Abstract
Aims: To assess outcomes after transcatheter aortic valve implantation (TAVI) according to sex, with the two available valves and four recognised delivery approaches.
Methods and results: VARC outcomes are reported according to sex for 305 high-risk patients consecutively treated in our centre, via available access routes utilising the Edwards SAPIEN™/SAPIEN™ XT or the Medtronic CoreValve ReValving System® devices. Three hundred and five patients underwent TAVI: 52.1% male and 47.9% female. Females had a smaller body surface area (1.84±0.16 m2 vs. 1.70±0.16 m2; p<0.001) and aortic annulus (24.4±1.6 mm vs. 22.6±1.7 mm; p<0.001) with increased symptoms (NYHA Class III/IV 61.6% vs. 73.6%; p=0.026). Conversely, men had more comorbidities: diabetes mellitus (35.2% vs. 21.9%; p=0.010), chronic kidney disease (41.8% vs. 23.3%; p=0.001), chronic obstructive pulmonary disease (45.3% vs. 30.1%; p=0.006) and previous myocardial infarction (28.3% vs. 14.4%; p=0.003). Thirty-day mortality was 4.7% with no difference between groups. There was a trend for females to develop more major vascular complications (11.9% vs. 19.9%; p=0.058). Notably, females required more blood transfusion (38.4% vs. 50.0%; p=0.041). No differences were observed in device success (92.5%; p=0.667), combined safety endpoint (61.8%; p=0.211) or combined efficacy endpoint (72.0%; p=0.889).
Conclusions: Female sex was a predictor of major vascular complications with females requiring more transfusion. No differences were noted amongst patients undergoing TAVI in composite safety and efficacy endpoints according to sex.
Introduction
Aortic stenosis (AS) is the most frequently encountered valvular heart disease and the consensus is intervention should be offered.1, 2 As the incidence increases with age, patients with significant AS are seen more commonly, with more associated comorbidities.Transcatheter aortic valve implantation (TAVI) has been demonstrated as an alternative treatment for severe AS in patients at high risk for current surgical techniques.3
Female patients with symptomatic AS tend to be older, with more associated conditions. Despite this, it has been shown that female sex is an independent predictor of survival in patients over 79 years undergoing SAVR.4 Furthermore, multivariable analysis has shown female sex is independently associated with better recovery of the left ventricular systolic function following TAVI5 and that left ventricular hypertrophy reverses more frequently in this group following SAVR.6 Female patients may therefore be more suited to undergo TAVI in view of their comorbidities, with more to benefit.
To our knowledge, no data has currently been published analysing possible gender issues regarding TAVI in clinical practice. The objective of this single-centre registry study was to evaluate the outcomes according to the sex of the patient with a comprehensive TAVI program which uses both currently commercially available transcatheter valves: Edwards SAPIEN™/Edwards SAPIEN™ XT (ESV) (Edwards Lifesciences, Irvine, CA, USA) and Medtronic CoreValve ReValving System® (MCV) (Medtronic, Minneapolis, MN, USA), via the transfemoral (TF), transapical (TAp), transaxillary (TAx) and transaortic (TAo) approaches.
Methods
Patients
From November 2007 to April 2011, all consecutive patients referred to our centre (San Raffaele Scientific Institute, Milan, Italy) for consideration of TAVI were assessed. Initially a multi-disciplinary team review was performed, consisting of two interventional cardiologists, one cardiothoracic surgeon and one anaesthesiologist. The decision that TAVI would be appropriate was made in patients who had severe symptomatic AS with an aortic valve area of <1cm2, in addition to fulfilling one of the following criteria: high surgical risk, as defined by a logistic European System for Cardiac Operative Risk Evaluation (logistic EuroSCORE) ≥10% (which is the current cut off for reimbursement in the Milan region); comorbidities not included in the score, including thoracic radiotherapy, porcelain aorta, Child-Pugh Class B and C liver cirrhosis or previous coronary artery bypass grafting with patent conduits (right internal mammary which crosses under the sternum or left internal mammary which may be damaged with re-do sternotomy access); or marked frailty conferring increased risk for SAVR as determined by the cardiothoracic surgeon.
Following the decision that TAVI was the treatment of choice, aCT scan was performed to assess the aortic annulus dimensions, the peripheral access sites and to delineate the coronary arteries.
The TF approach was considered as the first line access site, unless imaging had suggested this would not be appropriate and according to the discretion of our surgeons other access sites were reviewed (TAx>TAp>TAo). The procedures were performed as previously reported by our group,7 with TF percutaneous access and closure unless a complication arose.
Regarding valve type (ESV versus MCV), the annulus diameter, degree of aortic regurgitation and non TF route chosen (TAx versus TAp) were the criteria (Figure 1).
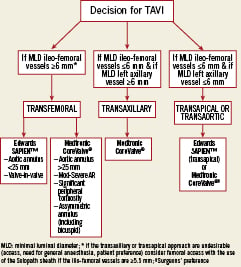
Figure 1. A schematic representation of the current access and device selection for TAVI in our institution.
The data was collected from a comprehensive prospective database with additional review of the patients’ case notes to enable all events to be confirmed. Following the publication of the VARC definitions, the events according to these were adjudicated retrospectively by two interventional cardiologists and a cardiothoracic surgeon independently.
Study endpoints
The endpoints were defined according to the published VARC definitions8. The safety and efficacy study endpoints consisted of all cause and cardiovascular mortality, myocardial infarction (MI), stroke, bleeding (life-threatening, major and minor), acute kidney injury (AKI) (stage 1-3) and vascular complications (major and minor). The prosthetic valve complications were prosthetic AS and regurgitation, prosthetic valve thrombosis and endocarditis (SBE), conduction disturbances and arrhythmia, permanent pacemaker implantation (PPM) and coronary obstruction. Furthermore, the composite endpoints of device success, combined safety endpoint (freedom from all-cause mortality, major stroke, life-threatening bleeding, AKI stage3, MI and major vascular complication at 30days) and combined efficacy endpoint (freedom from all-cause mortality, failure of current AS therapy or prosthetic valve dysfunction at one year) were reported. All patients provided written informed consent for the procedure and data collection according to our hospital practice.
Procedures
Initially in November 2007 the SAPIEN was used, the MCV became available in July 2008 and the SAPIEN XT replaced the SAPIEN in April 2010. Both brands of valve were used TF, TAx and TAo. The ESV was used TAp.
The patients were administered a dose of cefazolin 2g one hour prior to the procedure as antibiotic prophylaxis, and cefazolin 2g daily for five days thereafter. During the procedure, weight-adjusted unfractionated heparin was administered and monitored to maintain the activated clotting time between 200-250 seconds. Following TAVI, dual antiplatelet therapy was recommended for a period of 3-6 months consisting of aspirin 100mg daily, plus clopidogrel 75mg daily or ticlopidine 250mg twice daily. Aspirin was continued indefinitely thereafter.
Statistical analysis
Continuous variables are expressed as mean±SD and analysed with the Student t test or Wilcoxon rank-sum test depending on the variable distribution. The effect of nominal variables is analysed with the chi-squared test or Fisher exact test as appropriate. A regression model was performed to determine the independent predictors of the study endpoints using purposeful selection of covariates. Variables associated at univariate analysis and those judged to be of clinical importance from previous published literature were eligible for inclusion into the multivariable model-building process. Survival was recorded by Kaplan-Meier analysis and the log-rank method was used for comparison. All statistical analysis was performed with SPSS version 18.0 (SPSS Inc, Chicago, Il, USA). Ap-value of <0.05 was considered statistically significant.
Results
Between November 2007 and April 2011, 468 patients with a diagnosis of severe symptomatic AS were screened by our centre for possible TAVI. 305 (65.2%) of these underwent TAVI and were included in this analysis. Of the remainder: 113 (24.1%) were treated medically, 24 (5.1%) underwent SAVR, 18 (3.8%) had balloon valvuloplasty and eight (1.7%) died awaiting treatment. The median clinical follow-up length of those individuals undergoing TAVI was 279 (IQR 51-485) days.
The baseline characteristics of the study population according to sex are illustrated in Table1. In total, 52.1% were male and 47.9% were female. Females presented with more severe symptoms (NYHA Class III/IV 61.6% vs. 73.6%; p=0.026) and were more likely to undergo ESV implantation (55.3% vs. 66.4%; p=0.048). Furthermore, females had a smaller body surface area (1.84±0.16m2 vs. 1.70±0.16m2; p<0.001) and aortic annulus (24.4±1.6 mm vs. 22.6±1.7 mm; p<0.001). Notably, there was no difference between groups in the ileo-femoral size (9.8±3.6 vs. 8.9±1.4; p=0.505). Male patients were more likely to have diabetes mellitus (35.2% vs. 21.9%; p=0.010), chronic kidney disease (41.8% vs. 23.3%; p=0.001), chronic obstructive airways disease (45.3% vs. 30.1%; p=0.006) and previous myocardial infarction (28.3% vs. 14.4%; p=0.003) or CABG (28.3% vs. 13.0%; p=0.001). There was no difference in the access site chosen.
Safety and efficacy endpoints
The VARC safety and efficacy outcomes are reported in Table2. No significant difference was observed in death between males and females (respectively 3.8% vs. 5.6%; p=0.475) or cardiovascular death (3.2% vs. 4.2%; p=0.649) at 30 days. In the female group, there were eight deaths during the index hospitalisation, with no additional deaths between discharge and 30 days. Four deaths were due to aortic rupture/dissection, two of arrhythmia, one multi-organ failure and the last of a retroperitoneal bleed. Amongst the male group, there were six deaths. Two patients died of multi-organ failure, one patient of severe right heart failure, one of an interventricular septum rupture, one of refractory cardiogenic shock and finally one of a sudden death. Body mass index (odds ratio=OR 0.770; 95% CI 0.644-0.922; p=0.005), Logistic EuroSCORE (OR 1.034; 95% CI 1.004-1.006; p=0.029) and the presence of persisting significant aortic regurgitation (OR 8.242; 95% CI 1.306-52.029; p=0.025) were all correlated to overall mortality at 30 days. Multivariable analysis revealed no difference in the predictors of death according to gender.
There were four (1.3%) recorded periprocedural myocardial infarctions; one spontaneous event occurred in a male patient. The three females experiencing MI (all periprocedural) had an elevation of CK-MB enzymes and echocardiographic abnormalities or ventricular arrhythmia without any ST changes on EKG and/or symptoms diagnosing myocardial infarction. There were only three (1.0%) major strokes which affected two males and one female.
No significant differences in bleeding complications according to the VARC definitions were observed in our analysis. Life-threatening bleeding occurred in 36 (22.6%) males and 43 (29.5%) females. Amongst the female patients experiencing this complication, 15 (34.9%) developed shock, 11 (25.6%) were transfused ≥4units of blood and 10 (23.3%) had a drop in haemoglobin of ≥5g/dL. Furthermore, seven (16.3%) were complicated by cardiac tamponade. Of males having this complication, 11 (30.6%) required a blood transfusion ≥4 units, 11 (30.6%) had a reduction in haemoglobin ≥5g/dL, 10 (27.8%) had shock and finally, 4 (11.1%) had cardiac tamponade. The majority (94.9%) of life-threatening bleeding was procedure related, including cardiac tamponade and vascular access problems, with the remainder consisting of 2.5% haemothorax, 1.3% haematuria and 1.3% permanent pacemaker haematoma. There were 3 (1.0%) of patients in total who were converted to surgery, one female as the consequence of aortic annulus rupture and 2 (one of them a female) for uncontrolled bleeding. Predictors of life-threatening bleeding overall were the logistic EuroSCORE (OR 1.023; 95% CI 1.008-1.039; p=0.004) and all AKI (OR 3.145; 95% CI 1.788-5.533; p<0.001).
However, despite no significant difference in baseline haemoglobin (12.3±1.9g/dL vs. 12.0±1.6g/dL; p=0.125) or reduction in haemoglobin (2.7±1.6g/dL vs. 2.8±1.5g/dL; p=0.633), the female group was significantly more likely to undergo blood transfusion (38.4% vs. 50.0%; p=0.041). However, when receiving a blood transfusion, the median number of units was three (interquartile range 2-4 units) in both males and females. Furthermore, analysis showed that although the dose of heparin received during the procedure was similar between males and females (respectively 5284±1283 IU vs. 5145±1507 IU; p=0.504), when adjusted for the weight of the patient there was a trend towards a higher dosage of heparin per kilogram of body weight administered to the female group (72.9±19.4 IU vs. 78.6±22.1 IU; p=0.072).
There were 15.7% major vascular complications overall, with a trend towards an increased incidence amongst the female group (11.9% vs. 19.9%; p=0.058). Of the 29 females who had this complication: 18 (62.1%) required access site intervention, four (13.8%) pseudoaneurysms required intervention, three (10.3%) haematomas required ≥4 units of blood, 2 (6.9%) Prostar failures required ≥4units blood and finally two (6.9%) had aortic dissection/rupture. Amongst the 19 male patients who had this complication, there were 11 (57.9%) access site complications, five (26.3%) pseudoaneursyms, two (10.5%) failures of Prostar requiring ≥4 units of blood and one (5.6%) aortic dissection. Of note, it emerged that female gender was an independent predictor of major vascular complications (OR 0.970; 95% CI 0.947-0.993; p=0.012) in addition to the preprocedural ejection fraction (OR 0.512; 95% CI 0.264-0.994; p=0.048).
There was no difference in the occurrence of AKI stage 3 between the sexes (10.1% vs. 10.3%; p=0.951), with logistic EuroSCORE (OR 1.028; 95% CI 1.008-1.048; p=0.005) and life-threatening bleeding (OR 3.916; 95% CI 1.757-8.728; p=0.001) predictors of AKI stage 3.
Prosthetic valve performance and associated complications
There were no significant findings in prosthetic valve performance between genders. Following TAVI, there was no observed difference between sexes in the occurrence of aortic regurgitation; neither in those with more than a mild degree (defined as ≥2+) (respectively 28.9% vs. 24.0%; p=0.327) nor in those with a marked degree of valvular incompetence (3/4+) (4.4% vs. 4.1%; p=0.899). Furthermore, there was no difference in the incidence of PPM (16.4% vs. 13.0%; p=0.411), with an overall rate of 14.8%. (Table3)
Composite endpoints
Interestingly, female patients did have a trend to longer in-hospital stay during the index procedure as compared to males (7.4±5.7 days vs. 9.3±12.4 days; p=0.082). Device success occurred in 93.1% of male patients and 91.8% of females (p=0.667). Of the 11 device failures in the male group, seven had residual significant aortic regurgitation, two required the implantation of a second valve for residual severe AR and the last two had a second valve implantation because of embolisation of the first valve. In the female group, among 12 who had device failure: six had residual significant aortic regurgitation, four required a second valve (two due to severe aortic regurgitation, one for valve embolisation, another for aortic annulus rupture), another had a low implantation of an ESV and the last had failure of the valve to traverse the subclavian requiring conversion to a TF approach. The composite safety endpoint at 30 days was reached in 65.2% of males and 58.2% of females (p=0.211). Logistic EuroSCORE (OR 0.980; 95% CI 0.965-0.995; p=0.010) and baseline renal insufficiency (OR 0.507; 95% CI 0.296-0.869; p=0.134) were shown to be correlated with the combined safety endpoint. Furthermore, 164 patients were eligible for follow-up of one year, giving a combined efficacy endpoint of 72.0% overall, with again no significant difference between genders (p=0.889). (Table 4) Figure2 demonstrates survival at one year according to the sex of the patient by Kaplan-Meier analysis. Predictors of one year mortality were body mass index (OR 0.824; 95% CI 0.691-0.983; p=0.032), preprocedural ejection fraction (OR 0.953; 95% CI 0.911-0.997; p=0.038) and acute kidney injury stage 3 (OR 4.149; 95% CI 1.144-15.047; p=0.030). No differences emerged between the sexes.
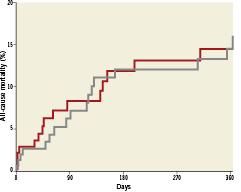
Figure 2. Kaplan-Meier curves to illustrate one year all-cause mortality according to the sex of the patient (males represented by gray line and females by red line).
Discussion
The main findings of the sub-analysis according to sex in our single-centre registry are: 1) female patients tend to be more symptomatic for NYHA at time of presentation with severe AS, however they have fewer comorbidities compared with men; 2) no differences in mortality, MI or stroke were observed between men and women at 30 days; 3) female patients were more likely to have major vascular complications and female sex was a predictor of this complication and 4) females consequently undergo more blood transfusions than their male counterparts.
To our knowledge, this is the first analysis to investigate whether there are differences in outcomes according to the sex of the patient following TAVI.
Notably, the proportion of females included in TAVI series is higher compared to coronary artery trials where females were significantly under-represented.9 One possible explanation is AS is a disease of the elderly and females tend to survive longer. Other possible causes are the lower BSA in the females, which is known to be associated with lower survival10 could have influenced the therapeutic decision and led to TAVI as well as delayed time to diagnosis. It has been postulated that the left ventricle of women adapt differently to AS, developing more hypertrophy with normal LVEF, which could have influenced the time of the diagnosis.11
In our study there was no difference in access site chosen between sexes, which may appear surprising, as females were smaller. However, there was no difference in the femoral access size between genders.
As expected, the aortic annulus size of our patients was significantly smaller, with more ESV utilised. Overall, there were four aortic dissection/ruptures in females versus one amongst males. Potentially the smaller size could be a risk for this and care needs to be taken when deciding the most appropriate valve size.
In our experience, TAVI appeared to be safe with 4.7% all-cause mortality at 30 days, not significantly influenced by gender. Our overall 30 day mortality rate compares favourably with preliminary registries reporting 0.9-15.2% deaths at 30 days.12-17 However our patient group had a lower NYHA class than other large registries. This finding could be explained by our slightly lower logistic EuroSCORE (24.2±17.0%) most probably due to the lower cut off for reimbursement we have currently in our region. However, it is important to emphasise that with our multi-disciplinary decision making, parameters not captured by the logistic EuroSCORE (previous radiotherapy, liver cirrhosis, porcelain aorta and frailty) were utilised. Notably, with experience our logistic EuroSCORE was reduced from 26.4±15.6% (in 2007-2009) to 21.0±16.7% (in 2010-2011). Recently published registries applying VARC criteria also reported lower logistic EuroSCORE (in Wenewaser et al 24.6±15.3%18 and Nuis et al 12.3% [IQR 9.1-18.4%]19) as compared to preliminary experiences. Interestingly, despite similar logistic EuroSCORE, our 30 day mortality appeared favourable to the 7.5-11.0%18-20 reported by these groups.
Interestingly in PARTNER A, 21 females undergoing TAVI had a lower one year mortality than men (18.4% vs. 28.0%). Furthermore, this was lower in females treated with TAVI as compared to SAVR (18.4% vs. 27.2%). Conversely, in our registry no differences were observed in mortality according to the sex of the patient.
Notably, our stroke rates are significantly lower compared to other series according to VARC (2.3-7.0%)18-20 as well as in PARTNER A (4.6%).21 Preloading of clopidogrel, use of newer generation devices, lower logistic EuroSCORE as well as no routine intracerebral imaging or evaluation by a neurologist unless there was clinical evidence of a stroke could have all played a role in our low rate.
Conversely, life-threatening bleeding occurred in 26.2% overall in our analysis, which is higher than previously reports, including those using VARC which are as low as 8.4%18-20. Although there were no differences in major or life-threatening bleeding between genders, female patients were more likely to undergo blood transfusion. In our institution, the decision for this was at the discretion of the treating physician in the intensive care unit and was assessed according to blood loss and haemodynamics. Initially, blood transfusions were used liberally, with a recent reduction in frequency leading to a significant decrease in this complication in the later two years of our experience (35.6%-14.9%). Clearly the lack of a consensus on the threshold for transfusion for TAVI was one of the reasons for this. Our 1.0% rate of conversion to surgery cannot explain the high rate of bleeding complications which may be the explanation in other series. It has additionally been shown in previous coronary studies that female gender is a powerful predictor of bleeding risk when undergoing interventional procedures.22-25 This has been postulated to be secondary to the increased age of females, as well as their smaller BSA, factors both consistent with our data. Furthermore, TAVI procedures are lengthy in duration and blood loss will inevitably occur.
The major vascular complication rate in our analysis of 15.7% is similar to that reported via VARC by Nuis et al of 16.0%19. Furthermore, our females did have a trend towards increased major vascular complications, indeed female sex was a predictor, which may be due to the older age of the patient, with increased atherosclerosis and tortuosity of the vasculature as well as differences in vessel composition which makes it more prone to injury upon instrumentation. Vascular complications are not rare in the transarterial approach and can correlate significantly with mortality at 30 days.26
Our device success of 92.5% appears good compared to other VARC reports, however the combined safety endpoint is reached by 38.2% of our population compared to 18.4-22.0% in other VARC reported studies18-20. This is likely a consequence of the life-threatening bleeding as our mortality and stroke are lower than those reported by these groups.
This was a single-centre sub-analysis with all inherent limitations. The size was relatively small to allow strong conclusions to be determined. Additionally, the analysis was not aimed at the comparison of longer term follow-up comparing the differences according to sex.
Conclusions
No differences were noted between the sexes undergoing TAVI in composite endpoints. Female sex however was a predictor of major vascular complication leading to females requiring more transfusion. Routine TAVI using both devices appears feasible, with good overall success and outcomes irrespective of the sex of the patient.
Conflict of interest statement
All authors have no conflict of interest to declare.