Abstract
Background: Coronary computed tomography angiography (CCTA) and fractional flow reserve (FFR) derived from CCTA (FFR-CT) may provide a means of reducing unnecessary invasive coronary angiography (ICA) in patients with suspected non-ST-elevation acute coronary syndromes (NSTE-ACS).
Aims: The aim of this study was to evaluate the capacity of FFR-CT and CCTA to rule out significant lesions in high-risk NSTE-ACS patients, using ICA with invasive FFR as the gold standard.
Methods: High-risk NSTE-ACS patients admitted to 4 European centres were enrolled in this single-arm, prospective core lab-adjudicated study. Patients underwent CCTA with FFR-CT analysis, followed by ICA with invasive FFR.
Results: Out of the 250 initially planned NSTE-ACS patients, 168 were included, of whom 151 (92%) had sufficient CCTA image quality to undergo CCTA and FFR-CT analysis. The median high-sensitivity troponin T level at 1 hour post-hospitalisation was 5.3 (interquartile range: 1.8-18.6) times the upper reference limit. At the patient level, the diagnostic performance of FFR-CT was numerically higher as compared to CCTA though not statistically significant (sensitivity: 94% vs 93%, specificity: 63% vs 54%, positive predictive value: 83% vs 79%, negative predictive value: 85% vs 80% and accuracy: 83% vs 79%; p=0.58), suggesting an enhanced capability to avoid unnecessary ICA. At the lesion level, the ability of FFR-CT to detect significant lesions was significantly better than that of CCTA (receiver operating characteristic curves: 0.84 vs 0.65 respectively; p<0.01).
Conclusions: In patients with high-risk NSTE-ACS, FFR-CT offers better diagnostic accuracy – though not statistically significant – and a higher ability to rule out haemodynamically significant stenoses as compared to CCTA. This indicates that FFR-CT can reduce unnecessary invasive procedures by more accurately identifying patients requiring further intervention.
Whilst ST-elevation myocardial infarction (STEMI) can typically be diagnosed based on electrocardiogram (ECG) criteria alone, non-ST-elevation acute coronary syndrome (NSTE-ACS) can represent a diagnostic challenge. The combination of a clinical assessment and ECG criteria is often insufficient for an accurate diagnosis. In addition, although biomarkers such as troponin have a high positive predictive value for the diagnosis of myocardial infarction when markedly raised, the advent of high-sensitivity troponin (hs-Tn) has led to an increase in the number of patients with mildly raised hs-Tn, which has less discriminative power. This results in a significant number of patients being referred for invasive coronary angiography (ICA) who are ultimately found to have no significant epicardial stenoses. This proportion has been reported to be as high as 50% among patients with an increase in troponin of ≤3x the upper range limit (URL)1.
Coronary computed tomography (CT) angiography (CCTA) has been widely studied in the context of low- to intermediate-risk chest pain, demonstrating an excellent capacity to rule out the presence of significant coronary artery disease. Similarly, fractional flow reserve (FFR) derived from CCTA (FFR-CT) has also been extensively studied as a tool to avoid invasive assessment of intermediate coronary lesions in a stable setting2. However, to date, no study has evaluated the potential benefit of CCTA and FFR-CT in the setting of high-risk, troponin-positive NSTE-ACS.
Accordingly, in the present study, we investigated whether, in patients with high-risk NSTE-ACS, CCTA and FFR-CT were able to exclude the presence of haemodynamically significant coronary stenoses.
Methods
STUDY POPULATION
The detailed methodology of the study has been described previously3. It is important to note that recruitment was slower than expected during the COVID-19 pandemic, as many centres temporarily prohibited the inclusion of non-COVID studies to prioritise pandemic management. Additionally, CT scanners were heavily used for COVID patients, limiting their availability for this study. As a result, the study was extended to 3 additional centres following a similar study protocol. Thus, in total, the study recruited patients from 4 European centres (Lausanne, Switzerland; Monzino, Italy; Aalst, Belgium; and UZB, Belgium) between August 2019 and April 2022. Patients presenting to the hospital with symptoms of ischaemia and in whom a rise and/or fall of high-sensitivity troponin T (hs-TnT) was detected with at least 1 value above the 99th percentile of the URL were screened for inclusion1.
Given the requirement for the iodinated contrast administration for both CCTA and ICA, patients with a glomerular filtration rate (GFR) below 45 ml/min were not included. Pregnant and breastfeeding women, patients with prior coronary stenting, coronary artery bypass grafting (CABG), and patients with known severe heart failure (ejection fraction below 30%) were also excluded. Additionally, patients were excluded if they presented with STEMI or NSTE-ACS with 1 or more very high-risk criteria requiring urgent ICA, as per current European4 and American guidelines5. In accordance with these guidelines, NSTE-ACS patients were deemed high risk when they presented with a positive troponin level, showing a dynamic rise or fall, along with symptoms of ischaemia.
STUDY DESIGN AND PROCEDURE
The present study is a single-arm, double-blinded, core laboratory-adjudicated prospective trial. Patients admitted with high-risk NSTE-ACS and who agreed to participate in the study underwent CCTA followed by ICA within a recommended time window of 24 hours, as per guidelines. In parallel, patients benefitted from guideline-recommended medical management including cardiac monitoring and antithrombotic therapy.
CT SCAN ACQUISITION
CT acquisition was performed on a 256-slice multidetector CT (Revolution CT [GE HealthCare] or equivalent). Beta blockers (molecule and dosage left to the physician’s discretion) were administered before image acquisition, aiming for a heart rate <65 bpm. Additionally, one dose of sublingual nitroglycerine (400-800 mg)678 was administered. Parameters used for CT acquisition were as follows9: 80-100 kVp/550 mA for body mass index (BMI) <25 kg/m² (high definition mode), 100 kVp/550 mA for BMI between 25 and 30 kg/m², 120 kVp/600 mA for BMI >30 kg/m² (standard definition mode). For the CCTA acquisition, 80 ml of iodinated contrast was used. A lesion was defined as significant if it had a quantitative coronary angiography (QCA) lumen area stenosis >50%1011 (see Core-laboratory analysis section).
FFR-CT ANALYSIS
FFR-CT was computed offline by blinded investigators in a central FFR-CT core laboratory (HeartFlow, Redwood City, CA, USA). A haemodynamically significant lesion was defined as a lesion with an FFR-CT value of ≤0.80. Of note, the FFR-CT value was taken at the same arterial position as the invasive FFR measurement.
ICA AND FFR
ICA was performed following local and international best practices. FFR was measured in all lesions with a visual diameter stenosis ≥30% using the PressureWire X Guidewire (Abbott) using the following protocol: equalisation of the pressure wire and the aortic pressure was performed at the tip of the guide catheter prior to all measurements. The pressure wire was then advanced distal to the stenosis. Hyperaemia was obtained using intracoronary adenosine (100 μg for the right coronary artery and 200 μg for the left coronary artery). At the end of the procedure, the absence of drift was confirmed by pulling back the pressure wire to the initial equalisation site.
BLINDING
Patients, as well as physicians performing ICA, were blinded to the results of CCTA. For obvious ethical reasons, relevant extracardiac findings were communicated to the treating physician to ensure adequate follow-up and/or treatment.
CORE LABORATORY ANALYSIS
In order to guarantee adequate blinding and provide high-quality standardised analysis, all data from ICA, CCTA, and FFR-CT were collected and analysed in a central core laboratory (CoreAalst BV, Aalst, Belgium). ICA images were analysed with three-dimensional (3D) QCA software (CAAS 8.2 Workstation [Pie Medical Imaging]). For ICA, a haemodynamically significant lesion was defined as a lesion with an FFR value of ≤0.80. FFR was not measured in case of very severe stenosis (>90%) or an occluded vessel. In this case, an arbitrary value of 0.50 was attributed to the vessel as previously described12. CCTA data were analysed using validated software (QAngio CT [Medis Medical Imaging]) by the core laboratory. Measurements were automatically generated by the software, and the analyst manually adjusted luminal contours when necessary. A significant lesion was defined as a QCA lumen area stenosis >50%. For FFR-CT, a haemodynamically significant lesion was defined as a lesion with an FFR-CT value of ≤0.80. A final database with each vessel analysed with each modality (ICA, CCTA and FFR-CT) was then generated by the core laboratory. For the purpose of simplicity, the coronary anatomy was segmented into three main vessels: left anterior descending artery, left circumflex artery and right coronary artery. Each side branch was adjudicated as pertaining to the main branch.
ENDPOINTS
The primary endpoint was the ability of FFR-CT and CCTA to rule out the presence of significant lesions as defined by the invasive evaluation (i.e., the negative predictive value [NPV]) at the patient level. Secondary endpoints were the sensitivity, specificity, positive predictive value (PPV) and accuracy of FFR-CT and CCTA compared to the invasive evaluation at the patient level. Additionally, the misclassification rate for each strategy was calculated, and analyses were also conducted at a vessel level.
SAMPLE SIZE DETERMINATION AND STATISTICAL ANALYSIS
With the latest iteration of the FFR-CT software, the per-patient sensitivity and specificity were 86% (95% confidence interval [CI]: 77-92%) and 79% (95% CI: 72-84%), respectively13. In the VERDICT-EDI trial based on non-STEMI (NSTEMI) patients14, 12% had 3-vessel disease, 23% had 2-vessel disease (which included the left main), 34% had 1-vessel disease, and 30% had no significant disease. Thus, out of 100 patients with 300 coronary arteries, 116 (i.e., 36+46+34) vessels with a stenosis were expected in our study. Based on the FAMOUS NSTEMI trial15, 60% of invasive FFR measurements of stenoses were significant16. Thus, with a standard error of 0.05 and for a power of 80%, 204 patients were required. However, as it was expected that a proportion of CCTA images would not be suitable for analysis, a sample size of 250 patients was targeted. Statistical analyses were carried out with SPSS Statistics 25.0 software (IBM) and Stata, version 14.3 (StataCorp). Comparisons of diagnostic performance (sensitivity, specificity, accuracy) were performed using a paired McNemar test.
ETHICS
This project was approved by the local ethics board of each institution. The study was conducted in accordance with the study protocol, the Declaration of Helsinki, the principles of Good Clinical Practice, the Human Research Act (HRA) and the Human Research Ordinance (HRO) as well as other locally relevant regulations.
Results
PATIENT POPULATION
Due to slower-than-expected enrolment related to the COVID-19 pandemic, study enrolment was stopped prematurely after reaching two-thirds of the planned sample size. In total, 168 patients presenting with high-risk NSTE-ACS were recruited between August 2019 and April 2022. The heart rate of 4 patients was too high to undergo adequate CCTA acquisition, and they were excluded. Due to insufficient image quality for CCTA12 and/or FFR-CT analysis1, 13 other patients (8%) were excluded, leaving a total of 151 patients for the final analysis. In 12 cases, an FFR-CT analysis would have been possible, even though a CT-only analysis was not, but by study design, these patients were excluded.
Baseline patient characteristics are reported in Table 1. The mean age was 63±12 years, and 70% of patients were male. The vast majority of patients (96%) presented with chest pain, while shortness of breath and nausea were less common (29% and 10%, respectively). In total, 60% of patients had ECG changes consistent with ischaemia or bundle branch block. The median hs-TnT level at 1 hour post-hospitalisation was 5.3 (interquartile range: 1.8-18.6) times the URL.
Table 1. Patients’ baseline characteristics and clinical presentation.
| Characteristic | n=151 |
|---|---|
| Age, years | 63±12 |
| Male | 106 (70) |
| BMI, kg/m² | 28±2 |
| Cardiac risk factors | |
| Active or former smoker | 103 (68) |
| Hypercholesterolaemia | 88 (58) |
| Hypertension | 74 (49) |
| Diabetes | 19 (13) |
| Peripheral artery disease | 5 (3) |
| Clinical presentation | |
| Chest pain | 145 (96) |
| Shortness of breath | 44 (29) |
| Nausea/vomiting | 15 (10) |
| ECG findings | |
| Normal ECG | 45 (40) |
| ST depression | 16 (14) |
| T wave inversion | 34 (30) |
| RBBB | 3 (3) |
| LBBB | 10 (9) |
| 1 hr troponin elevation (number of times above URL) | 5.3 (1.8-18.6) |
| Values are expressed as n (%), mean±SD or median (Q1-Q3). BMI: body mass index; ECG: electrocardiogram; LBBB: left bundle branch block; Q: quartile; RBBB: right bundle branch block; SD: standard deviation; URL: upper range limit | |
ICA FINDINGS AND TREATMENT DECISION
A total of 99 patients (66.0%) had at least 1 significant lesion (either diameter stenosis >90% or with a diameter stenosis between 30% and 90% with an FFR ≤0.80). The remaining 52 patients (34.4%) either had no lesion with a diameter stenosis >30% on ICA or had a lesion with a diameter stenosis between 30% and 90% with an FFR>0.80). FFR was measured in a total of 106 lesions in 68 patients (45%). The majority of patients had 1- (34.4%) or 2-vessel (44.4%) disease. After ICA, 64% of patients were treated with percutaneous coronary intervention (PCI), 33% were managed conservatively, and 3% were referred for CABG surgery (Table 2).
Table 2. Coronary angiography findings and treatment.
| Coronary angiography findings | n=151 |
|---|---|
| Patients with at least one significant lesion | 99 (66) |
| Extent of coronary artery disease | |
| None | 52 (34.4) |
| Single vessel | 67 (44.4) |
| Two vessels | 23 (15.2) |
| Three vessels | 9 (6.0) |
| Patients with at least 1 FFR measurement performed | 68 (45) |
| Total number of FFR measurements performed | 106 |
| Mean FFR value | 0.71±0.36 |
| Treatment decision | |
| Conservative | 49 (33) |
| PCI | 97 (64) |
| CABG | 5 (3) |
| Values are expressed as n (%), n, or mean±SD. CABG: coronary artery bypass grafting; FFR: fractional flow reserve; PCI: percutaneous coronary intervention; SD: standard deviation | |
PERFORMANCE OF FFR-CT AND CCTA AT THE PATIENT LEVEL
The ability of FFR-CT to rule out the presence of a significant lesion (NPV − predefined primary endpoint) was numerically higher than with CCTA (85% vs 80%, respectively). A similar trend was also observed for the other diagnostic parameters (secondary endpoints): 94% versus 93% for sensitivity, 63% versus 54% for specificity, 85% versus 80% for PPV, and 83% versus 79% for accuracy (Figure 1). However, this trend was not statistically significant (p=0.58).
Depending on the strategy used, the rate of misclassification varied notably. Using a guideline-based strategy with referral to ICA if appropriate, 34% of patients were assigned to undergo unnecessary ICA. Conversely, when employing a CCTA- or FFR-CT-based strategy, the rate of misclassification decreased to 21% and 17%, respectively (p<0.01) (Figure 2). A summary of the performance of CCTA and FFR-CT is shown in Table 3. Finally, the rate of potentially avoidable ICA (i.e., true negatives) would have been 19% with a CCTA-based strategy and 22% with an FFR-CT-based strategy.
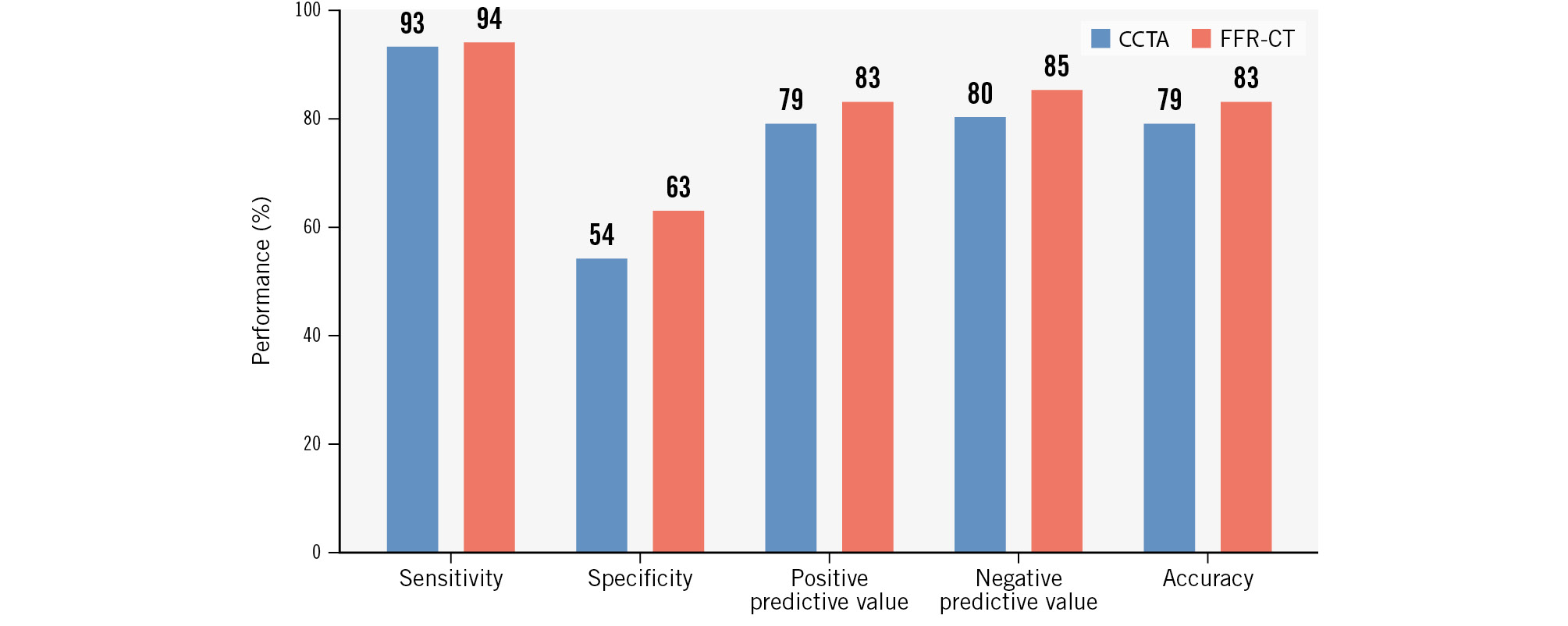
Figure 1. Diagnostic performance of CCTA (blue) and FFR-CT (red) at the patient level with invasive FFR as the gold standard. CCTA: coronary computed tomography angiography; FFR: fractional flow reserve; FFR-CT: FFR derived from CCTA
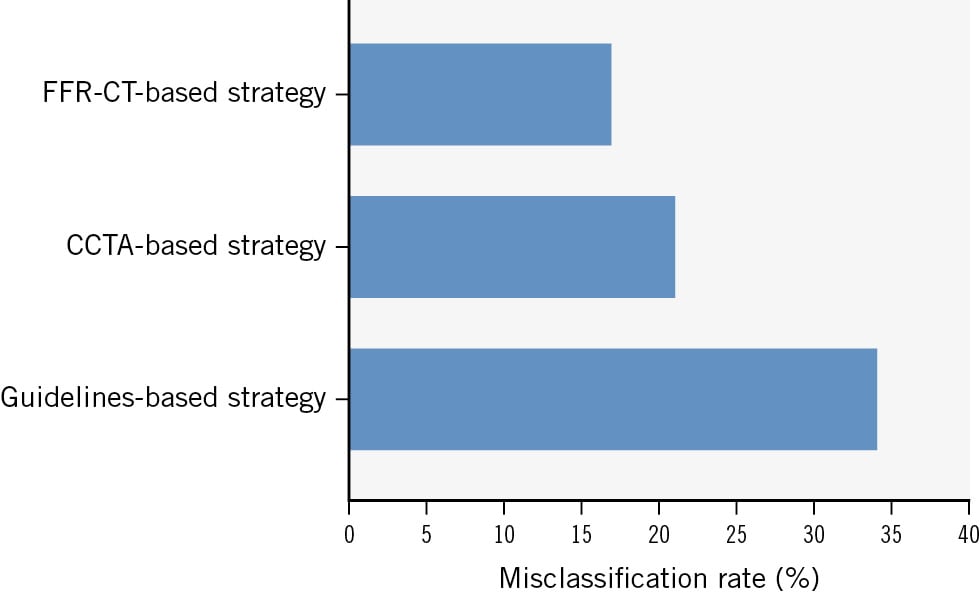
Figure 2. Percentage of misclassification (wrong positives and wrong negatives) of a guideline-based approach, a CCTA-based strategy, and an FFR-CT-based strategy. CCTA: coronary computed tomography angiography; FFR-CT: fractional flow reserve derived from CCTA
Table 3. Performance of CCTA and FFR-CT at the patient level (n=151).
| Angiography (gold standard) | CCTA | FFR-CT | |
|---|---|---|---|
| True positive | 99 | 92 | 93 |
| True negative | 52 | 28 | 33 |
| False positive | - | 24 | 19 |
| False negative | - | 7 | 6 |
| Sensitivity, % | - | 93 | 94 |
| Specificity, % | - | 54 | 63 |
| Positive predictive value, % | - | 79 | 83 |
| Negative predictive value, % | - | 80 | 85 |
| Accuracy, % | - | 79 | 83 |
| Values are n, or % where indicated. CCTA: coronary computed tomography angiography; FFR-CT: fractional flow reserve derived from CCTA | |||
PERFORMANCE OF CCTA AND FFR-CT AT THE VESSEL LEVEL
Figure 3 displays the percentage stenosis in terms of QCA according to modality (ICA vs CCTA). A total of 459 vessels were analysable in all 3 modalities (ICA, CCTA and FFR-CT). Overall, the performance of FFR-CT was better, mostly because of an increased specificity. On receiver operating characteristic analysis, the area under the curve was significantly higher for FFR-CT as compared with CCTA (0.85 vs 0.64; p<0.01) (Central illustration). At the vessel level, the NPV of FFR-CT and of CCTA were similar (92% vs 92%). Sensitivity was slightly lower for FFR-CT compared to CCTA (83% vs 87%), while the other diagnostic parameters were all in favour of FFR-CT: 81% versus 70% for specificity, 67% versus 56% for PPV, and 82% versus 75% for accuracy (Table 4).
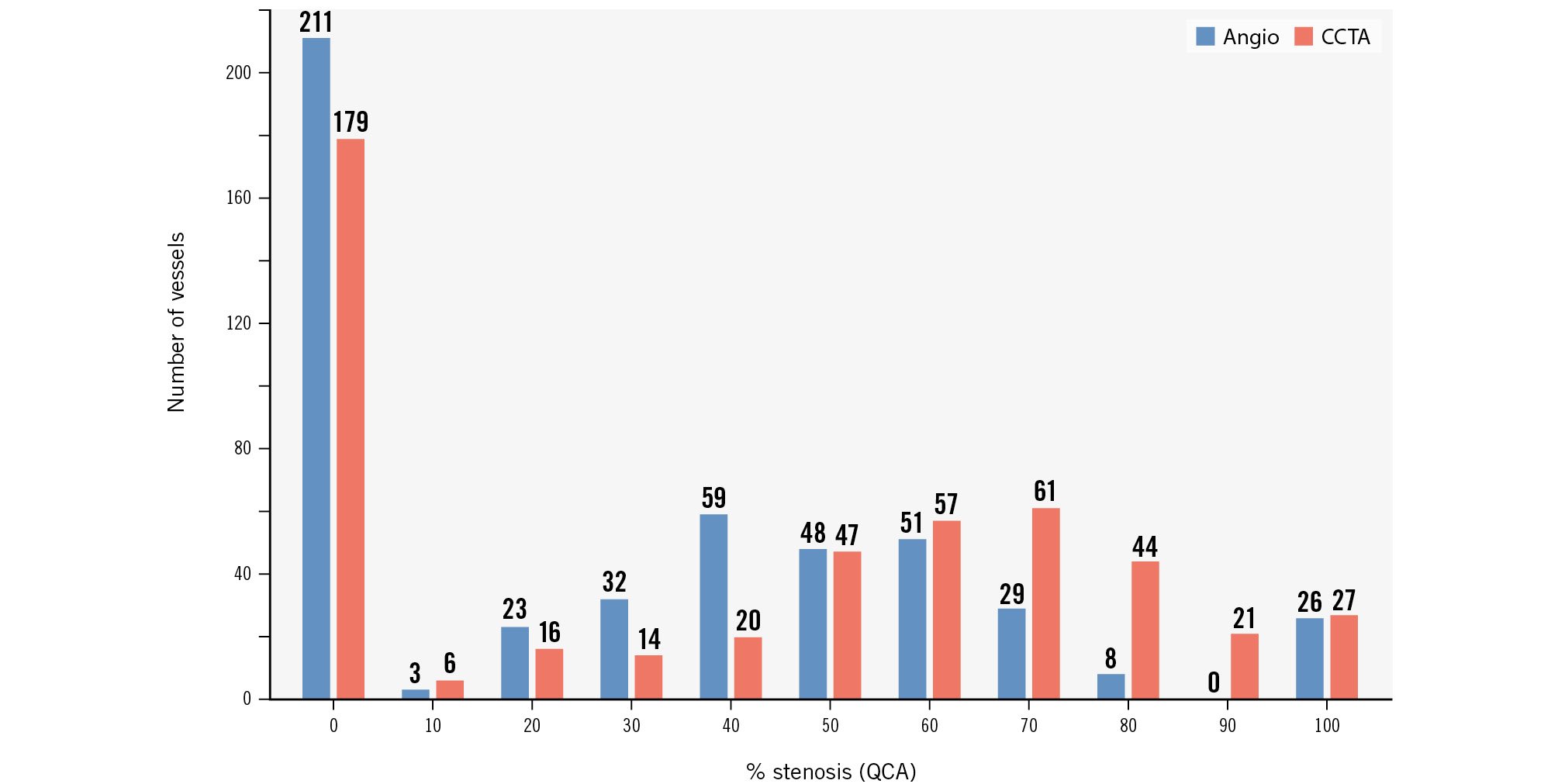
Figure 3. Percentage stenosis in terms of QCA according to modality (angiography in blue and CCTA in red). CCTA: coronary computed tomography angiography; QCA; quantitative coronary angiography
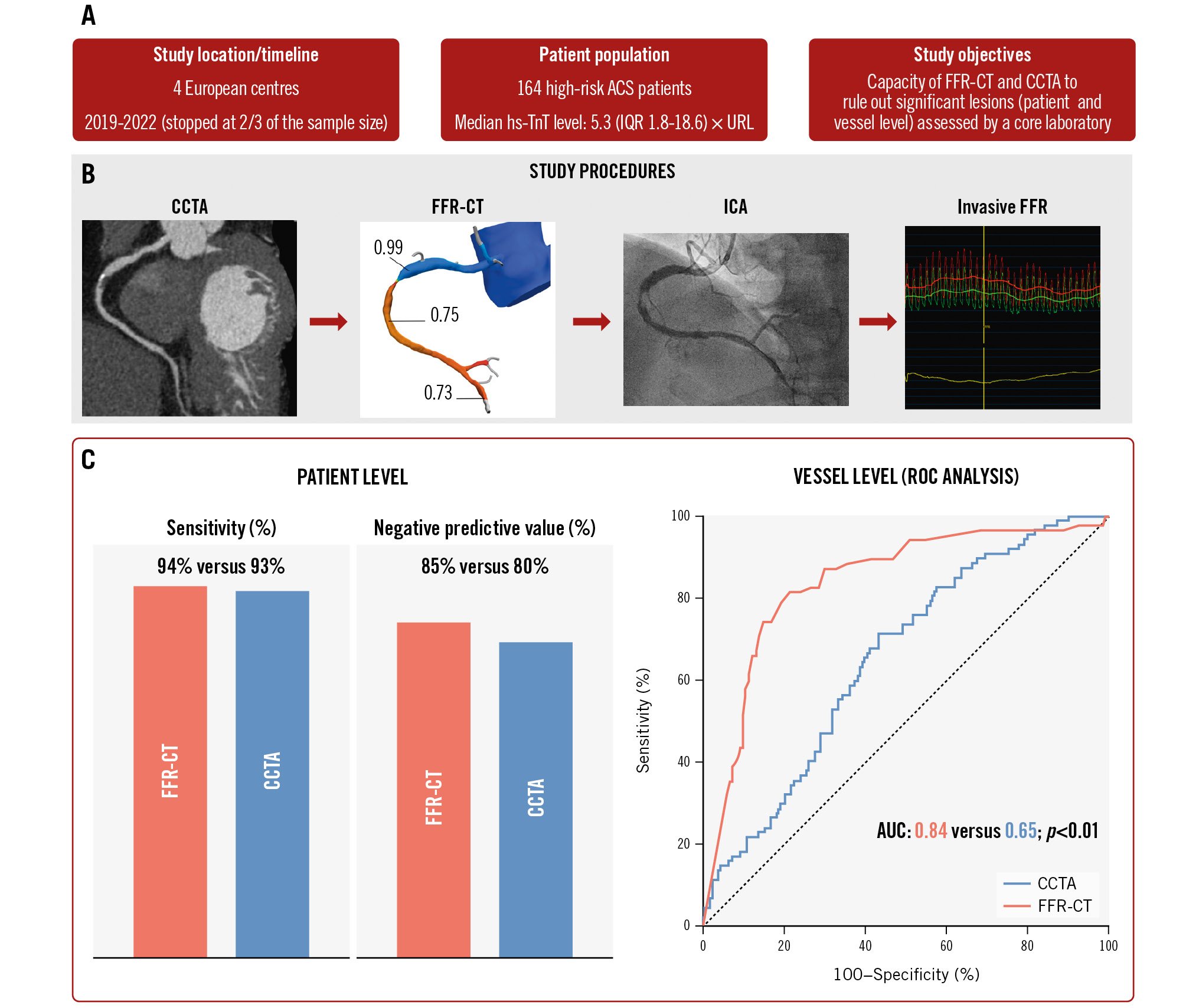
Central illustration. Usefulness of FFR-CT in patients with high-risk NSTE-ACS. A) Study summary; (B) study procedures; and (C) patient- and vessel-level results. In patients with high-risk NSTE-ACS, FFR-CT offers better diagnostic accuracy and a higher ability to rule out haemodynamically significant stenoses as compared to CCTA, with the potential to reduce unnecessary invasive procedures. ACS: acute coronary syndrome; AUC: area under the curve; CCTA: coronary computed tomography angiography; FFR: fractional flow reserve; FFR-CT: FFR derived from CCTA; ICA: invasive coronary angiography; IQR: interquartile range; NSTE-ACS: non-ST-elevation acute coronary syndrome; ROC: receiver operating characteristic; URL: upper range limit
Table 4. Performance of CCTA and FFR-CT at the vessel level (n=459)
| Angiography (gold standard) | CCTA | FFR-CT | |
|---|---|---|---|
| True positive | 141 | 123 | 117 |
| True negative | 318 | 222 | 259 |
| False positive | - | 96 | 59 |
| False negative | - | 18 | 24 |
| Sensitivity, % | - | 87 | 83 |
| Specificity, % | - | 70 | 81 |
| Positive predictive value, % | - | 56 | 67 |
| Negative predictive value, % | - | 92 | 92 |
| Accuracy, % | - | 75 | 82 |
| Values are n, or %, where indicated. CCTA: coronary computed tomography angiography; FFR-CT: fractional flow reserve derived from CCTA | |||
Discussion
The present study is the first to systematically assess the performance of FFR-CT and CCTA, as compared with ICA with invasive FFR, in the context of high-risk, troponin-positive NSTE-ACS. The main findings can be summarised as follows (Central illustration): (1) in this high-risk population, 34.4% of patients were found to be without significant coronary artery disease; (2) both CCTA and FFR-CT demonstrated the capacity to avoid unnecessary ICA, but FFR-CT had a numerically higher – although statistically non-significant – diagnostic accuracy compared to CCTA, particularly in terms of its slightly higher NPV; and (3) at the vessel level, FFR-CT exhibited significantly better diagnostic accuracy as compared with CCTA alone.
Taken together, the present data suggest that the use of CCTA (alone or in combination with FFR-CT) has the potential to optimise the management of NSTE-ACS by optimising patient selection for ICA.
Despite meeting all the criteria for NSTE-ACS including elevated troponin, a significant proportion of patients were found to be without significant obstructive coronary artery disease. This raises important questions regarding the limits of the current state-of-the-art diagnostic approach. Indeed, all the patients included in the present study met guideline-based indications for an early invasive strategy (i.e., within 24 hours). However, in more than one-third of these patients, this invasive strategy was not able to find an actionable coronary cause for their symptoms. This finding has important implications both in terms of unnecessary exposure to procedural risks and healthcare costs. As a consequence, the development of a non-invasive screening approach is highly relevant to current clinical practice.
In the present study, the use of CCTA or FFR-CT would have avoided between 54% and 64% of unnecessary invasive assessments. CCTA as an adjunctive diagnostic tool has already been studied in the past, albeit in different subpopulations. In a meta-analysis of 9 studies (n=1,349 patients), CCTA presented an overall high negative predictive value to exclude ACS in patients presenting to the emergency department with chest pain and suspected ACS17. The sensitivity of CCTA for NSTE-ACS diagnosis was 95% (95% CI: 88-100%), and specificity was 87% (95% CI: 83-92%), yielding a negative likelihood ratio of 0.06 (95% CI: 0-0.14) and a positive likelihood ratio of 7.4 (95% CI: 4.8-10.0). However, in these studies, patients were in the low-to-intermediate chest pain risk category with normal initial cardiac biomarkers, none had evidence of ischaemia on initial ECGs, and an NSTE-ACS was subsequently diagnosed in only 10% of patients (as opposed to 66% in the present cohort). Additionally, none of the previously published studies systematically evaluated the performance of CCTA and FFR-CT against FFR − the invasive gold standard in such a high-risk population. In the present patient population and similarly to prior studies, FFR-CT showed an increased specificity and ability to rule in significant lesions, thus, further limiting the number of patients sent unnecessarily for invasive evaluations13. Importantly, this did not come at the price of a lower sensitivity, and the number of false negative cases was similar for CCTA and FFR-CT (7 vs 6 patients). Of note, in the present study, CCTA data were adjudicated by a core laboratory. In the PROMISE study, the use of a core laboratory reclassified 16% of the patients compared to site-adjudicated results18. In comparison, FFR-CT analysis and reporting is an automated process with no reader-to-reader variability. Taken together, these two elements suggest that the actual difference between CCTA and FFR-CT performance might be larger in a real-world setting where CCTA can be adjudicated by physicians with varying degrees of expertise.
Additionally, for patients who ultimately undergo ICA, the prior implementation of an FFR-CT-based strategy has the potential to streamline the invasive evaluation. By providing detailed insights into the haemodynamic significance of specific coronary lesions, FFR-CT may reduce or even eliminate the need for additional invasive FFR measurements.
The current results also show that, despite being challenging (as illustrated by the slow enrolment rate), a strategy of CCTA first followed by ICA is feasible within the guideline-recommended window of 24 hours. However, this requires a strong collaboration between emergency, radiology and cardiology departments.
The results of the present study pave the way for future larger studies that should aim at clarifying the group of patients in which a first-line strategy of CCTA+FFR-CT is most effective and safe. Ultimately, a randomised trial assessing the impact of a CCTA-first strategy, compared to usual care, on hard clinical endpoints in patients with high-risk NSTE-ACS will be needed. Finally, the cost-effectiveness of such an approach will need to be evaluated. However, this is a complex aspect since, beyond the avoidance of unnecessary ICA, CCTA+FFR-CT also offer the possibility of avoiding invasive physiological measurements in intermediate lesions. Moreover, CCTA is gaining interest as a tool for effective PCI planning192021.
Limitations
This study has limitations related to its non-randomised design, relatively small sample size and the fact that it had to be stopped before reaching the targeted sample size. Moreover, the present cohort represents a relatively select population as patients with low GFR, prior PCI/CABG and severe heart failure were excluded. The prevalence of patients with no significant coronary artery disease in our study may indicate that, while meeting the high-risk ACS criteria, they were potentially at slightly lower risk than in other studies15. However, these limitations are compensated by the multicentric nature of the study and the core laboratory adjudication of all imaging data, ensuring proper blinding and high-quality data. Finally, this study focused on physiological assessment, and it cannot be excluded that systematic use of intravascular imaging might have occasionally identified plaque erosion or rupture in patients without FFR-significant lesions, thus, unmasking an occult culprit lesion.
Conclusions
In high-risk NSTE-ACS, FFR-CT not only offers improved diagnostic accuracy as compared to CCTA but also exhibits the capacity to rule out significant lesions. It demonstrates greater specificity and positive predictive value, significantly surpassing CCTA at the lesion level. This suggests that FFR-CT could reduce unnecessary invasive procedures (and simplify these) by more accurately identifying patients requiring further intervention. However, these findings need to be confirmed in larger studies or in a randomised trial as this study was prematurely stopped with a smaller patient population than initially planned, thus, limiting the statistical power of its findings.
Impact on daily practice
This preliminary multicentre, international, core lab-adjudicated study suggests that fractional flow reserve (FFR) derived from coronary computed tomography angiography (FFR-CT) may help reduce unnecessary coronary angiographies in high-risk acute coronary syndrome patients. However, before being widely implemented, these findings need further confirmation. The successful application of this approach in hospitals requires well-established protocols and close collaboration with radiology departments, as both tests must be completed within 24 hours. Additionally, although rare in our study, there is a potential limitation if FFR-CT analysis is not feasible. While this strategy adds approximately 80 cc of contrast for patients who ultimately undergo coronary angiography, it provides a complete analysis of the coronary tree, reducing the need for additional contrast use for FFR measurements in non-culprit vessels. It also simplifies the procedure overall, as it begins with a wealth of information from the FFR-CT. For patients with a negative FFR-CT, this algorithm allows for early discharge, saving contrast and optimising hospital resources.
Funding
The present project is funded by a grant from the “Fondation Vaudoise de Cardiologie Interventionnelle”.
Conflict of interest statement
D. Meier has received an institutional grant from Edwards Lifesciences. T. Mahendiran is supported by a grant from the Swiss National Science Foundation (SNSF). D.C. Rotzinger receives consultancy compensation from GE HealthCare. B. De Bruyne receives grant support from Abbott, Boston Scientific, Biotronik, and St. Jude Medical; receives consulting fees from St. Jude Medical, Opsens, and Boston Scientific, outside of the submitted work; and is a shareholder in Siemens, GE HealthCare, Bayer, Philips, HeartFlow, Edwards Lifesciences, and Celyad. C. Collet reports receiving research grants from Biosensors, HeartFlow, and Abbott; and consultancy fees from HeartFlow, Abbott, and Philips/Volcano. S. Fournier reports speaker fees from Medtronic, CathWorks, Biotronik, and Amgen. The other authors have no conflicts of interest to declare.