“It is not enough to conquer; one must learn to SEDUCE”.
Voltaire (1694-1778)
In everyday practice, percutaneous coronary intervention using a bare metal stent (BMS) is still frequently performed and the chance of incurring in-stent restenosis (ISR) is not negligible. Different treatment modalities for BMS ISR are still an important area of discussion. One of the most appealing is the drug-eluting balloon (DEB). This device has been proven angiographically and clinically superior to an uncoated balloon in BMS ISR1,2. Moreover, in the same type of lesion, DEBs have also shown angiographic and clinical results at least comparable to first-generation drug-eluting stents (DES), with a trend towards lower angiographic restenosis and lower target lesion revascularisation3. Nowadays, the use of DEBs has received a class IIa recommendation for the treatment of BMS ISR according to the 2010 European Society of Cardiology guidelines.
The SEDUCE (Safety and Efficacy of a Drug elUting balloon in Coronary artery rEstenosis) trial is a randomised clinical trial comparing the iopromide-based paclitaxel DEB with the second-generation everolimus-eluting DES for the treatment of BMS ISR4. This study focuses on optical coherence tomography (OCT) findings at nine-month follow-up, with specific emphasis on the healing characteristics of the two devices in terms of stent strut coverage. This study is an important addition to the current literature on DEB versus second-generation DES. The RIBS V (Restenosis Intra-stent of Bare Metal stents: Paclitaxel-eluting Balloon vs. Everolimus-eluting Stent) trial has recently been published, using the very same devices as those used in the SEDUCE5. The RIBS V data are broadly in agreement with the SEDUCE data, with a slight angiographic superiority of DES over DEB but no clear clinical benefit. However, both studies remain largely underpowered for clinical endpoints. Nevertheless, no major trends have been seen in one or another direction and the actual event rates were very low with both devices, suggesting both therapies are very effective in treating BMS ISR. Thus, the choice of one device over the other can be left to the single operator based on her/his personal preference and expertise, and on possible comorbidities of the patient.
Possibly a more interesting analysis of the SEDUCE and the RIBS V trials focuses on the imaging modalities used to assess the performance of the two devices. Angiography (used in both trials), is a relatively simpler and cheaper modality than OCT; however, we can question its complete validity in the comparison of DEB versus DES. Indeed, with DES implantation there is a definite acute advantage in terms of angiographic luminal gain as compared to DEB and this advantage is maintained at follow-up, but the angiographic loss is comparable. This means that the antiproliferative power of both devices is broadly comparable, but the additional scaffolding provided acutely by the metallic cage of the DES allows for some extra luminal gain. Regrettably, no intravascular imaging modality was routinely used in SEDUCE or RIBS V just after the index procedure to assess the acute result of the device used. Serial intravascular imaging (before and after intervention as well as at follow-up) would lead to additional information about the mechanism of action of the different devices6.
In a recently published study from our group, we routinely performed serial OCT analysis before PCI with DEB for ISR and after the procedure, as well as at six-month follow-up7. In this study, we noted that the in-stent restenotic segment treated with DEB showed extensive dissections of the neointimal tissue just after DEB inflation. These dissections were left untreated because of the satisfactory angiographic result. At follow-up, all these dissections were completely healed, with restoration of a near circular lumen surface inside the lumen without a growth in neointimal volume (even with a trend towards neointimal volume reduction), and with no substantial angiographic late luminal loss (Figure 1). Extrapolating these findings to the DEB versus DES comparison, we can assume that these dissections seen only with OCT would impact on the quantitative angiographic analysis by influencing the automatic lumen border detection to determine a slightly smaller lumen diameter in the case of DEB only treatment, as these dissections remain somewhat “hanging” in the lumen. Meanwhile, with stent implantation these dissections would be compressed against the vessel wall. These phenomena would impact on acute gain of DEB as compared to DES and, given a similar antiproliferative power for both devices, the acute difference generated by the metal scaffold would also remain at follow-up.
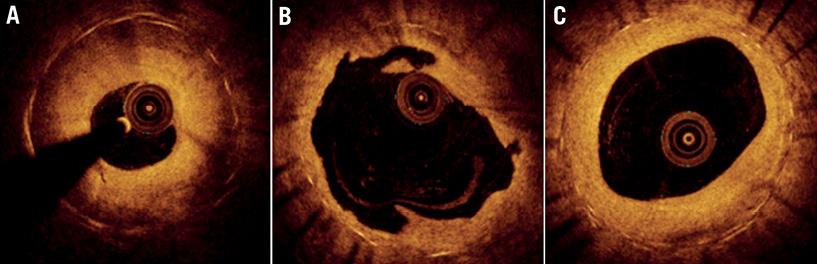
Figure 1. Serial optical coherence tomography findings in drug-eluting balloon treatment of in-stent restenosis. A) Preprocedural optical coherence tomography (OCT) image of a severe in-stent restenosis. B) Acute OCT final result after treatment with drug-eluting balloon with residual dissections clearly visible (OCT image at the same longitudinal location of the preprocedural OCT). C) OCT result at six-month follow-up with clear restoration of a near circular lumen border (OCT image at the same longitudinal location of preprocedural and post-procedural OCT).
From a methodological perspective, the classical angiographic endpoints are most probably not appropriate for comparisons of strategies which provide different acute gains (i.e., balloons and stents). We also believe they are not appropriate in case of comparison of devices with effective antiproliferative power leading to low late lumen loss (<0.4-0.5 mm), as these angiographic parameters are no longer predictive of the clinical need for target lesion revascularisation during follow-up8-11.
Optical coherence tomography provides more detailed images and better understanding of the mechanisms and course of the healing processes post intervention than angiography. It seems also to be a worthy tool to provide information about tissue prolapse, dissections, localised thrombus formation, minimal strut malapposition and detailed neointimal hyperplasia growth. It is foreseeable that OCT would help to provide essential insights in the future development of percutaneous coronary interventions. Considering also the large number of new devices rapidly appearing on the market (nowadays there are already several different DEBs available, most of them without proper clinical data), OCT appears the perfect tool to compare these devices and to assess their efficacy at a microscopic level. Studies using serial OCT may become the standard to assess new devices and compare them to the currently available devices in order to understand more quickly, and with a smaller number of patients, the properties and drawbacks of the new devices.
Conflict of interest statement
The authors have no conflicts of interest to declare.