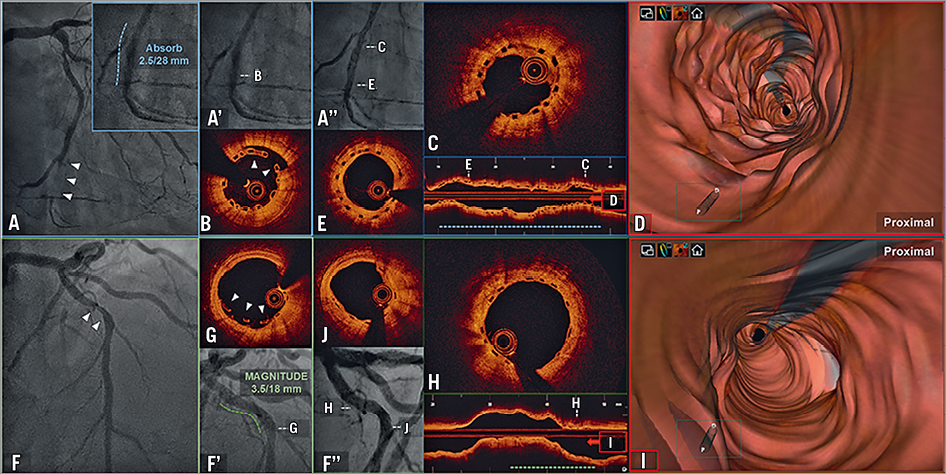
Figure 1. Serial CAG and OCT findings. Absorb BVS: baseline (A), 1-month (A’ and B) and 10-month follow-up (A’’ and C-E). MAGNITUDE: baseline (F), index procedure (F’ and G) and 9-month follow-up (F’’ and H-J). Dashed lines indicate lesion treated (blue: Absorb BVS, green: MAGNITUDE). Resolving strut malapposition of Absorb BVS (B: 1-month follow-up, E: 10-month follow-up) and MAGNITUDE (G: index procedure, J: 9-month follow-up). Comparison of neointimal coverage: thicker (Absorb BVS: C-E) and thinner (MAGNITUDE: H-J). 3D reconstruction demonstrating “undulated” neointimal BVS coverage (D) and “smooth” MAGNITUDE neointimal coverage (I).
A 46-year-old male underwent percutaneous coronary intervention (PCI) of a distal left circumflex (LCx) artery lesion (Figure 1A). After lesion preparation with a non-compliant (NC) balloon, a 2.5x28 mm bioresorbable scaffold (Absorb BVS; Abbott Vascular, Santa Clara, CA, USA) was implanted, and then post-dilated with a 2.5 mm NC balloon (20 atm). Intravascular ultrasound (IVUS) confirmed appropriate BVS expansion and strut apposition.
One month later, a staged PCI to the mid-left anterior descending artery (LAD) was performed (Figure 1F). Predilatation was performed with a 3.0 mm NC balloon and a 3.5x18 mm sirolimus-eluting bioresorbable scaffold (MAGNITUDE®; Amaranth Medical, Mountain View, CA, USA) was implanted (10 atm) (Figure 1F’). Optical coherence tomography (OCT) demonstrated well-embedded scaffolds except for focal minor malapposition at the distal edge (Figure 1G). OCT was also performed in the distal LCx previously treated with the BVS (Figure 1A’). This revealed thin neointimal strut coverage and focal minor malapposition in the mid segment with partial tissue bridging (Figure 1B).
Nine months later, a follow-up coronary angiogram revealed good angiographic results (Figure 1A’’, Figure 1F’’) and OCT showed homogeneous strut coverage without significant neointimal hyperplasia (NIH) in the MAGNITUDE-treated lesion (Figure 1H, Supplementary Table 1). In the distal LCx, all Absorb BVS struts were covered but partially thicker NIH was observed (Figure 1C). Notably, in the lesion after BVS implantation, the luminal surface appeared undulated, in contrast to the MAGNITUDE which was smoother (Figure 1D, Figure 1I). In both lesions, the initial malapposition resolved (Figure 1E, Figure 1J).
Vessel healing with neointimal formation is multifactorial, including device- and lesion-related factors. Strut thickness and vessel surface area coverage are associated with the haemodynamic microenvironment, affecting subsequent neointimal formation1. Although there was a difference in vessel size treated, the thinner struts and lesser footprint of the MAGNITUDE compared with the BVS (98 µm vs. 150 µm, and 22% vs. 32%) may have contributed to the favourable neointima. Furthermore, the degradation process of ultra-high molecular weight poly-L-lactic acid (PLLA) of the MAGNITUDE may differ from that of the BVS and result in different vessel healing. In contrast, the underlying plaque morphology may have influenced results, even though intravascular imaging showed that fibrotic plaque with mild calcification was the predominant subtype in both lesions.
Funding
Restoring Endoluminal Narrowing Using Bioresorbable Scaffolds - Extended Trial III (RENASCENT III): NCT02900937. This study is sponsored by Amaranth Medical Inc.
Conflict of interest statement
A. Latib has served on the advisory board for Medtronic and has received honoraria from Abbott Vascular. J. Granada has received research grants from Boston Scientific. The other authors have no conflicts of interest to declare.
Supplementary data
Supplementary Table 1. Quantitative comparison of OCT measurements: Absorb BVS vs. MAGNITUDE.
To read the full content of this article, please download the PDF.