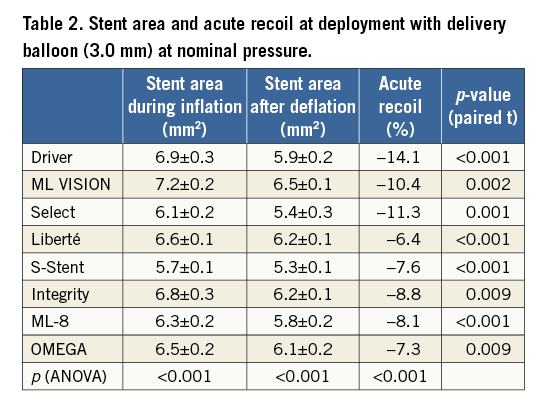
In comparing stent materials (Figure 4), the stent area in stainless steel stents (6.1±0.4 mm2) was smaller than in cobalt-chromium stents (6.8±0.4 mm2, p<0.001) and platinum-chromium stents (6.5±0.2 mm2, p=0.038) during inflation. The degrees of recoil were not significantly different among the three stent materials. Consequently, the post-deployment stent area in stainless steel stents (5.6±0.5 mm2) was smaller than in cobalt-chromium stents (6.1±0.3 mm2, p<0.001) and platinum-chromium stents (6.1±0.2 mm2, p=0.020) after deflation (in mean diameter, 2.68±0.11 mm, 2.79±0.07 mm and 2.78±0.05 mm, respectively). Of note, these results indicate that post-deployment stent dimensions were only 79-86% of cross-sectional areas and 89-93% of diameters expected by the manufacturers’ compliance charts, despite this non-diseased coronary model (3.0 mm stents deployed in a 3.0 mm tube).
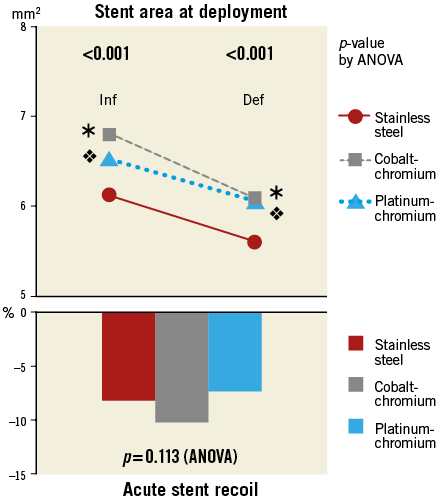
Figure 4. Stent area and acute stent recoil at deployment with delivery balloon (3.0 mm): stainless steel vs. cobalt-chromium vs. platinum-chromium stents. ![]() p<0.001.
p<0.001. ![]() p<0.05 in post hoc comparisons vs. stainless steel. Def: after deflation; Inf: during inflation
p<0.05 in post hoc comparisons vs. stainless steel. Def: after deflation; Inf: during inflation
In comparing conventional and latest-generation cobalt-chromium stents (Figure 5), the stent area in latest-generation stents was smaller than in conventional cobalt-chromium stents during inflation. The degree of recoil was less in latest-generation stents than in conventional cobalt-chromium stents. As a result, stent areas after deflation were not significantly different between the two groups.
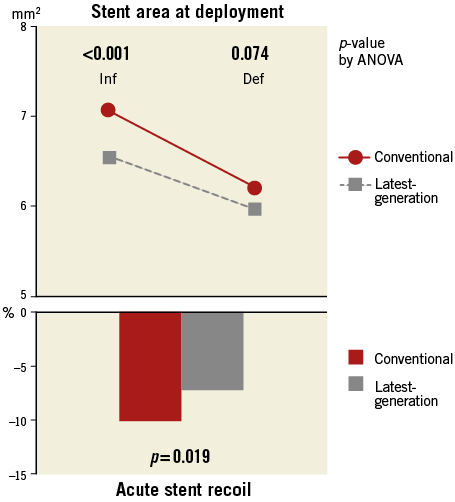
Figure 5. Stent area and acute stent recoil at deployment with delivery balloon (3.0 mm): conventional vs. latest-generation cobalt-chromium stents. Def: after deflation; Inf: during inflation
POST-DILATATION
Overall, the average stent areas during post-dilatation inflation using a non-compliant balloon at 20 atmospheres were similar between the single long inflation and the first short inflation (8.2±0.2 vs. 8.2±0.1 mm2, p=0.322). During multiple short inflations, a numerically slight but statistically significant increase of the stent areas during inflation was observed from the first to the third short inflation (8.2±0.1 to 8.3±0.1 mm2, p<0.001). Among all stent types, stent areas were comparable during single long inflation, but not during multiple short inflations (Table 3). Regardless of inflation strategies, significant acute recoil was observed after post-dilatation in all stent types. Final stent areas after deflation were considerably different among all stent types, after both single long inflation and multiple short inflations.
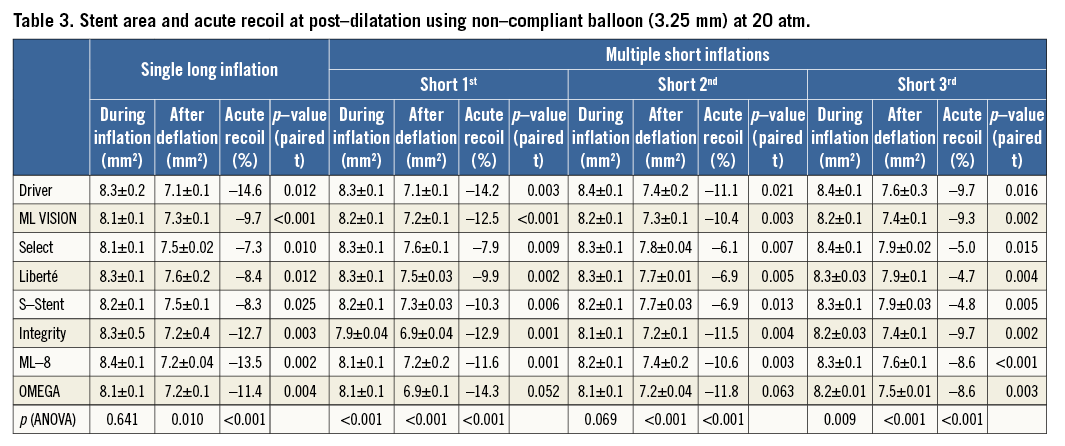
In comparing stent materials (Figure 6), stent areas during post-dilatation inflation were comparable among stainless steel, cobalt-chromium and platinum-chromium stents. However, cobalt-chromium and platinum-chromium stents showed significantly greater recoil than stainless steel stents both after single long inflation and at each point after multiple short inflations. As a result, final stent areas were smaller in cobalt-chromium and platinum-chromium stents than in stainless steel stents, after both single long inflation (7.2±0.2 and 7.2±0.1 vs. 7.6±0.1 mm2, p<0.001) and multiple short inflations (7.5±0.1 and 7.5±0.01 vs. 7.9±0.04 mm2, p<0.001). Among all three stent materials, the degrees of recoil (% recoil) were not significantly different between single long inflation and first short inflation (–8.0% vs. –9.4%, p=0.085, in stainless steel stents; –12.6% vs. –12.8%, p=0.808, in cobalt-chromium stents; –11.4% vs. –14.3%, p=0.099, in platinum-chromium stents). On the other hand, the degrees of recoil were significantly improved from first to third short inflation (from –9.4% to –4.8%, p<0.001, in stainless steel stents; from –12.8% to –9.3%, p<0.001, in cobalt–chromium stents; from –14.3% to –8.6%, p<0.001, in platinum–chromium stents). Consequently, multiple short inflations achieved greater final stent areas than a single long inflation in all three stent materials (Table 4).
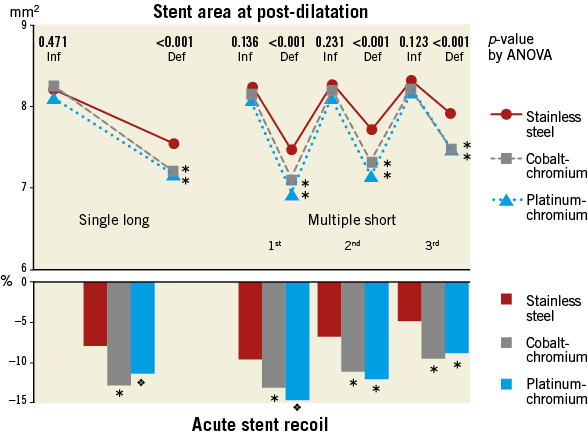
Figure 6. Stent area and acute stent recoil at post-dilatation with non-compliant balloon (3.25 mm): stainless steel vs. cobalt-chromium vs. platinum-chromium stents. ![]() p<0.001.
p<0.001. ![]() p<0.01. In post hoc comparisons vs. stainless steel. Def: after deflation; Inf: during inflation
p<0.01. In post hoc comparisons vs. stainless steel. Def: after deflation; Inf: during inflation
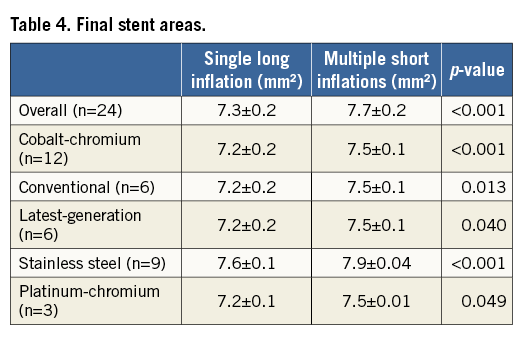
In comparing conventional and latest-generation cobalt-chromium stents (Figure 7), stent areas during inflation and after deflation, and the degrees of recoil were comparable between the two groups, except for the stent area during the first short inflation. Similar to the comparison of stent materials, the degrees of recoil were not significantly different between single long inflation and first short inflation. On the other hand, the degrees of recoil were significantly improved from first to third short inflation in both groups. Consequently, multiple short inflations achieved greater final stent areas than a single long inflation in both groups (Table 4).
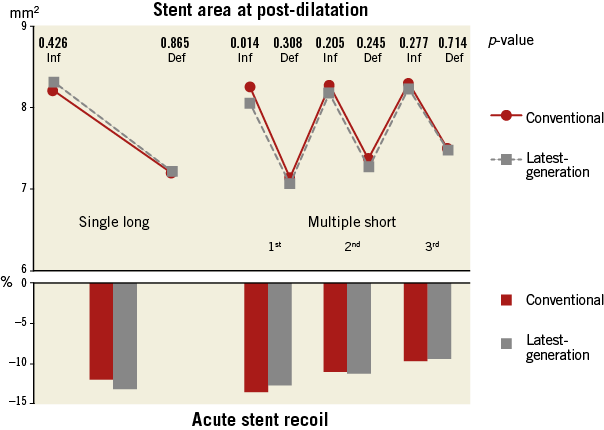
Figure 7. Stent area and acute stent recoil at post-dilatation with non-compliant balloon (3.25 mm): conventional vs. latest-generation cobalt-chromium stents. Def: after deflation; Inf: during inflation
Discussion
The present study highlights the impact of stent materials/designs and post-dilatation strategies on stent expansion in response to balloon inflations. The main findings of this study are as follows: 1) cobalt-chromium and platinum-chromium stents achieved larger stent area than stainless steel stents at deployment with their original delivery systems; 2) the degrees of recoil were greater in cobalt-chromium and platinum-chromium stents than in stainless steel stents when they were dilated equally by the same non-compliant balloon system at post-dilatation; 3) the performance was largely similar between conventional and latest-generation cobalt-chromium stents; and 4) multiple short inflations achieved larger final stent area than a single long inflation at post-dilatation, regardless of stent materials and designs.
EVALUATION OF ACUTE STENT RECOIL
Numerous studies have demonstrated that suboptimal stent expansion continues to contribute to adverse clinical events, even in this modern DES era with optimised antiplatelet regimens. In clinical settings, however, final stent expansion often fails to meet expected stent dimensions. Particularly when the stent delivery balloon is used for post-dilation, most stents achieve only <80% of diameter and <70% of cross-sectional area predicted by the inflation pressure and nominal compliance charts8. Technically, this suboptimal stent expansion can result from failure of the stent to expand fully to its nominal area during balloon inflation, acute recoil of the stent after balloon deflation, or a combination of the two mechanisms. Understanding these individual mechanical properties in different stent designs/materials is crucial not only for the development of next-generation stents but also for the establishment of optimal lesion selection and deployment strategies specific to currently available stents.
Although several studies have tried to address this issue using quantitative coronary angiography (QCA)7,9, the ability of angiography to measure stent dimensions precisely is limited by its low resolution and silhouette-based assessment of a three-dimensional (3D) stent structure10. Intravascular imaging can offer high-resolution cross-sectional assessment of the final stent dimensions, whereas current imaging catheters do not allow stent measurements during balloon inflation to distinguish the two mechanisms (i.e., underexpansion versus acute recoil). To overcome these limitations, a few studies utilised custom-built imaging devices, such as a 0.018-inch IVUS imaging core11 or a 3D optical contactless machine12, to evaluate acute stent recoil of bare metal stents (BMS) during balloon deflation. In the DES era, one case report demonstrated acute recoil of a first-generation sirolimus-eluting stent using a dedicated OCT wire similar to ours13. To the best of our knowledge, the present study is the first to provide systematic evaluation of stent expansion and acute recoil in various DES platforms, including the latest-generation cobalt-chromium and platinum-chromium stents, under identical conditions and post-dilatation protocol. While acute stent recoil was observed in all investigated stent types, the degrees of initial stent expansion and subsequent recoil were both considerably different among the stent materials/designs. The present study also revealed that optimal post-dilatation techniques could improve the final stent dimensions by reducing the degree of acute recoil at post-dilatation.
IMPACT OF STENT MATERIALS AND DESIGNS
Recent trends in metallic stent materials include cobalt-chromium or platinum-chromium alloys that enable thinner-strut stent designs compared with conventional stainless steel stents. Despite the theoretical advantages in flexibility and deliverability14 as well as long-term outcomes2, a concern has also been raised about possibly reduced radial strength that leads to greater stent recoil in thinner-strut cobalt-chromium stents than in stainless steel stents. In fact, controversial results have been reported with respect to the balloon inflation pressure required for cobalt-chromium versus stainless steel stents. For example, a small randomised series of patients reported that cobalt-chromium stents (ML VISION) required a higher balloon deployment pressure than the similarly designed stainless steel stents (ML ZETA®; Abbott Vascular) to achieve predefined IVUS criteria of optimal stent expansion15. Conversely, a recent retrospective IVUS study reported a higher maximum stent deployment pressure in stainless steel stents (TAXUS Liberté and CYPHER) than in cobalt-chromium stents (XIENCE/PROMUS) to reach comparable final stent dimensions8. In both studies, however, IVUS measurements were available only after balloon dilation, thereby precluding individual assessment of initial stent expansion and subsequent acute recoil. More recently, a clinical study evaluating the impact of stent materials/designs on acute recoil using QCA reported greater acute recoil with cobalt-chromium stents compared with stainless steel and platinum-chromium stents7. It is notable that their results were discordant with ours, in terms of platinum-chromium stents. Including the above three studies, all previous in vivo studies used original delivery balloons to evaluate stent expansion, the mechanical property and nominal pressure of which significantly differ from one to another. Combined with other potential confounding factors frequently seen in retrospective clinical studies, this methodological limitation raised the need for systematic evaluation of the initial stent expansion and subsequent acute recoil across a wide variety of commonly used stents, under standardised conditions with an identical non-compliant balloon for post-dilatation, as employed in the current bench test model.
In the present study, at deployment using the stent delivery balloon, the stent area during inflation was significantly smaller in stainless steel stents than in cobalt-chromium and platinum-chromium stents. This observation may be attributed to several factors, such as different stent characteristics including stiffness of the thicker-strut stainless steel stents, and the different original delivery balloon in each stent system. Of note, nominal pressure for the S-Stent semi-compliant delivery balloon is relatively low (6 atm) compared with other stent systems (9-12 atm). When the same non-compliant balloon was used for post-dilatation, all stents showed equivalent stent areas achieved during the inflation of the post-dilatation balloon. In clinical practice, higher-pressure balloon inflation for stent deployment is often performed rather than nominal pressure. However, the exact pressure considered appropriate for stent deployment can vary significantly among operators and institutions. Accordingly, an attempt was made to standardise the conditions of the bench test model as much as possible, by employing nominal pressure, which was offered by the manufacturer to expand the delivery balloon to 3 mm in diameter equally, to deploy the stents.
In contrast to the similar degrees of recoil detected during deflation of the stent delivery balloon among the three stent materials, cobalt-chromium and platinum-chromium stents showed significantly greater recoil at post-dilatation, resulting in smaller final stent areas than stainless steel stents. Because of the experimental model used in the present study (i.e., 3.0 mm stents deployed in a 3.0 mm silicone tube, followed by post-dilatation with a 3.25 mm balloon), the former observation is considered to represent predominantly intrinsic elastic recoil of each stent, while the latter probably resulted from compressive external force, suggesting slightly reduced radial strength of cobalt-chromium and platinum-chromium stents compared with stainless steel stents.
COMPARISON BETWEEN GENERATIONS IN COBALT-CHROMIUM STENTS
Given that the same material is used, differences in stent design can also affect stent expandability during balloon inflation, intrinsic elastic recoil at deflation, or radial strength against compressive external force. Both the Integrity and ML-8 stents are made from the same alloys as their prior-generation stents (Driver and ML VISION, respectively), but are designed to achieve better flexibility and conformability while preserving radial strength16. Thus, there was an interest in the behaviour of these latest-generation cobalt-chromium stents in the present study. At deployment, using the original stent delivery balloon, the stent area during inflation was significantly smaller in the latest-generation cobalt-chromium stents than in conventional cobalt-chromium stents. This may possibly be due to the difference in delivery balloon system, since both stent groups showed comparable stent areas achieved during post-dilatation inflation where the same non-compliant balloon and inflation pressure were applied. In addition, the difference in stent design between the generations may be another reason. At deflation of the deployment balloon, the degree of recoil was significantly less in latest-generation stents than in the conventional stents, suggesting improved intrinsic elastic recoil in latest-generation stents. At post-dilatation, the behaviour was similar between latest-generation and conventional stents, indicating that radial strength against compressive external force is maintained in latest-generation stents compared with prior-generation cobalt-chromium stents. In contrast to the substantial differences seen in comparisons among different material groups, the results observed among the different stent designs between the generations were largely similar. This suggests that different stent designs may affect overall stent performance (such as flexibility, conformability, crossability and side branch access) but may not have as much impact as stent material with respect to fundamental expandability and radial strength against compressive external force.
BALLOON INFLATION STRATEGY: SINGLE LONG INFLATION VS. MULTIPLE SHORT INFLATIONS
Stent expansion can also be influenced by procedural strategy, such as the duration or frequency of balloon inflation. To date, multiple studies have suggested that the duration of balloon inflation is important in achieving optimal stent expansion. One experimental study reported that the inflation periods of ≥30 seconds appeared adequate for optimal deployment of stainless steel stents17. Several in vivo studies using QCA, IVUS, or OCT also demonstrated that sufficiently longer balloon inflations (25-60 seconds or longer) resulted in better stent expansion compared with a shorter balloon inflation3-5. On the other hand, although the frequency of balloon inflation can be another important factor affecting stent expansion, the exact impact of multiple inflations on initial stent expansion and subsequent acute recoil have not been well understood. One study attempted to investigate the potential benefit of multiple inflations by comparing stent expansion between single and two-time balloon inflations in clinical patients6. In their comparison between patient groups of identical total inflation time, stent expansion after two five-second inflations (10 seconds in total) tended to be larger than after a single 10-second inflation (p=0.09). However, no significant difference was observed in other group comparisons with longer durations (p=0.57 for total 20 seconds, p=0.59 for total 40 seconds). In that clinical study, the usage of the original delivery balloons, the mixture of several types of DES and BMS, and variable target lesion characteristics might have contributed to the controversial results. Another clinical study also reported that multiple balloon inflations of the original delivery balloon were associated with a decreased risk of acute stent recoil, although the major limitation was its retrospective study design where the duration and the number of balloon inflations, as well as the selection of stent type and IVUS guidance, were all determined at the discretion of the operator, based on the clinical characteristics and angiographic/IVUS findings during the procedure7. Therefore, several essential questions remained to be addressed, including the relative importance of duration versus frequency, the primary component affected (expansion or recoil), and whether the optimal inflation strategy differs among different stent materials/designs. Accordingly, the current investigation employed a standardised bench-test study design with a predefined protocol to compare mechanical stent properties across a variety of stents.
In comparing post-deployment balloon inflation strategies tested in the present study, no significant differences were observed in stent areas achieved during balloon inflation between the single long inflation and the first short inflation. In contrast, the degrees of recoil after deflation of the first short inflation tended to be greater compared with those after a single long inflation. These results suggest that the duration of balloon inflation primarily affects the degree of acute recoil, rather than the degree of stent expansion during the inflation. Importantly, however, the degrees of recoil were significantly improved from the first to the third short inflation, resulting in a larger final stent area after multiple short inflations than a single long inflation, regardless of stent materials/designs. Several possible factors could be considered to account for this observation. For example, it is probably attributed to the physical properties of the metallic alloy, including the rigidity and plasticity in changing or keeping the form in response to continuous vs. repetitive force. Another factor potentially affecting the final stent expansion may be the change in expandability of the balloon by repetitive inflation. In this study, a brand-new balloon was used for the post-dilatation procedure in each stent, and therefore the balloon condition was considered identical among the stents. On the other hand, the expandability of the balloon from crimped to full inflation states may vary between the initial and the second/third inflations. In fact, multiple short inflations resulted not only in decreased acute recoil but also in slight increases of the stent areas during balloon inflation from the first to third attempts. These two hypothetical mechanisms might explain the effectiveness of repetitive inflations to achieve greater stent expansion. Taken together, longer inflation, divided into multiple inflations, may be recommended to obtain better final stent dimensions, particularly with cobalt-chromium and platinum-chromium stents, which appear to be more susceptible to acute recoil compared with stainless steel stents. In clinical settings, however, further investigation is warranted to confirm whether the balloon dilatation methods evaluated in this study have a practical impact on final stent expansion, and the procedure should be adjusted depending on the status of the target lesion and the clinical condition of the patient.
Study limitations
Several limitations should be noted in this experimental study. In general, bench test models may not exactly emulate the biomechanical properties of human arteries. Particularly, the silicone mock vessel used in the present study is not a stenosis model, although this model has a radial compliance of 5-7% per 100 mmHg, which is currently the industry standard for regulatory investigations18. While the overdilatation method applied in this study (i.e., using a 3.25 mm post-dilatation balloon in the 3.0 mm silicone mock vessel) could generate a certain degree of elastic recoil force, the exact compression force in diseased human coronary arteries, potentially with low radial compliance, has not been determined. The establishment of an official bench model mimicking a diseased human coronary artery is eagerly awaited. Last, each study stent was deployed using its original delivery balloon. These differ from each other, thereby potentially affecting the result at stent deployment. Using an identical delivery system would be ideal to assess the expandability of the stent from its initial crimped status to deployment, subtracting the influence of the performance of the delivery balloon. However, this artificial setting would not offer clinically applicable data as provided in the present study.
Conclusions
Real-time OCT revealed significant acute recoil in all stent types serving as the platform of major DES. Both stent materials/designs and post-dilatation strategies showed significant impacts on final stent expansion.
| Impact on daily practice Significant acute recoil at coronary stent implantation generally occurs even in this era with developed metallic platforms of drug-eluting stents. The degree of acute recoil can vary according to both stent materials/designs and balloon dilatation strategies. In daily practice, the longer inflation, divided into multiple inflations, may be recommended to achieve better stent expansion, especially in cobalt-chromium and platinum-chromium stents, which appear to be more susceptible to compressive external force compared with stainless steel stents. |
Acknowledgements
We thank Heidi N. Bonneau, RN MS, CCA, for her editorial review of the manuscript.
Conflict of interest statement
P. Yock receives grant support from Abbott Vascular, Medtronic, and Boston Scientific. The other authors have no conflicts of interest to declare.