“The man with a new idea is a crank until the idea succeeds”
From: Following the Equator, Mark Twain
An account of a physician performing a highly technical medical procedure over the internet on a patient several miles away would be typical material for a science fiction magazine but not a prestigious medical journal. Yet, in the current issue of EuroIntervention, Madder and colleagues report that exact notion1.
These investigators performed a remarkable experiment using the CorPath (Corindus Vascular Robotics, Boston, MA, USA) robotic system with the controls connected over the internet. Using this system, coronary stenting was successfully accomplished, first with an ex vivo simulator model and then using an in vivo swine model, by an interventional cardiologist 7.4 kilometres away. This is an amazing technological achievement, but is this just an entertaining parlour trick or does it represent the first step towards a novel healthcare delivery system?
Robotics have been used increasingly in surgery over the past several decades, yet their role in interventional cardiology has been limited. Unlike surgery, where robotics offers a less invasive approach with improved anatomic visualisation, interventional cardiology is already a minimally invasive procedure and angiography already offers exquisite coronary anatomical details. Cardiologists rapidly become adept in the manual techniques currently used to perform percutaneous coronary interventions (PCI) and many procedures can be performed very quickly. Thus, it is difficult to justify robot-assisted PCI on the grounds that it enhances our ability to perform PCI.
The technical aspects of robot-assisted PCI have been described previously2. Briefly, the physician obtains access and engages a guide in the coronary in the usual manner. The guide catheter is connected to the robotic device and a technician loads the guidewire and balloon catheter. The operator sits in a cockpit several feet away employing a joystick to advance, retract or rotate the equipment (Figure 1). This allows the operator to sit down, away from the radiation source and without the need to wear radiation protection gear. The main benefits are enjoyed by the operator. However, these benefits should not be understated. Interventional cardiologists have the highest occupational exposure to radiation3,4 and may be at increased risk of malignancy including brain tumours5. Interventional cardiologists wear heavy, lead aprons for radiation protection and stand for prolonged periods at the procedure table wearing heavy gear contributing to a high rate of orthopaedic injuries such as lumbar and cervical spine injury, as well as knee, hip and ankle arthritis6,7. These may be career limiting. Robot-assisted PCI reduces operator radiation exposure by 95%8 and, while difficult to measure, clearly allows a more comfortable PCI procedure with less operator fatigue which may (ideally) translate into a better outcome. Documented patient benefits of robotic PCI are more limited but include lower contrast use, lower radiation exposure and less geographic miss than with manual PCI9,10. Adoption of this technology has been slow as many centres find it difficult to justify its cost without more tangible patient benefits.
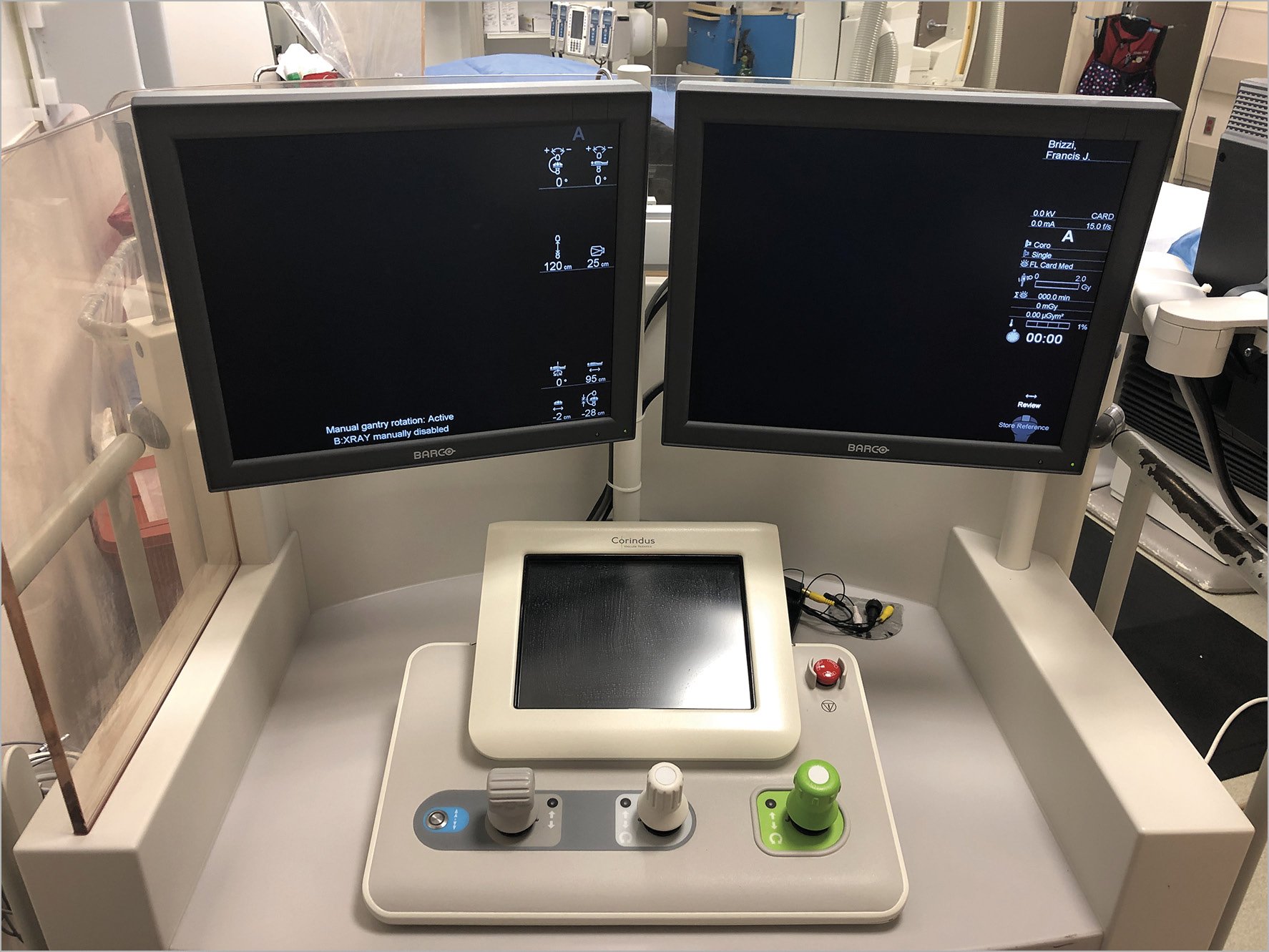
Figure 1. The operator sits in this cockpit to perform robotic PCI. Usually this sits 4-5 metres away from the patient but why not 50-100 kilometres away?
The report by Madder and associates suggests another and entirely novel indication for robot-assisted PCI – allowing an interventional cardiologist to perform PCI on patients remotely at a facility without an interventionalist. This concept has enormous promise. There exist numerous scenarios where telestenting could be applied. While most major population centres (especially in the USA) have no shortage of interventional cardiologists, there remain rural and underprivileged areas throughout the world with no access to an interventional cardiologist. Patients needing interventional services in these areas either have to travel for the procedure, or wait for someone to come to them, or simply do without. This is substandard care for patients with acute, ST-segment elevation myocardial infarction (STEMI) in whom prompt treatment with PCI clearly saves lives. Another scenario relates to the proliferation of low-volume PCI programmes. There are many such programmes and hiring skilled interventional cardiologists, particularly for 24/7 coverage, is challenging. Finally, less skilled interventional cardiologists practising in a low-volume programme typically do not have ready access to more skilled physicians in the event of procedural difficulty. All of these scenarios could potentially be addressed by a skilled interventionalist with a sound internet connection and a robotic platform in the manner suggested by Madder and associates.
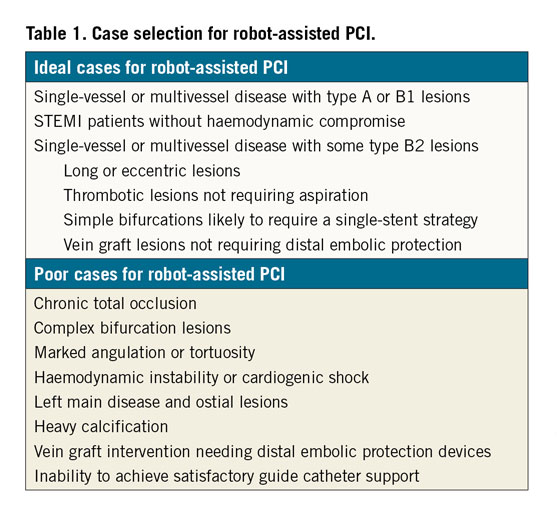
The promise of telestenting is balanced by significant perils. Not all lesions can be treated robotically2 (Table 1). Particularly challenging for robot-assisted PCI are bifurcation lesions needing a two-stent strategy, ostial disease, and lesions that require substantial force to advance balloons and stents such as those with extreme angulation, tortuosity or heavy calcification. Chronic occlusions are not ideal for this technology and the robot cannot perform aspiration thrombectomy or atherectomy, advance or retract a guide extender, position distal embolic protection devices, or allow some intracoronary imaging such as optical coherence tomography (OCT) and intravascular ultrasound (IVUS). More importantly, what happens if the procedure is initiated but cannot be completed robotically? Similarly, what if there is a complication such as a guide dissection, perforation, stent embolisation or vessel closure? The absence of an on-site interventionalist to troubleshoot these scenarios would likely result in a poor outcome. Further, the system is highly dependent on information technology; any technical glitch could spell disaster. On an emotional level, it might be disconcerting for the patient to undergo a procedure in which the operator is miles away. This disconnect in the physician-patient relationship would not be terribly satisfying for the physician either. Finally, the system still requires a skilled operator on site to gain access, engage the coronary artery with an appropriate guide catheter and troubleshoot. Finding an individual with these skills may be just as challenging as finding an interventional cardiologist in the first place. Finally, cost will probably constrain this technology. Areas most likely to need this service are also unlikely to have the means to afford the cost of a system as well as maintain the robust inventory needed to perform PCI.
Despite these issues, the concept of telestenting is a very exciting idea. The work by Madder and colleagues is just the first step. There remains an enormous amount of work to define the system requirements, ideal staff, optimal patient selection and creation of “fail safe” methodology before this could be widely implemented.
Conflict of interest statement
The author has no conflicts of interest to declare.