According to current guidelines, primary percutaneous coronary intervention (PPCI) is the preferred form of reperfusion treatment for patients with ST-segment elevation myocardial infarction (STEMI). This article focuses on technical aspects of PPCI and current recommendations for the use of antithrombotic and antiplatelet agents during interventional treatment of STEMI.
Interventional STEMI treatment should be provided by experienced institutions offering 24 hours / 7-day PPCI service with acceptable transport delay. Patients referred from community non-PPCI hospitals as well as from ambulances should be accepted for mechanical reperfusion. As the clinical outcome after interventional treatment closely depends both on the experience of the operators and the PCI laboratory as a whole. The current guidelines unequivocally recommend that PPCI should be performed by skilled professionals within less than 90-120 minutes after first medical contact. Optimally, hub-spokes system based on PPCI-hospital and collaborating remote hospitals or ambulances referring STEMI patients should be established. Also, standard operating procedures for STEMI treatment for PCI-hospitals should be implemented. Comprehensive quality improvement program and monitoring of clinical outcomes and door-to-balloon times for PPCI-hospitals and STEMI treatment network as a whole should be obligatory.
Administration of aspirin, unfractionated heparin and clopidogrel before transfer to PPCI is strongly recommended. Thereby, broader use of bivalirudin, as an alternative to the combination of unfractionated heparin and GPIIb/IIIa inhibitors, especially in patients with increased risk of bleeding, is recommended. It is also advisable to adjust treatment to the individual patient’s specific needs (type of pharmacotherapy, transport for PPCI versus fibrinolysis) based on the risk of infarction (duration of symptoms at presentation, infarct location, signs of heart failure), risk of bleeding (age) and a possibility of transport for PPCI (expected delay). Preferably the technique of direct stenting, with a broader use of drug-eluting stents during PPCI should be employed if possible. Use of simple manual aspiration in occluded arteries, as well as vessels with established flow and large thrombus burden, should be recommended. Aspiration should be started 2 cm before lesion with thrombus. Multiple slow-passage techniques should be used, with a stop on the thrombus site and continuation of suction distally to the site of occlusion (if possible). Two or three passages are recommended. Optimally, suction success should be confirmed by presence of thrombus on the filter. If passage with catheter through the lesion site is not possible, a low-pressure small balloon inflation is allowed to give a possibility of passing to the distal segments. Optimal technique of PPCI should be chosen after evaluation of IRA flow, thrombus burden and vessel size (Figure 1).
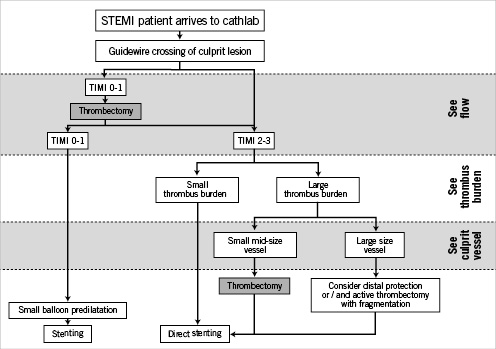
Figure 1. Flow chart for primary percutaneous coronary intervention in ST-segment elevation myocardial infarction. Modified with permission from Dudek D, Mielecki W. Tips & tricks of thrombectomy devices. In: Sabate M. Percutaneous cardiac interventions. Tips and tricks of new techniques beyond stenting. PCR publishing 2010.

