“Reports that say that something hasn’t happened are always interesting to me, because, as we know, there are known knowns; there are things we know we know. We also know there are known unknowns; that is to say we know there are some things we do not know. But there are also unknown unknowns - the ones we don’t know we don’t know. And if one looks throughout the history of our country and other free countries, it is the latter category that tend to be the difficult ones.” United States Secretary of Defense. Donald H. Rumsfeld 20021.
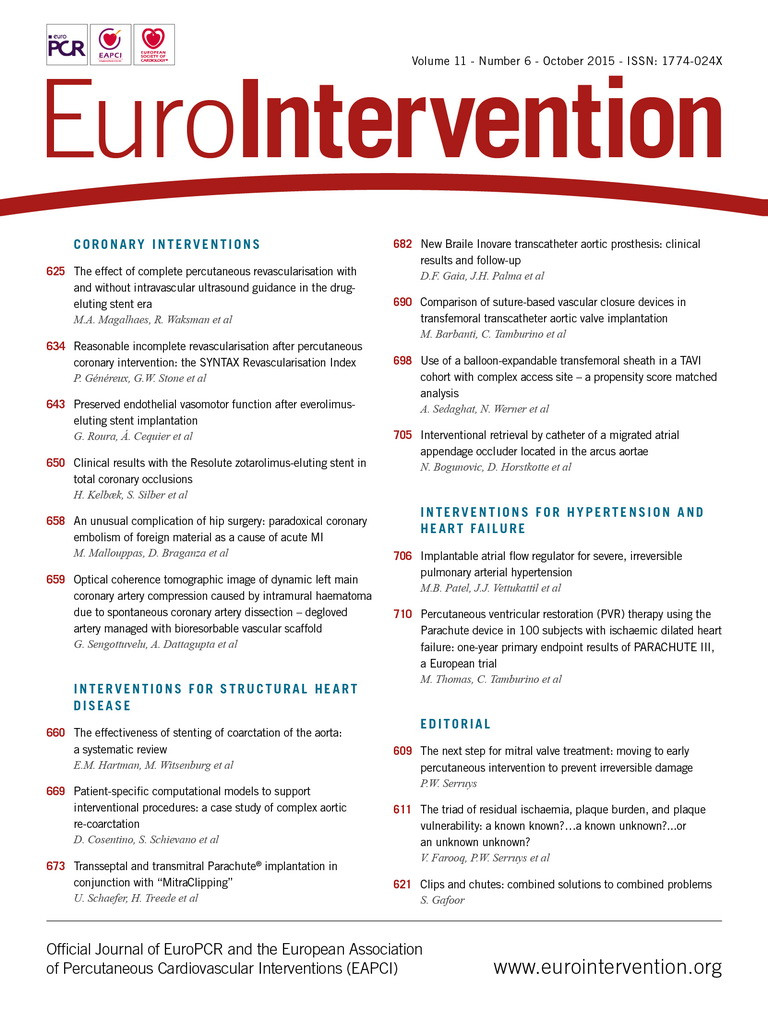
Donald Rumsfeld famously gave the above answer to a question about the lack of evidence linking the then government of Iraq to weapons of mass destruction. When trying to understand the role of ischaemia and completeness of revascularisation in stable coronary artery disease, one is faced with a similar conundrum. Central to this question is the role of ischaemia and the impact of surgically and percutaneously based revascularisation on clinical outcomes in stable coronary artery disease. Historically, both COURAGE2 (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) and BARI 2D3 (Bypass Angioplasty Revascularization Investigation 2 Diabetes), examining predominantly mild to moderate ischaemia, have failed to show a survival benefit for revascularisation, whereas the SYNTAX trial4-6, examining much more complex patients with a greater anatomically complex disease and ischaemia burden, demonstrated a clear survival benefit for complete revascularisation in all-comers PCI and CABG-treated populations (Figure 1, Figure 2)7,8.
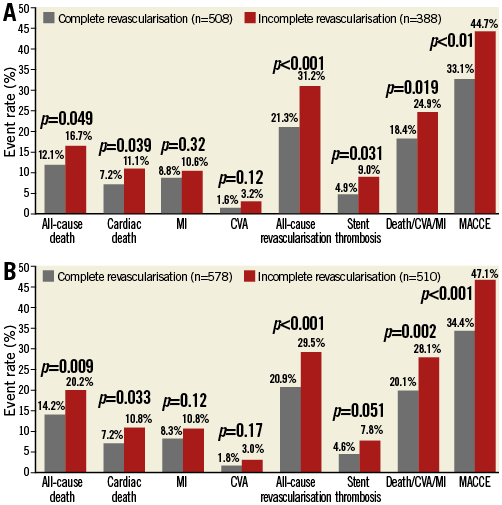
Figure 1. Long-term (five-year) clinical outcomes in the PCI arm of the SYNTAX trial stratified by completeness of revascularisation. A) Randomised SYNTAX PCI cohort. B) All-comers (randomised and registry) SYNTAX PCI cohort. CVA: cerebrovascular accident; MACCE: major adverse cardiac and cerebrovascular events; MI: myocardial infarction. Courtesy of the SYNTAX Trial Investigators4-6.
Figure 2. Long-term (five-year) clinical outcomes in the CABG arm of the SYNTAX trial stratified by completeness of revascularisation. A) Randomised SYNTAX CABG cohort. B) All-comers (randomised and registry) SYNTAX CABG cohort. CVA: cerebrovascular accident; MACCE: major adverse cardiac and cerebrovascular events; MI: myocardial infarction. Courtesy of the SYNTAX Trial Investigators4-6.
SYNTAX trial
Notably, in the SYNTAX trial, the negative impact of incomplete revascularisation on clinical outcomes, including mortality, was evident in the randomised and all-comers (randomised and registry) PCI cohorts (Figure 1), whereas, with CABG, clinical outcomes were shown to be dependent on the study population examined (Figure 2)7,8, i.e., there was little difference in clinical outcomes, including mortality, between complete and incomplete revascularisation in the randomised CABG cohort (Figure 2A), compared to a clear mortality benefit in the all-comers CABG cohort (Figure 2B). Trying to understand these findings at first glance appears confusing, until one examines the types of patients enrolled in the randomised and all-comers cohorts of SYNTAX.
SYNTAX was designed to be an all-comers trial, in which practically no patient was refused entry, in order to overcome the selection bias that had plagued earlier randomised trials comparing surgically and percutaneously based revascularisation9,10. For a patient to be randomised in SYNTAX, both the cardiac surgeon and the interventional cardiologist had to agree that the patient could potentially undergo equivalent anatomical revascularisation, and that CABG and PCI could equally be offered4-6,11. Patients were nested in registries if these criteria could not be met. As a result, the CABG registry (for PCI-ineligible patients) had significantly more anatomically complex disease compared to the randomised CABG cohort (mean SYNTAX score 37.8±13.3 vs. 29.1±11.4, p≤0.001) since the interventional cardiologist was unable to match the cardiac surgeon in offering complete revascularisation. In addition, the CABG registry had greater vascular-related clinical comorbidity (presence of peripheral vascular disease, carotid artery disease, clinical urgency, and reduced ejection fraction), undoubtedly due to the association of increasing coronary anatomical complexity with extra-cardiac vascular disease12. Conversely, the PCI registry (for CABG-ineligible patients) had profoundly greater clinical comorbidity, since CABG was prohibitive on the grounds of operative risk (greater EuroSCORE and Parsonnet scores)13,14.
Reasonable incomplete revascularisation
To add to this already complex picture is the concept of reasonable incomplete revascularisation in surgically and PCI-treated patients15-19, namely that when a threshold of coronary artery disease (and associated ischaemia) is treated, the residual ischaemia is limited and does not have an adverse impact on clinical outcomes. This concept has been shown to potentially exist in both CABG and PCI-treated patients in SYNTAX17-19. Such findings have support from the nuclear substudy of the COURAGE trial20, which associated at least moderate (≥10%) ischaemia with an adverse prognostic impact, and is now the subject of the ongoing multicentre randomised ISCHEMIA trial (ClinicalTrials.gov Identifier: NCT01471522), aiming to recruit ~8,000 patients worldwide. ISCHEMIA uses at least a moderate amount of ischaemia as an entry criterion and will compare an initial invasive strategy of cardiac catheterisation followed by optimal revascularisation in addition to optimal medical therapy (OMT), compared to an initial conservative strategy of OMT alone with catheterisation reserved for failure of OMT. The primary endpoint will be time to centrally adjudicated cardiovascular death or non-fatal myocardial infarction over an average follow-up of four years.
With regard to less complex coronary artery disease, this is currently the subject of the ongoing PROSPECT II and PROSPECT ABSORB trials (ClinicalTrials.gov Identifier: NCT02171065) which aim to identify plaques prone to future rupture and clinical events, and potentially to passivate them with the Absorb bioresorbable vascular scaffold (BVS)21-23, in addition to guideline-directed OMT.
Does ischaemia per se lead to adverse hard clinical outcomes?
Against this backdrop, let us now ask the question, does ischaemia per se lead to adverse hard clinical outcomes? Ignoring the potential for improving functional capacity, etc., the answer is probably no, provided one can guarantee that the patient will never have a future cardiac event (a highly implausible scenario). To rephrase the question –do anatomic burden and plaque vulnerability lead to adverse outcomes, and does associated ischaemia (and potential revascularisation) in this setting have an impact on clinical outcomes? The answer is probably yes. A recent post hoc analysis of COURAGE24 demonstrated that the anatomic burden of coronary disease –crudely quantified by a numerical score assessing the number of stenotic lesions as a marker of the extent of myocardial jeopardy– was potentially a more potent predictor of adverse clinical outcomes compared to the actual degree of ischaemia. In the accompanying editorial25, Spencer King 3rd used the following analogy to help explain these findings:
“One can imagine that a patient with a total occlusion of an anterior descending coronary artery and collateral supply from other vessels would have a large ischaemic burden, but if there is not extensive atherosclerosis in the other vessels, the potential for an acute coronary event may be limited. Conversely, a patient with an extensive anatomic burden of disease may have many plaques that are potentially vulnerable to producing an acute event. In other words, the presence of ischaemia is not what produces most clinical events but rather the vulnerable plaque that leads to a sudden occlusion or embolisation of a previously functioning conduit. One might ask in retort why ischaemia has always been viewed as a risk factor for clinical events. Patients with increasing degrees of ischaemia are likely to also have increasing burden of anatomic disease, but in this current observation on patients having both parameters measured, the anatomic disease trumps the measure of chronic ischaemia.”
This simple analogy highlights the potential importance of revascularising total occlusions in appropriately selected patients, and is supported by many registries showing the presence of multivessel disease in STEMI to have an adverse short- and long-term prognostic impact compared to single-vessel disease26,27, in particular when cardiogenic shock is present –with the presence of a concurrent non-infarct-related chronic total occlusion (that is well collateralised from the culprit vessel), a key factor driving the poorer survival.
SYNTAX score II
The issue of plaque burden and vulnerability potentially influencing outcomes has support from the SYNTAX score II28-30, where the anatomical SYNTAX score was combined with clinical variables that were shown to alter the threshold value of the anatomical SYNTAX score that would lead to similar long-term mortality between CABG and PCI. Notably, female gender, reduced left ventricular ejection fraction and impaired kidney function were shown to be factors that affected decision making between CABG and PCI despite correction for all risk factors, with much lower anatomical SYNTAX scores needed for equipoise for long-term mortality between CABG and PCI28. These findings are supported by a recent sub-analysis of the STICH (Surgical Treatment of IsChemic Heart failure) trial31, demonstrating that, in subjects with more advanced ischaemic cardiomyopathy, more extensive coronary artery disease and worse myocardial dysfunction and remodelling, a net longer-term prognostic benefit was seen for CABG compared to OMT, despite the short-term (30-day) mortality risk being higher with CABG. In addition, a population-based study of patients with chronic kidney disease and multivessel coronary disease from the Ontario provincial registry demonstrated that CABG was associated with improved early and late mortality benefit compared to PCI32. These findings raise the possibility that excess plaque vulnerability, in addition to plaque burden, may play a role in decision making between CABG and PCI, in that patients with these characteristics are more likely to derive a longer-term prognostic benefit from surgical revascularisation, despite the potentially higher operative risks associated with reduced left ventricular ejection fraction or impaired kidney function. These findings may in part be due to the potentially protective effects of a bypass graft in passivating the entire vessel from future cardiac events for the lifespan of the graft –unlike PCI which would treat the obstructive lesion alone9,28,31,32.
Washington registry
Adding to this increasingly complex field, in this issue of EuroIntervention, comes an important registry study from Magalhaes and colleagues33 from the Washington Hospital Center, USA, describing the impact of intravascular ultrasound (IVUS) guidance in attaining complete revascularisation. Based on a definition of all epicardial and significant branches ≥2.5 mm in vessel diameter successfully treated in patients with multivessel disease n=2,132 consecutive patients with 4,299 lesions), complete revascularisation not unexpectedly was shown to be associated with a lower incidence of death/Q-wave myocardial infarction at one year compared to incomplete revascularisation, an effect that persisted after adjustment for confounding factors (HR: 0.66 [0.38-0.99], p=0.046). Notably, IVUS guidance was shown to allow more complete revascularisation by optimising stent implantation and lesion coverage, allow the detection of coronary lesions not appreciated as warranting revascularisation by angiography alone, and was shown to reduce the incidence of repeat intervention irrespective of whether or not complete revascularisation was achieved. Such findings support meta-analyses demonstrating the potential benefit of IVUS-guided PCI34,35, and increase expectations from the ongoing SYNTAX II trial36 (ClinicalTrials.gov Identifier: NCT02015832) which uses functional and IVUS guidance in revascularising patients with multivessel (de novo three-vessel) coronary artery disease.
When interpreting the results of the Washington registry, one should however be mindful of the population studied and whether this is representative of contemporary practice. One glaring issue in the Washington registry is the complete exclusion from the study of patients with chronic total occlusions, with the authors stating that it was the preferred strategy for these patients to undergo surgical revascularisation. The lack of revascularisation of CTOs was the most common cause of incomplete revascularisation in SYNTAX8, yet in the Washington study, since the presence of CTOs was an exclusion criterion, complete revascularisation was still not attainable in the majority of patients (866/2,132, 41%), this in spite of a less strict definition of complete revascularisation (vessels >2.5 mm) compared to SYNTAX (>1.5 mm). There is undoubtedly a strong likelihood that there is a (probably appropriate) selection bias in patients who were incompletely revascularised, with a significant subset of patients with very complex disease in which complete revascularisation was not possible, was not the operator’s intention, or, importantly, who were surgical turndowns. The issue of surgical turndown patients not being recorded as such in registries is not a small one, having recently been shown to occur relatively commonly in registries (in 22% of subjects at two academic medical centres in the USA37) and to be a strong independent predictor of in-hospital and long-term mortality following PCI37. These data are supported by the PCI registry of SYNTAX, consisting of patients with clinical comorbidity that made surgical revascularisation prohibitive, in which the five-year mortality was as high as 30%6.
One other interesting observation from the Washington registry was the cluster of stent thrombosis seen in patients who were incompletely revascularised following PCI. These findings were also shown in the PCI-treated patients from SYNTAX8 (Figure 1). Notably, in the Washington registry, as alluded to by the authors, because of a higher use of IVUS guidance and a similar post-diameter stenosis in complete and incomplete revascularisation patients, this would make stent optimisation a less likely cause for the increase in stent thrombosis in patients who were incompletely revascularised. As referred to below, incomplete revascularisation is a surrogate marker of sicker patients8,38 with more vascular-related comorbidity, which raises the possibility that this phenomenon, if real, may be secondary to neoatherosclerosis, as has previously been hypothesised in the SYNTAX trial8,39,40. In support of this hypothesis are recent data from the long-term follow-up of patients implanted with first-generation drug-eluting stents from the SIRTAX trial, which demonstrated in-stent neoatherosclerosis to be more common among patients with angiographic and clinical evidence of native atherosclerosis progression, suggesting a similar underlying pathophysiological mechanism40.
Surrogate marker of sicker patients
Putting all this together, it is clear that incomplete revascularisation is a surrogate marker of sicker patients with more anatomically complex disease and more vascular-related clinical comorbidity, and that this has an adverse impact on longer-term outcomes, including mortality8,38. Comparisons between the complete and incomplete revascularisation groups have been likened to comparing apples and oranges, and, whilst statistical matching of patients may help, the likelihood of unaccounted confounders should lead us to interpret these results with caution8,38,41.
What is clear is that treating the ischaemia in patients with complex coronary artery disease affects outcomes, but plaque burden and vulnerability are factors which, at present, we do not reliably know how to integrate into current decision-making processes. Clinical tools such as the anatomical SYNTAX score and SYNTAX score II are likely to account indirectly for this phenomenon, whereas the use of intravascular imaging to aid in potentially passivating high-risk plaques remains the subject of ongoing research. There is, however, a need to differentiate between complete and reasonably incomplete revascularisation that would not have an adverse impact on clinical outcomes in surgically and percutaneously treated patients. The judgement of the Heart Team and clinical tools15-19 to objectively quantify reasonable incomplete revascularisation will potentially aid this process. This phenomenon may however not be static or even be completely predictable since it is dependent on the degree of plaque burden and vulnerability which we do not yet know how to reliably measure and integrate into our decision-making algorithms for treating ischaemia. Trying to adopt a one size fits all treatment strategy therefore appears difficult, but the logic of trying to attain as complete a revascularisation as possible in patients with multivessel disease, which would include revascularisation of total occlusions if the territory is viable, does not appear unreasonable, or at least staying within the threshold of reasonably incomplete revascularisation, however one is to judge this. One should not, however, underestimate the vital role of guideline-directed OMT in reducing coronary artery disease progression and clinical events42,43. This guidance is supported by the BARI trial, which demonstrated that two thirds of the increase in myocardial jeopardy and recurrence of angina at five years is related to native coronary disease progression in previously untreated coronary vessels44.
The future
Future studies targeting all three factors, namely anatomical complexity/residual ischaemia, plaque burden, and plaque vulnerability seem more appropriate, and are probably more likely to be achievable with non-invasive imaging utilising computed tomography (CT) angiography, non-invasive anatomical assessments (with, for example, a CT-derived SYNTAX score36,45) and possibly molecular imaging to assess plaque vulnerability non-invasively46,47. These are the known unknowns. There are, however, likely to be unknown unknowns which we are yet to consider. The German sociologists Daase and Kessler, whilst agreeing with the basic points of Rumsfeld, have argued that he left out a vital point, namely “what we do not like to know”48, in this case whether looking at ischaemia and the impact of complete revascularisation in isolation is a gross oversimplification of what is actually going on, and how it impacts on the treatment of our patients…
Conflict of interest statement
The authors have no conflicts of interest to declare.