
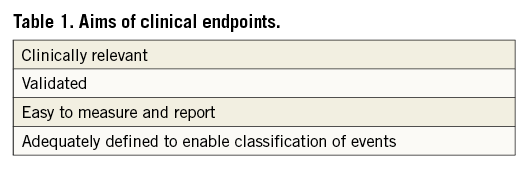
Clinical studies evaluating transcatheter aortic valve implantation (TAVI) are primarily performed to investigate the safety and efficacy of the intervention. They are crucial for initial device evaluation and approval, subsequent utilisation in clinical practice, and in forming the basis of future research and development to address limitations and thus further improve outcomes. The challenge therefore is how to determine exactly what constitutes device success/failure or a complication. This is further complicated by the inherent element of subjectivity in adjudicating a “clinical event”, resulting in a number of different clinical endpoints being used across different studies. Whilst this can make interpretation of observations and their general applicability challenging for individual studies, variability in clinical endpoints across a wide range of studies can be prohibitive to their comparison and to further analysis (e.g., meta-analysis). Defined clinical endpoints should therefore fulfil a number of aims (Table 1), be applicable to all devices being studied, and be regularly updated if necessary to take into account new devices or new device-patient interactions.
With regard to TAVI, the requirement for standardised clinical endpoints and therefore the ability to interpret results and perform comparisons between studies is vitally important. Following the first successful procedure in 20021, this revolutionary technology has been rapidly adopted and is now the recommended treatment of choice for the treatment of patients with severe symptomatic aortic stenosis who are deemed to be inoperable or at high surgical risk2. In recent years, attention has focused on the identification of less common events, longer-term outcomes and also on improving technology and procedural aspects to reduce complications further. This is critical in the evaluation of TAVI for patients of intermediate or lower risk in whom longer-term efficacy is paramount. Whilst the total TAVI patient pool is enlarging with greater usage over time, the relative numbers of patients treated at each centre are low and are inadequate to power studies aimed at identifying low-frequency events or risks. To facilitate timely change, it is vital that numerous clinical studies can be compared in order to obtain adequate statistical power to derive meaningful results.
In an attempt to achieve these aims, the Valve Academic Research Consortium (VARC) was formed and subsequently published criteria for reporting of clinical endpoints in TAVI, initially in 20113 and then again with revised criteria in 20124.
In this issue of the journal, Erlebach and colleagues5 report on the compliance of contemporary TAVI studies with these VARC-defined endpoints. After exclusion of reviews, case reports, small case series and studies not reporting VARC endpoints, 498 of 5,023 published manuscripts between February 2011 and February 2014 were included in the final analysis. Manuscripts were then categorised into being “compliant”, “mixed compliant” or “non-compliant” with regard to their usage of VARC endpoints.
The authors observed that 44.8% of publications did not use any VARC definition, with 45.4% classified as “mixed compliant” and only 9.8% of publications as “compliant”. Not surprisingly, VARC criteria usage increased over time with greater utilisation of VARC-2 criteria following their publication in comparison to the initial VARC-1 criteria, with 74% (n=49) usage after 12-18 months.
Whilst these observations do inform us that the scientific community is improving in applying standardised clinical endpoints to their research, it also highlights that there is a great deal of room for improvement. Further analysis of the results identified that VARC endpoints for valve dysfunction, TAVI-related complications and quality of life were not commonly used. A possible cause of this may be the requirement of a large amount of clinical data to report those endpoints adequately in accordance with the current criteria. Using the assessment of quality of life as an example, current VARC-2 criteria “recommend that a comprehensive assessment of health-related quality of life (HRQOL) for patients undergoing TAVI incorporate both a heart failure-specific measure (such as the Kansas City Cardiomyopathy Questionnaire [KCCQ] or the Minnesota Living with Heart Failure Questionnaire [MLHFQ]) as well as one or more generic measures (such as the Medical Outcomes Study Short Form 36 [SF-36], the Short Form 12 [SF-12], or the EuroQOL [EQ-5D])”. In combination with the observation that the majority (72%) of studies were single-centre investigations and probably retrospective in nature, it may have been that this very comprehensive data set was not available from a retrospective database to enable their accurate reporting. Furthermore, many patients may well have been treated in tertiary level referral centres, with patients then subsequently followed up by their local cardiologist, again resulting in incomplete data collection and the use of non-VARC endpoints. Another possible reason for poor compliance rates may be the absence of a currently accepted “gold standard” for a specific endpoint. For example, the optimal echocardiographic method for the evaluation of aortic regurgitation following TAVI remains unclear6: centre preference for a specific method not incorporated into current VARC criteria may have resulted in deviation from standardised endpoints.
On the other hand, endpoints such as stroke, myocardial infarction and bleeding and vascular complications were frequently reported, probably representing ease of completion and also general acceptance and validation of their definitions. These data therefore demonstrate the importance of designing criteria that are not only functional and validated, but also “user-friendly”. This suggests that the requirement for large amounts of data not routinely collected in clinical practice will result in greater non-compliance with standardised endpoints.
Looking forward, the use of standardised endpoints is going to be critical to evaluate both hard and qualitative clinical outcomes. This is particularly important in relation to TAVI, where practice is rapidly changing due to technical and technological advances and where the representative patient pool is relatively small. The continual revision of endpoint definitions reflecting contemporary practice, new devices, new device-patient interactions and research findings whilst also making them “user-friendly” will be essential to ensure that they are fit for purpose, truly represent contemporary TAVI practice and are more widely adopted. There are other active measures that could be undertaken to increase the compliance with standardised endpoints and wider acceptance by the scientific community, such as endorsement by regulatory groups and professional societies, usage in large randomised controlled trials (RCTs), and having it as a requirement for publication, especially for hard clinical endpoints. It may also require us to employ innovative solutions such as E-polling in order to get a larger consensus and buy-in from the scientific community, particularly with regard to controversial and debatable endpoint definitions.
In conclusion, significant progress has been made in realising the goal of standardised outcomes for TAVI clinical trials; however, a concerted effort by researchers, editorial boards and stakeholders is required to improve compliance further and build upon the progress already made in this area.
Conflict of interest statement
A. Latib is a consultant for Medtronic and Direct Flow Medical. N. Ruparelia has no conflicts of interest to declare.

