![]()
Abstract
In the United Kingdom, a clinical data set is completed for every patient undergoing coronary intervention and certain structural interventions, and sent to central servers in the National Institute for Cardiovascular Outcomes Research (NICOR) on behalf of the British Cardiovascular Intervention Society (BCIS). These data are linked to the national mortality register. In addition, data are obtained about the structure of healthcare provision using an annual survey. Analyses of these data are provided for different audiences in several formats. Public reports of individual consultant operator activity and risk-adjusted outcomes from percutaneous coronary intervention (PCI) have also been produced annually since 2012.
Transcatheter aortic valve implantation (TAVI) has been performed since 2007. Over 2,000 cases were performed in 2015, giving a rate of 30 per million population. Complications to discharge have fallen as case mix has changed and technologies improved. While the mean age has remained about 81 years, the logistic EuroSCORE of patients treated by TAVI has fallen from about 22 in 2010 to 18 in 2015. Tracked 30-day mortality was 3.7% in 2014. Left atrial appendage occlusion and patent foramen ovale (PFO) closure for stroke, and the use of the MitraClip® system (Abbott Vascular, Santa Clara, CA, USA) for mitral regurgitation have been funded through a process called “commissioning through evaluation”.
Introduction
Data regarding adult coronary interventions in the United Kingdom (UK) have been collected since 1988 at the inception of the British Cardiovascular Intervention Society (BCIS). Initially a paper-based system, in 1996 the Department of Health approved a pilot scheme to attempt to collect data on every percutaneous coronary intervention (PCI) procedure electronically, and send encrypted data to central servers for analysis. By 2000, an established programme was agreed, and from about 2005 almost every PCI centre in the UK has participated in this process. Since 2010 these data have been collected by the National Institute for Cardiovascular Outcomes Research (NICOR) on behalf of BCIS. For every patient undergoing coronary intervention and those undergoing certain structural interventional procedures a data set relating to that patient and procedure is collected and sent in an encrypted format to central servers in NICOR for analysis1. In addition, each year a survey is sent to each interventional centre to gather data about the structure of healthcare provision. Analyses of these data are provided for different audiences in several formats. Each year an annual overview of activity and outcomes is provided (all are available for free download from the BCIS web site www.bcis.org.uk). Public reports of individual consultant operator activity and risk-adjusted outcomes from PCI have also been provided annually since 2012 and can be accessed in the “patient” area on the BCIS web site (Figure 1A). In addition, automated reports that focus on delays to emergency PCI, overall PCI activity and risk-adjusted outcomes (Figure 1B) are sent to each PCI centre on a monthly and quarterly basis. Centres and operators can create their own reports at any time for any date range via a professional web portal. These reports are designed to help with local data validation and to provide reports that can be used for professional appraisal and revalidation.
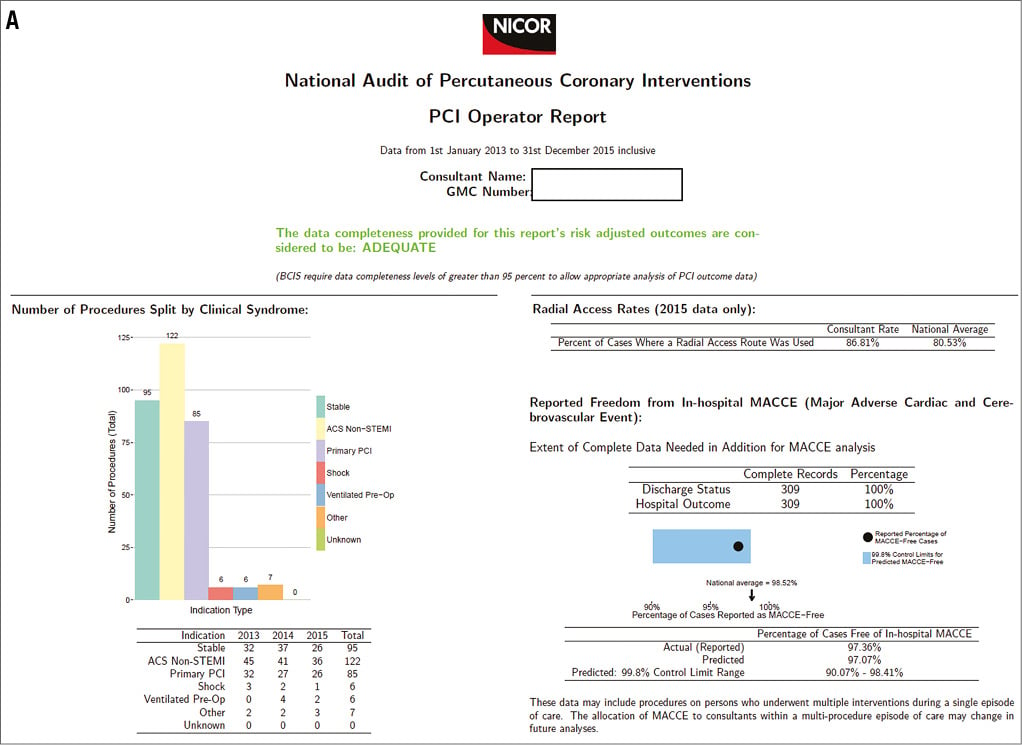
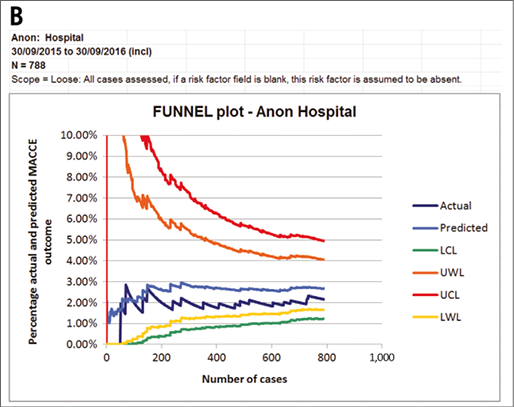
Figure 1. Two examples of displays of data from the PCI database for different audiences. A) An example of part of the 2016 public report of a consultant PCI operator. B) A cumulative funnel plot as sent to all UK hospitals every quarter. The observed adverse outcome rates are plotted as a cumulative running mean for each successive case (dark blue line: Actual), and are compared with “Predicted” adverse rates from a model2, and the warning limits (2 standard deviations) and control limits (3 standard deviations). LCL: lower control limit; LWL: lower warning limit; MACCE: major adverse cerebrovascular and cardiovascular events; UCL: upper control limit; UWL: upper warning limit
Case ascertainment is assessed by comparing declared total activity in the annual survey with the number of cases uploaded to the central database. Data completeness is measured with a focus on key fields required for assessment of risk-adjusted outcome, and quality is driven up by open reporting of these measures. There is no external validation of the data submitted, but a series of logical checks for internal consistency is applied, as are range checks on values. The accuracy of most outcome data is therefore dependent on accurate reporting by centres. However, independent assessment of mortality is provided by linkage to the mortality register held by the Office of National Statistics (ONS) (although this applies only to people living in England and Wales, not Scotland or Northern Ireland). Centres have an opportunity to validate their data before it is made publicly available.
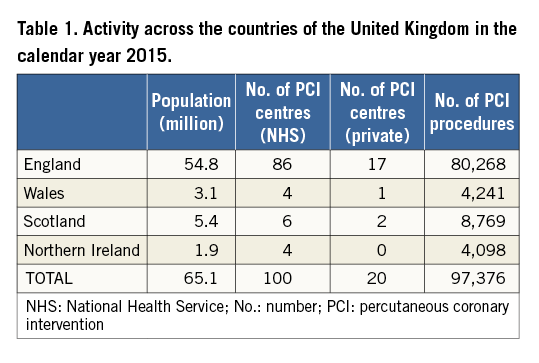
Demographics and organisation
There are four countries in the United Kingdom. Their population, the number of PCI centres and activity in the calendar year 2015 are presented in Table 1. TAVI was performed in thirty-three cardiothoracic surgical centres in the UK (which represents almost every surgical centre). This includes one centre in Scotland, one in Northern Ireland, two in Wales and the remainder in England.
Coronary interventions
The vast majority of PCI is performed in National Health Service (NHS) hospitals (98.8% of procedures in 2015). These centres are reimbursed by central government according to a tariff-based system linked to activity and adjusted for case mix. Current tariff levels for PCI are graded according to the number of stents used, and whether rotational atherectomy, intravascular imaging or pressure wires were also used during the procedure. In future, it is planned to include a measure of patient comorbidity.
STRUCTURE
Of the NHS PCI centres, 36% had on-site cardiac surgery, and performed 59% of all the PCI procedures. Sixty-nine provided a primary PCI service to treat patients presenting with ST-elevation myocardial infarction (STEMI) 24/7/365. Ten of these centres had no accident and emergency (A&E) department on site, and so only treated patients diagnosed with ST-elevation by the emergency services, with direct admission to their catheter laboratories. The others also received patients direct from the emergency services, but in addition treated patients initially seen in A&E.
In 2015 there were 647 interventional cardiology consultants in the UK, with an average of 7.5 working in each NHS centre, performing on average 126 cases per annum each.
APPROPRIATENESS
The mean age of patients treated by PCI was approximately 65 years, 74% were male and 21% diabetic. Current smokers represented 24%, and 26% had had a previous PCI and 8% previous coronary artery bypass surgery (CABG). Acute coronary syndromes accounted for the majority of activity, 27.3% for STEMI, and 37.3% for non-ST-elevation myocardial infarction or unstable angina (NSTEMI or UA), and 32.4% treated for stable symptoms.
The treatment of STEMI changed quite rapidly from thrombolysis to primary PCI over the years 2006 to 2011. By 2013, primary PCI had been established across the country, and the rate of primary PCI per million population (pmp) levelled off at about 385 by 2015 (varying in different regions from about 300 to 500 pmp). The use of PCI in patients with out-of-hospital cardiac arrest has been gradually increasing. Although in 2015 such cases accounted for 1.53% of all PCI activity, there was marked variation by centre, with these patients comprising 4% of all PCI procedures in some hospitals.
Coronary anatomy is recorded in the data set by epicardial territory, not by lesion. The percentage of patients with one, two or three epicardial territories subtended by a stenosed artery (stenosis >75%) was 68.4%, 22.3% and 8.5%, respectively. However, 77.6% of patients have single, 17.4% double and only 3.4% have triple epicardial territory intervention during each PCI procedure. The mean number of lesions treated per PCI is 1.4 and mean number of vessels 1.26.
The distribution of treated territories in 2015 for stable clinical syndromes was the left anterior descending in 43%, right coronary artery in 28.4%, circumflex in 21.3%, a graft in 2.3% and the left main stem in 5.1%. In patients treated by primary PCI, the circumflex was the culprit in only 16% (compared with 39% for right and 40% left anterior descending), which is in keeping with evidence that acutely occluded circumflex vessels often do not cause typical ST-elevation.
As is shown in Table 2, about 92% of all procedures used stents, of which 88.5% were drug-eluting, though this varied among countries, from 85% in Scotland, to 92% in Northern Ireland. On average, 1.51 stents are used per case. In spite of an increase in the use of drug-eluting stents from 55% to 88.5% between 2007 and 2015, procedures performed for restenosis have remained very stable at about 5%. Use of bioabsorbable scaffolds is rising but these devices are still only used in a minority of procedures (860 in 2015).
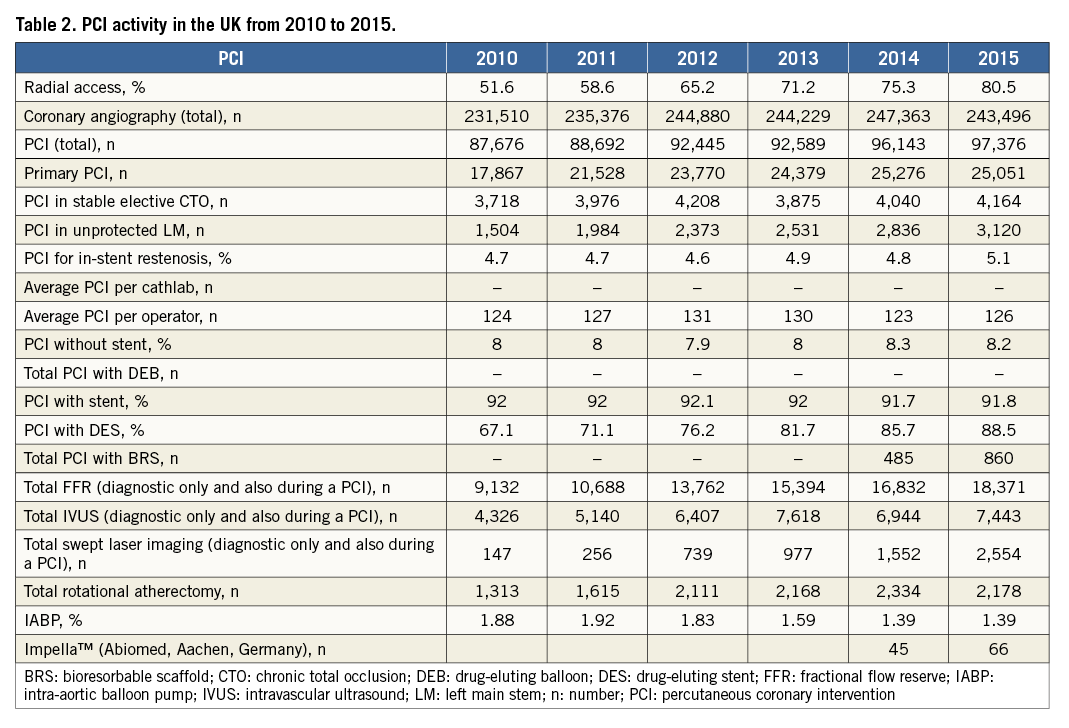
The use of glycoprotein IIb/IIIa receptor antagonists has fallen to 15.3% for all PCIs, 9.9% for NSTEMI and 39.6% for primary PCI. Bivalirudin use in primary PCI fell from its peak of 19% in 2013 to 1.8% in 2015. Ticagrelor use has risen progressively, and in 2015 was used in 29.9% of NSTEMI and 38.1% of primary PCI procedures.
There is quite a marked variation in the use of adjunctive technologies by different centres. For example, although Table 2 shows that rotational atherectomy was used on average in 2.2% of cases, it was as high as 7% in some centres.
PROCESS
Door- and call-to-device times are assessed for patients being treated by primary PCI, and data presented both by median delays and percentage treatment within cut-off recommendations. In 2015, median door-to-device times were 39 minutes, and the percentage of patients treated with a PCI centre door-to-device time less than 90 minutes was 90.5%, and less than 60 minutes 77.8%. These figures are testament to the hard work and dedication of all involved with treating these patients, but continued careful monitoring will remain in place to help ensure delays remain short.
Treatment delays for patients presenting with NSTEMI are less favourable. This might reflect pressure on the system created by the adoption of primary PCI. The median delay to PCI was 59.6 hours in those presenting to a PCI centre, and 80.1 hours for those admitted to a non-PCI centre and then transferred. This meant that, overall, only 56.6% of patients were treated within guideline recommendations of 72 hours.
OUTCOMES
Mortality following PCI is assessed both from data reported by centres, and, for England and Wales, from the independent mortality tracking provided via the Office of National Statistics. Data for 2014 are available at the present time. For patients being treated electively, in-hospital mortality was 0.16%, rising to 0.39% at 30 days (tracked). The in-hospital cerebrovascular accident (CVA) rate was reported as 0.04%. For those treated in the context of NSTEMI, in-hospital mortality was reported as 0.7%, rising to a tracked 30-day mortality of 1.4%. In-hospital stroke was reported at 0.06%. In all patients treated by primary PCI (including those with out-of-hospital arrest, and those in shock), in-hospital mortality was reported as 5.3%, rising to 6.9% by tracking at 30 days. CVA was reported in 0.15% of these cases. For patients in cardiogenic shock, in-hospital mortality was reported as 25.4%, rising to a tracked 30-day mortality of 42%, and in-hospital CVA rate of 0.3%.
PUBLIC REPORTING OF INDIVIDUAL PCI OPERATOR ACTIVITY AND OUTCOMES
Since 2013, individual PCI consultant operator data have been publicly reported in the UK. These reports are available on the patient area of the BCIS web site (www.bcis.org.uk), and are mirrored on the government’s web site “my NHS”. They describe several aspects of each interventional cardiologist’s activity over the previous three years. These include overall PCI volume, case mix and radial access rates. In addition, each operator’s risk-adjusted outcomes are reported. Two different risk adjustment models are used. For all the UK, the North West Quality Improvement Programme model is used2. This is based on self-reported major adverse cardiac and cerebrovascular outcomes (death, myocardial infarction, stroke and need for emergency cardiac surgery). A disadvantage of this approach is that centres that are not good at recording such events will appear to perform better than those who are assiduous at data collection. For this reason, we developed a new risk model that was based on ONS-tracked 30-day mortality. This assessment is therefore independent of a centre’s ability to record post-PCI events, but is currently applicable to England and Wales only3. The data are presented as observed survival (or survival free from major adverse cardiovascular or cerebrovascular events), against confidence limits derived from the models (Figure 1A).
Striking the balance between identifying practice that is in need of improvement, and incorrectly criticising acceptable outcomes is difficult, and exacerbated by the multiple comparisons inherent in this sort of analysis. At present, those who fall outside two standard deviations are made aware of the finding but this does not enter the public domain. However, those who fall outside three standard deviations are publicly identified. There are many reasons why an operator’s outcomes may differ from that predicted by models, thus the identification of a “potential” outlier is intended to start a process of enquiry. The commonest reason for potential outlier status is an error in the recording of data, or incorrect risk factor attribution. These and other issues need to be addressed before it is possible to decide if there might be a genuine problem with an operator’s outcomes.
While the aim is to increase transparency to patients, commissioners, healthcare professionals and the public, there are potential disadvantages to public reporting. These issues have been well rehearsed in the literature, particularly from North America. A balance must be struck between transparency and the creation of risk-averse behaviour, which may disadvantage the sickest of our patients. Most deaths associated with PCI occur in spite of the PCI rather than because of it. Well calibrated risk models should take account of the patient’s comorbidity and presenting clinical features, and are, for example, good at adjusting for cardiogenic shock. However, it is recognised that no risk model currently performs well for patients admitted with out-of-hospital cardiac arrest who are ventilated before PCI. To avoid risk-averse behaviour, these patients are excluded from risk-adjusted public reporting in the UK.
Structural heart interventions
In 2008, a UK transcatheter aortic valve implantation (TAVI) steering group was established to encourage a collaborative approach for the introduction of this technology, with representation from the professional societies, the Department of Health, regulators and commissioners. A data set was established and data from every TAVI procedure in the UK are collected by NICOR to be analysed centrally. Reports based on these analyses are fed back to each centre, and also presented annually (available for free download from the BCIS web site www.bcis.org.uk). Details of the UK experience have been published4. The first cases were performed in 2007, and this had risen to over 2,000 cases by 2015 (Table 3). In 2015 the TAVI rate pmp was 30 across the UK, ranging from 22 pmp in Scotland to 51 pmp in Northern Ireland. Complications to discharge have fallen as case mix has changed and technologies improved. While mean age has remained about 81 years, the logistic EuroSCORE of patients treated by TAVI has fallen from about 22 in 2010 to just 18 in 2015. Stroke occurred in 1.9% in 2015, and early mortality has fallen progressively, with tracked 30-day mortality reaching 3.7% in 2014.
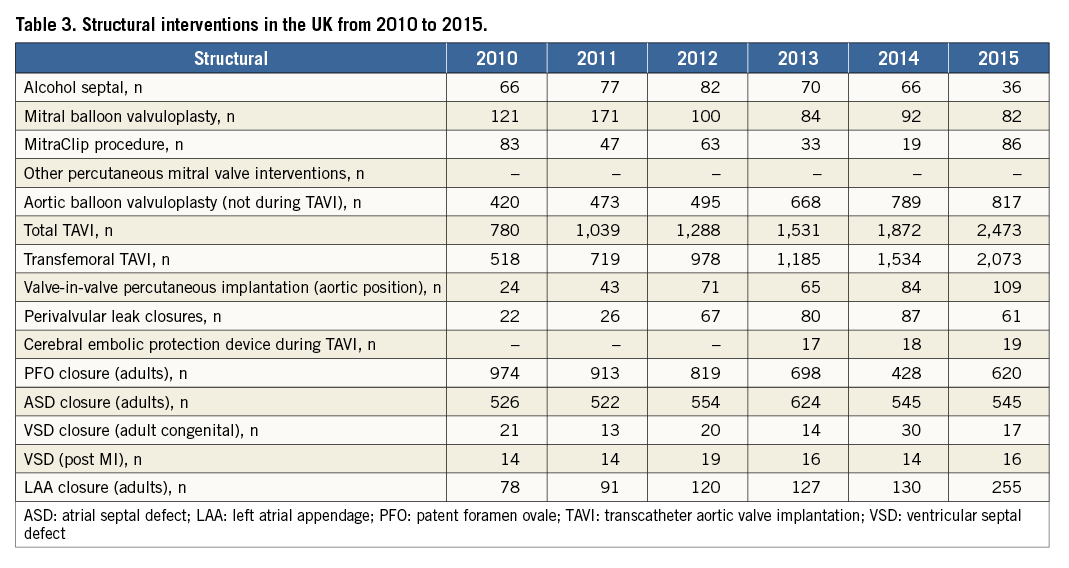
Left atrial appendage occlusion, patent foramen ovale (PFO) closure for stroke, and the use of the MitraClip system for mitral regurgitation have been funded through a process called “commissioning through evaluation”. Centres in the UK were selected to perform a certain number of these procedures, with data being submitted centrally via NICOR. The aim is that these registries will provide information about the application of these technologies in the UK setting and help guide future commissioning.
Conclusions
There is a long tradition of trying to capture interventional activity in the UK which has led to the development of sophisticated data collection mechanisms. These data have provided an important set of benchmarks that have allowed activity across the UK to be explored. The audit process has helped drive up quality of care, particularly with regard to process issues such as the speed with which primary PCI can be delivered. Public reporting has increased transparency, opening up the data to a wider audience, particularly our patients. A large number of observational studies have been published based on the registry data. These have explored a wide variety of clinical issues relating to PCI and TAVI. Many challenges remain. We strive to increase data completeness and quality, and are providing centres with increasingly sophisticated tools to help with data collection. We are in the process of implementing a new information technology infrastructure to collect the national data, and are also developing interactive data visualisation tools to make the analyses and reports more accessible and so better suited to our different audiences, including healthcare professionals, commissioners, regulators and patients.
Acknowledgements
The authors wish to thank the staff at all the hospitals in the UK who provided data for national audit, and the staff at the National Institute for Cardiovascular Outcomes Research for their role in data collection and analysis.
Conflict of interest statement
A. Banning is partially funded by The NIHR Oxford Biomedical Research Unit. The other authors have no conflicts of interest to declare.

