In 1921 the term robot entered the English language when Karel Čapek’s play “Rossum’s Universal Robots” premiered in Prague. Čapek’s robots were initially happy working with humans but, in the course of the play, a robot rebellion resulted in the extinction of the human race. In subsequent years, robots gradually entered into science fiction literature and film, noting that the robots, by and large, conjured up trepidity and apprehension while nevertheless amassing scores of science fiction devotees. To counter the anxiety, in 1947 the science fiction writer Isaac Asimov devised the “three laws of robots” in which, above all, robots must not harm humans. Remarkably, these laws crossed over into academia and were further adapted by scientists, leading to the seminal publication of the “three laws of responsible robotics” in 2009 in IEEE Intelligent Systems, enshrining the principle that robots must fulfil the highest standards of safety and ethics1.
In medicine, robot technology is no longer science fiction. In the field of surgery, the most well-known robot is the da Vinci® robot-assisted device (Intuitive Surgical Inc., Sunnyvale, CA, USA), which is typically employed for prostatectomies2, gynaecological interventions and, recently, in minimally invasive coronary artery bypass surgery and also mitral valve repair. The primary objective of the da Vinci robot is to enhance surgical precision, noting that a number of publications in the literature cautiously report inconclusive results. Interestingly, the secondary objective is to create the potential for remote surgery from any location in the world.
Another technological development is telemedicine, which not only includes robot-assisted surgical interventions, both on-site and from a distance, but also teleconsultations via secured internet networks. In fact, telemedicine has existed since 1906 when Willem Einthoven sent an electrocardiogram via a telephone line for consultation. Despite the advances in cardiology and its continual expansion into novel yet diverse subspecialties, by comparison the development of telemedicine has been somewhat gradual. However, with the advent of contemporary healthcare digitisation, a new impetus has been created.
This impetus can now also be found in interventional cardiology, a prime example of which is the entry of robotics into the cathlab. Analogous to the surgical field, initial challenges have been overcome, yet many still remain. The level of human dexterity and tactility which a robot must mimic is considerable: take, for instance, the manipulation of a guidewire when crossing severe and complex lesions or traversing tortuous vessels. Other universal operator skills include gaining access to the vascular system, the introduction of a guiding catheter, angiographic filming, the introduction of the guidewire, crossing the lesion, preparing the lesion pre-stenting, positioning the balloon with the stent, and so forth. This is a complex process with an enormous number of manual interactions. An additional difficulty concerns acute interventions with their inherent and sometimes severe limitation of time. Consequently, due to the complex nature of PCI procedures, the adoption of robots in interventional cardiology is unsurprisingly modest. Nonetheless, the field of robot-guided PCI continues to evolve, supported by several publications reporting feasibility results of novel systems3-5.
While the tools and techniques of interventional cardiology continue to advance, occupational hazard awareness has risen significantly as concerns remain regarding radiation exposure, as described in anecdotal case reporting of catastrophic outcomes6 and also in terms of orthopaedic strain7. Robot-guided PCI systems may provide solutions for decreasing or eliminating operator occupational hazards in conjunction with contributing to improved procedural success similar to the achievements attained with surgical robots. An added benefit of the robot-guided PCI system is the concept of performing a remote PCI procedure due to logistical issues of patient transport across vast distances or even heavy traffic in a large metropolis.
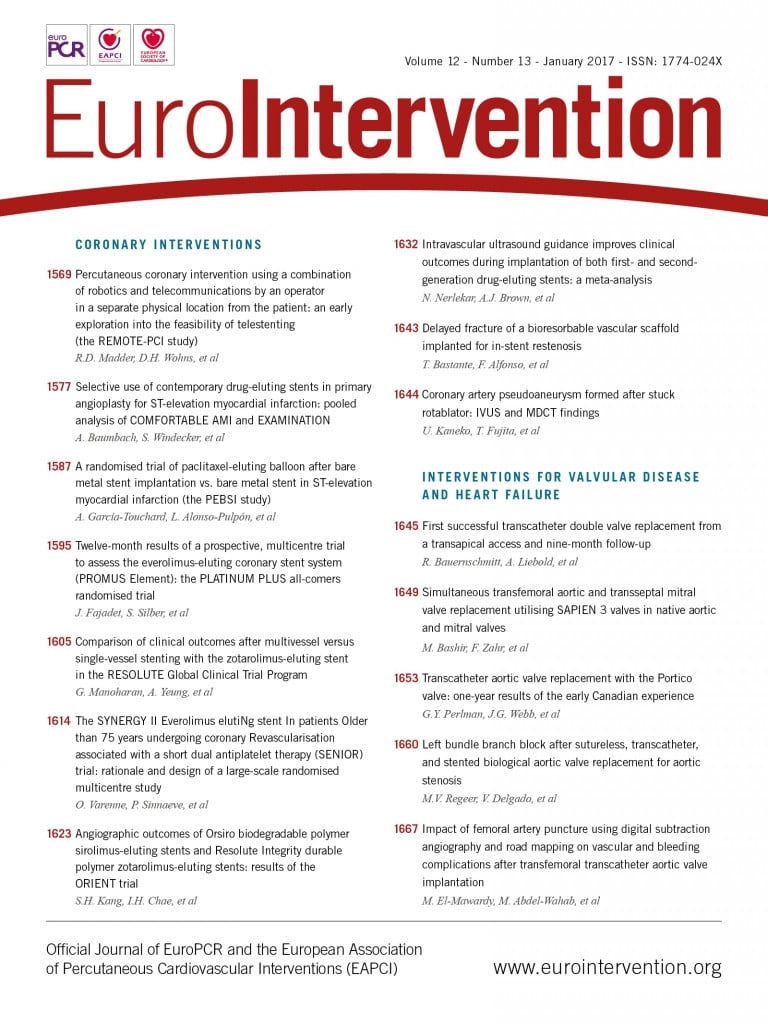
In this issue of EuroIntervention, Madder et al describe their early experience in telestenting, using a combination of robotics and telecommunications in 20 patients who were isolated from the operators during the stent procedure except for the audio and visual connectivity provided by telecommunications devices8. Although the sample size was small and the study had a mono-centre design, it is however an elegant yet tentative attempt in robot-assisted PCI with a technical success rate of 95%. The critical reader will be cognisant of the learning curve involved, the current iteration constraints with respect to the distance limitation of 55 feet between the robotic arm and the controller, and tactile responsiveness. Nonetheless, the technology is incontestably promising and warrants further investigation and development.
When operators are considering the implementation of robot-assisted telestenting in their local practice, the authors of this editorial respectfully point out additional challenges for consideration. The Netherlands traditionally maintains a very high-speed computer network with 63% of its high broadband connections above 10 Mbps, ranking 10th in the world (the USA is ranked 18th globally with 56% above 10 Mbps)9. Conversely, despite the high-speed network in The Netherlands, it is still a challenge to connect hospitals via networks. Technical issues remain, combined with adherence to complex legal requirements in terms of data integrity, security and patient privacy. The technical challenges in The Netherlands are attributed to the fact that real-time sharing of cardiovascular images in a diagnostic, and thus uncompressed, format is currently not possible. Furthermore, to the best of our knowledge, a commercially available system capable of real-time dynamic cardiovascular image sharing in the aforementioned diagnostic quality does not exist. Nevertheless, an alternative solution does exist in the form of image compression. This solution is limited, as a compression ratio of more than 2:1 is not recommended by both the ACC and the ESC10. Operators should bear in mind the fact that the image size and frame rates of angiographic images are too large for uncompressed transfer. Currently available algorithms, which were essentially developed for the consumer market, apply dynamic compression. This form of compression entails the image size itself being decreased to a smaller size, which necessitates fewer pixels, causing significant loss of image detail or, in terms of moving imagery, the reduction of the number of frames, for instance removing every other frame or more. It is worth noting that these algorithms operate fully automatically and adjust themselves depending on the traffic on the network. With these intrinsic limitations it is extremely difficult, if not impossible, to determine the diagnostic quality of the image properties.
Reformatting the images can lead to the removal or addition of minuscule details. Calcified spots and intimal tears could be removed or artificially added. This novel field of inter-hospital real-time cardiovascular image data sharing certainly warrants further evaluation. In addition, access to textual information, such as patients’ medical history (electronic medical health record [EMR]) will also need to be shared securely and, naturally, video conferencing platforms should be provided.
The digitisation of healthcare or eHealth, as described above, provides great opportunities for innovation. The medical arena possesses a great diversification and heterogeneity in systems which brings about its own challenges with respect to uniform connectivity. Fortuitously, electronic standards exist for imagery which allay to some degree connectivity issues, for example IHE11,12, HL713, DICOM14. However, an obligation from medical device manufacturers to commit to and assimilate these electronic medical standards is not only desirable but, one could argue, essential.
Aside from overcoming the technical challenges, fulfilling the patient privacy legal requirement is another issue. In April 2016, the EU issued a new directive, (EU) 2016/680, on the protection of personal data, which will be enforced in all member states no later than 6 May 2018. In essence, this new set of rules returns the control of personal data to EU citizens. Furthermore, data may only be collected legitimately under strict conditions. “Persons or organisations which gather and manage personal information must protect it from misuse and must respect certain rights of the data owners which are guaranteed by EU law. Individuals might also be unwilling to transfer personal data abroad if they were uncertain about the level of protection in other countries”.
In conclusion, the novel concept of robotics and telestenting is intriguing and is deserving of our unswerving attention, not only in terms of the techniques themselves, but also in terms of fulfilling the highest standards of safety and ethics as stipulated in the three laws of responsible robotics. Isaac Asimov encourages us with his reassurance that “there is a single light of science, and to brighten it anywhere is to brighten it everywhere”.
Conflict of interest statement
The authors have no conflicts of interest to declare.