Abstract
Aims: The aim of this study was to examine the relationship between the anatomical SYNTAX score (SXscore), derived from all three coronary arteries, and coronary wall pathology measured by radiofrequency intravascular ultrasound (RF-IVUS) and near-infrared spectroscopy (NIRS) in a single non-culprit segment.
Methods and results: In patients referred for coronary angiography (N=88) or PCI (N=592) for stable angina or acute coronary syndrome, the SYNTAX score calculator (www.syntaxscore.com) was used to determine the SXscore before PCI, if applicable. RF-IVUS and/or NIRS were performed in a non-stenotic 40 mm study segment following the clinically indicated angiography/PCI. After adjustment for multiple confounders, a higher SXscore was associated with higher segmental plaque volume in the study segment (2.21 mm3 per SXscore point, 95% CI: 0.92-3.50, p-value 0.001), as well as with higher volume of fibrous (0.93 mm3 per point) and fibro-fatty tissue (0.29 mm3 per point). A higher SXscore was also associated with a higher NIRS-derived lipid core burden index (LCBI) in the full study segment (1.35 units per SXscore point, 95% CI: 0.22-2.47, p-value 0.019). Importantly, SXscore correlated with the fatty/fibro-fatty and LCBI signals despite adjusting for plaque burden.
Conclusions: In patients with CAD, higher SXscores are associated with higher atherosclerotic burden as assessed by RF-IVUS and NIRS in a single non-stenotic coronary artery segment.
Abbreviations
ACS: acute coronary syndrome
ATHEROREMO-IVUS study The European Collaborative Project on Inflammation and Vascular Wall Remodeling in Atherosclerosis - IVUS study
CABG: coronary artery bypass graft surgery
CAD: coronary artery disease
CAG: coronary angiography
CI: confidence interval
IBIS-3 study: Integrated Biomarker and Imaging Study 3
IQR: interquartile range
LCBI: lipid core burden index
MACE: major adverse cardiac events
MLA: minimal luminal area
NIRS: near-infrared spectroscopy
PCI: percutaneous coronary intervention
RF-IVUS: radiofrequency intravascular ultrasound
SAP: stable angina pectoris
SD: standard deviation
STEMI: ST-segment elevation myocardial infarction
SXscore: SYNTAX score
TCFA: thin-cap fibroatheroma(s)
Introduction
The SYNTAX score (SXscore) is an angiographic tool that grades the complexity of coronary artery disease (CAD) and is also used for short- and long-term prediction of major adverse cardiac events (MACE) in patients undergoing percutaneous coronary intervention (PCI) and/or coronary artery bypass graft surgery (CABG)1,2. The severity and composition of coronary atherosclerosis as assessed by radiofrequency intravascular ultrasound (RF-IVUS) and near-infrared spectroscopy (NIRS) in one (non-)stenotic coronary artery segment have recently also shown prognostic value for MACE3-8. Furthermore, RF-IVUS and NIRS in one (non-)stenotic coronary artery segment have previously been used to evaluate the effects over time of antiatherosclerotic therapy under the assumption that these assessments are representative of the total coronary atherosclerotic burden9. However, how well the atherosclerotic burden as graded by NIRS and RF-IVUS measured in one (non-)stenotic coronary artery segment correlates with the atherosclerotic burden as assessed by the SXscore which is derived from all three coronary arteries has never been investigated in a large cohort.
It is important to realise that the three methods differ from each other in the assessment and quantification of CAD. The SXscore is an anatomical scoring tool that grades luminal coronary obstruction, directly from the coronary angiography (CAG). Therefore, it lacks detail with respect to coronary artery wall pathology. Conversely, RF-IVUS and NIRS have been shown to provide information on plaque morphology in the imaged coronary segment. However, both of these imaging techniques require additional intracoronary catheters, whereas the SXscore itself does not require instrumentation of the coronary lumen.
The aim of this study was to examine the relationship between the coronary atherosclerotic burden measured as luminal coronary obstruction graded by the SXscore, derived from all three coronary arteries, and the atherosclerotic burden by assessing coronary artery wall pathology measured by RF-IVUS and NIRS in one non-stenotic segment of a single non-culprit coronary artery.
Methods
STUDY POPULATION
This study constitutes a combined analysis of two cohorts, The European Collaborative Project on Inflammation and Vascular Wall Remodeling in Atherosclerosis - IVUS (ATHEROREMO-IVUS) study and the Integrated Biomarker and Imaging Study 3 (IBIS-3). The design of both studies has been described elsewhere9-11. In total, 770 patients with an indication for diagnostic CAG and/or PCI due to either stable angina pectoris (SAP) or an acute coronary syndrome (ACS) were included and had an RF-IVUS and/or NIRS performed in a non-stenotic segment of a non-culprit coronary artery.
Both studies were approved by the Medical Ethics Committee of the Erasmus MC and performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all included patients. ATHEROREMO-IVUS is registered at ClinicalTrials.gov (NCT01789411), and IBIS-3 is registered in the Netherlands trial register (NTR2872).
CORONARY INTRAVASCULAR ULTRASOUND AND NEAR-INFRARED SPECTROSCOPY
RF-IVUS and NIRS methods have been described in detail previously9-11. For a comprehensive Methods section, refer to Supplementary Appendix 1.
SYNTAX SCORE
The SXscore was calculated (pre PCI) for every CAG taken at study entry using the SYNTAX score calculator (www.syntax score.com). Details concerning the calculation of the SXscore have been described elsewhere1. In brief, the three coronary arteries are divided into 16 segments, each with a corresponding weighting factor. If there is a lesion producing 50% or more luminal obstruction, the weighting factor is added. Moreover, other factors that reflect the severity of the atherosclerotic lesion and the possible difficulty of a percutaneous treatment, for example lesion length and diffuse disease of the vessel, are taken into account. Eventually, all points are summed to obtain the SXscore reflecting the complexity of the CAD of the patient.
As applied in other all-comers and ST-segment elevation myocardial infarction (STEMI) populations, lesions caused by in-stent restenosis were considered as de novo lesions12-14. Occlusions in patients presenting with ACS were scored as occlusions of unknown duration, as the analyst was blinded to all other patient information15.
In case of a co-dominant coronary artery circulation, the vessel mainly responsible for the perfusion of the posterior side of the heart was designated as the dominant coronary artery. Lastly, patients with a pre-existing CABG, whose CAG was unquantifiable using the SXscore, were excluded.
The SXscores were determined by a trained analyst who was blinded with respect to other patient characteristics and clinical outcome.
STATISTICAL ANALYSIS
Categorical variables are presented as numbers and percentages. The distribution of the continuous variables, including RF-IVUS and NIRS parameters, was examined for normality with Kolmogorov-Smirnov tests. Normally distributed continuous variables are presented as mean±standard deviation (SD). Non-normally distributed continuous variables are presented as median and interquartile range (IQR). SXscores were categorised into tertiles based on the distribution of the SXscores in the particular group that was being examined. Kruskal-Wallis tests were used for multiple group comparison of continuous variables. Categorical variables were compared using Pearson chi-square tests or Fisher-Freeman-Halton exact tests when appropriate.
Linear and logistic regression analyses were applied to evaluate the relation between SXscore (explanatory) and RF-IVUS- and NIRS-derived (dependent) variables. Variables concerning plaque volume were first normalised for the imaged segment length (i.e., normalised plaque volume=plaque volume/imaged segment length*median segment length of study population). In multivariable analyses, age, gender, hypertension, renal impairment, hypercholesterolaemia, diabetes mellitus, smoking, indication for CAG, history of PCI, as well as segmental plaque burden were entered as potential confounders/explanatory factors. Thus, the models allow a conclusion on the relation between SXscore and the RF-IVUS/NIRS imaging signals, irrespective of the patient’s segmental plaque burden. Assumptions underlying linear regression models were evaluated by visual examination of the residuals.
All statistical tests were two-tailed and p-values <0.05 were considered significant. SPSS, Version 21.0 (IBM Corp., Armonk, NY, USA) was used for all the analyses.
Results
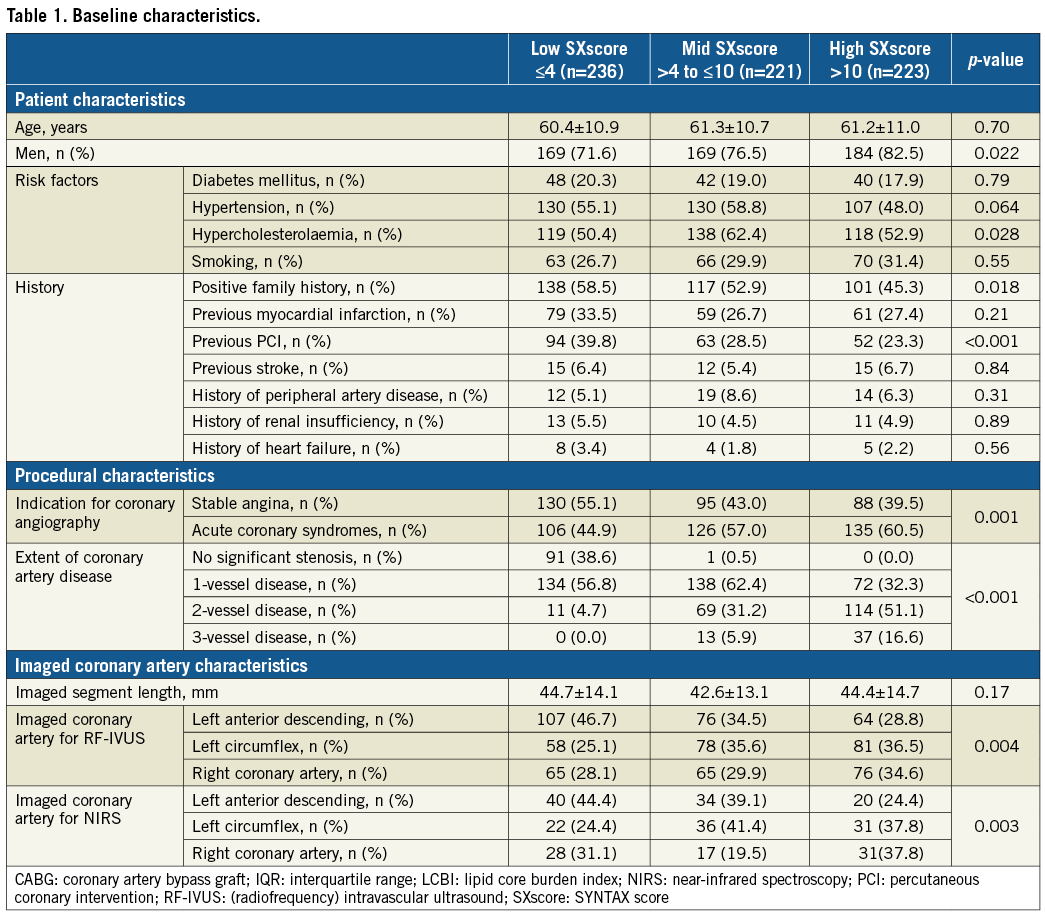
BASELINE CHARACTERISTICS
The current study included 680 patients from the combined ATHEROREMO-IVUS and IBIS-3 cohorts (Figure 1). The overall SXscore ranged from 0 to 37.5 with a median of 7 (IQR: 3-13) and a mean of 8.6±7.4. Baseline clinical and angiographic variables were stratified according to tertiles reflecting the obtained SXscores (lowest tertile, ≤4; middle tertile, >4 to ≤10; highest tertile >10) (Table 1). The highest tertile comprised more men. As expected, more patients in the higher tertiles exhibited two- or three-vessel disease, whereas no significant stenosis or one-vessel disease was more frequently present in patients with the lowest SXscores. More patients with lower SXscores had previously undergone a PCI.
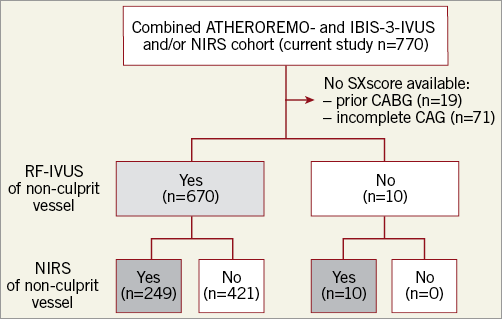
Figure 1. Patient inclusion. RF-IVUS was available in 670 patients (light grey) and NIRS was available in 259 patients (dark grey). ATHEROREMO-IVUS: The European Collaborative Project on Inflammation and Vascular Wall Remodeling in Atherosclerosis- IVUS study; IBIS-3: Integrated Biomarker and Imaging Study-3; NIRS: near-infrared spectroscopy; RF-IVUS: radiofrequency intravascular ultrasound; SXscore: SYNTAX score
CORONARY INTRAVASCULAR ULTRASOUND IN RELATION TO SXSCORE
After adjustment for multiple confounders/explanatory factors, a higher SXscore was associated with a higher plaque volume in the study segment (2.21 mm3 per SXscore point, 95% CI: 0.92-3.50, p-value 0.001) (Table 2). The relation between SXscore and plaque burden was consistent with this observation, although statistically non-significant (p-value 0.078). A higher SXscore was also associated with a higher volume of fibrous (0.93 mm3 per SXscore point, 95% CI: 0.53-1.33, p-value <0.001) and fibro-fatty tissue (0.29 mm3 per SXscore point, 95% CI: 0.17-0.42, p-value <0.001) (Table 2, Figure 2). Importantly, the SXscore correlated with the fatty/fibro-fatty signals despite adjusting for plaque burden. In contrast, we found no association between SXscore and necrotic core volume (p-value 0.16) or the presence of thin-cap fibroatheroma (TCFA) (p-value 0.46).
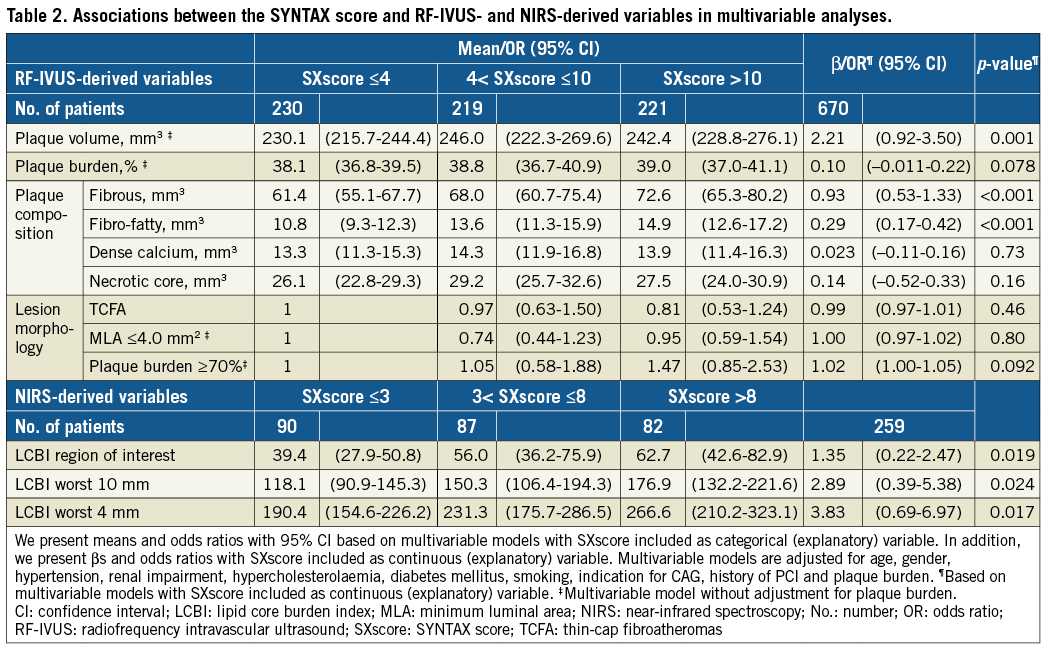
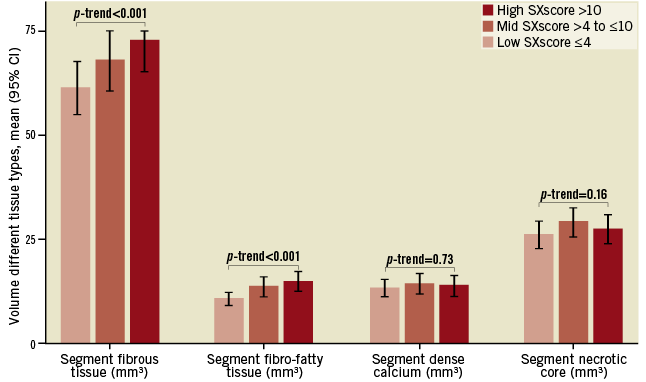
Figure 2. Distribution of RF-IVUS-derived plaque components across the SXscore categorised in tertiles. The mean volumes of the different plaque components (fibrous, fibro-fatty, dense calcium and necrotic tissue) are divided across the SXscore categorised in tertiles (cut-off points 4 and 10). RF-IVUS: radiofrequency intravascular ultrasound; SXscore: SYNTAX score
NEAR-INFRARED SPECTROSCOPY IN RELATION TO SXSCORE
A higher SXscore was associated with a higher NIRS-derived lipid core burden index (LCBI) in the full study segment (1.35 units per SXscore point, 95% CI: 0.22-2.47, p-value 0.019) (Table 2, Figure 3). Consistent results were observed for the 10 and 4 mm segments with highest LCBI values. Again, it is relevant to note that the observed correlation between SXscore and LCBI signals was independent of segment plaque burden.
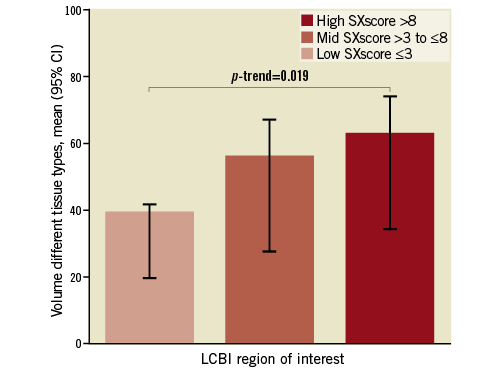
Figure 3. Distribution of NIRS-derived LCBI across the SXscore categorised in tertiles. The mean LCBI of the region of interest is divided across the SXscore categorised in tertiles (cut-off points 3 and 8). LCBI: lipid core burden index; SXscore: SYNTAX score
Discussion
This is the first study, to our knowledge, to have examined systematically a large patient population for the correlation of coronary atherosclerotic burden as determined by the SXscore and the extent and characteristics of coronary atherosclerosis as assessed by RF-IVUS and NIRS in one non-stenotic segment of a single non-culprit coronary artery. This study shows that there is a significant and independent association between these entities in patients with CAD.
The SXscore is a well-established angiographic tool for the assessment of the severity and complexity of CAD2. It not only evaluates the number of significant stenoses but also lesion length and the amount of calcification, amongst others. Still, as the SXscore is based on coronary luminography, it is limited in the assessment of the extent of (non-stenotic) plaque burden and plaque morphology, including the identification of high-risk plaque characteristics and vulnerable plaques. We demonstrated that the SXscore is associated with RF-IVUS- and NIRS-derived information on the extent and composition of coronary atherosclerosis in patients with CAD. The correlation between SXscore and the amount of fatty/fibro-fatty tissue as well as LCBI was most striking. In this respect, it is relevant to note the absence of relations between SXscore and plaque phenotype (necrotic core volume) and lesion morphology (TCFA).
Previously, a significant relation between atherosclerotic burden in one non-culprit coronary segment as assessed by RF-IVUS or NIRS and cardiovascular outcome was demonstrated which persisted after exclusion of culprit-related and imaged segment-related cardiac events5,7. This indirectly supported the assumption that the atherosclerotic burden in one non-culprit coronary segment may be representative of the atherosclerotic disease of the entire coronary tree. The current study shows a direct association between the angiographic atheroma burden of all three vessels and intravascular coronary wall evaluation of a non-culprit segment.
Although pre-specified high-risk plaque phenotypes (TCFA, MLA ≤4.0 mm2 and lesions with a plaque burden of ≥70%) were not significantly associated with an increase in SXscore, the volume of fibrous and fibro-fatty tissue in plaques was higher in patients with a higher SXscore. Although a previous study has shown that plaque morphology, as measured by three-vessel imaging by optical coherence tomography (OCT) or IVUS, is associated with and may be used for the identification of vulnerable plaques in patients with ACS16, it appears from our study that it is the amount of tissue type which is associated with SXscore and not plaque morphology (the layout of the tissue) per se. In the light of the relatively low overall angiographic burden of disease in our population, however, it needs to be considered that this finding may not be applicable in a patient population with more advanced CAD. Moreover, necrotic core and dense calcium did not show a significant association with a higher SXscore.
Previously, in one other small cohort, the relationship between NIRS and SXscore was explored but no association was found17. The relationship between NIRS and the SXscore has also been studied in a subset of patients from ATHEROREMO-IVUS18. The enrichment of the ATHEROREMO-IVUS cohort with the IBIS-3 cohort in the current study substantially increases the sample size and creates more robust data.
In most studies, SXscore is stratified in tertiles or even quartiles, reflecting the distribution of the scores found in the respective cohort2. The thresholds of the original SYNTAX trial (cut-off points: 22 and 33) have been incorporated in the guidelines for the decision making regarding CABG and PCI, but these thresholds apply to patients with left main and/or three-vessel disease19. Our population also consisted of patients with single- or two-vessel disease and hence, understandably, our mean SXscore and cut-off values for the tertiles were relatively low. Further research is warranted to assess which absolute SXscore thresholds are applicable in a heterogeneous population for risk prediction of adverse outcome in patients with CAD.
Furthermore, we argue that combined IVUS-NIRS intracoronary imaging holds promise for more precise detection and quantification of atherosclerotic burden in patients with CAD, and in the future may even be of interest for the prediction of adverse events. However, further research is warranted to assess the application of combined IVUS-NIRS intracoronary imaging for the prediction of adverse events.
Limitations
This cohort, composed of two prospective studies, has broad inclusion criteria which enable the results to be applicable to a broad patient population with CAD. Data collection, processing and analyses were conducted by independent researchers blinded to patient and outcome data. However, a few limitations deserve consideration.
As indicated, our study includes patients with relatively low SXscores. This might induce an underestimation of the studied associations and insufficient power to reveal additional associations. However, a subgroup analysis with exclusion of patients without significant CAD showed results that were essentially similar. Moreover, the lowest tertile in this cohort contains significantly more patients with a previous PCI, which may indicate an underestimation of the severity of CAD caused by a low SXscore derived at study entry.
Furthermore, while the SXscore analyst was blinded to all patient information, occlusions in STEMI patients were scored as occlusions of unknown duration. In the MI SYNTAX score study, it was proposed to calculate occlusions in STEMI patients post wiring20. However, the MI SYNTAX score did not show better performance than the original SXscore calculated in STEMI patients.
Lastly, although the literature has demonstrated that experienced operators produce reasonable SXscores, the modest reproducibility of the SXscore in general has to be acknowledged21. However, because of the overall relatively low angiographic burden of disease in our study population, we expected a fair reproducibility of the SXscore in our study. To address the reproducibility of our SXscores, a second experienced operator, blinded to patient characteristics and previously scored SXscores, repeated SXscore analysis in a representative random sample. Cohen’s kappa was shown to be 0.91, indicating a good interobserver agreement.
Conclusions
In patients with CAD, there is a clear and significant correlation between a higher SXscore and a higher atherosclerotic burden as assessed by RF-IVUS and NIRS in one non-stenotic segment in a single non-culprit coronary artery.
| Impact on daily practice This study shows that RF-IVUS and NIRS imaging in one non-culprit coronary artery segment reflects overall coronary atherosclerotic burden in patients with CAD. Our findings may support the use of RF-IVUS and NIRS in one single non-culprit coronary artery segment for the evaluation of the atherosclerotic burden in patients with CAD over time. However, trials are needed to investigate the suitability of assessing dynamic changes in plaque composition to predict outcome benefit with therapeutic interventions. |
Guest Editor
This paper was guest edited by Alec Vahanian, MD, PhD; Department of Cardiology, Hôpital Bichat-Claude Bernard and University Paris VII, Paris, France.
Funding
ATHEROREMO-IVUS was funded by the Seventh Framework Programme (FP7), theme FP7-HEALTH-2007-2.4.2-1. IBIS-3 was supported by AstraZeneca, Infraredx and Volcano Corporation. The study was initiated by the investigators, and was designed, conducted, interpreted and reported independently of these sponsors.
Conflict of interest statement
R-J. van Geuns has received grants from Abbott Vascular and Boston Scientific. P. Serruys has received personal fees from Abbott Laboratories, AstraZeneca, Biotrinik, Cardialysis, GLG Research, Medtronic, Sino Medical Sciences Technology, Société Europa Digital Publishing, Stentys France, Svelte Medical Systems, Philips/Volcano, St. Jude Medical, QualiMed, Xeltis. The other authors have no conflicts of interest to declare. The Guest Editor is a consultant for Edwards Lifesciences.
Supplementary data
Supplementary Appendix. Methods.
To read the full content of this article, please download the PDF.