Angiography is the most commonly used method to guide percutaneous coronary intervention (PCI). However, angiography has a number of limitations. It only provides luminal morphology in a two-dimensional view of a complex 3-dimensional structure and does not provide information about plaque characteristics, vascular remodelling, or stent underexpansion after PCI. These drawbacks can be overcome by intravascular ultrasound (IVUS) guidance. IVUS provides valuable information on the cross-sectional coronary vascular structure and plays a key role in contemporary stent-based PCI by accurately assessing the coronary anatomy, assisting in the selection of treatment strategy, and defining optimal stenting outcomes. Many randomised trials and observational cohort studies have shown that IVUS guidance can achieve a larger luminal diameter than angiography guidance. In a recent meta-analysis, Ahn et al reported that IVUS-guided PCI was associated with larger stents and a larger post-procedural angiographic minimal lumen diameter compared with angiography-guided PCI1. The mean difference in stent size and in post-procedural minimal lumen diameter was 0.33 mm (95% confidence interval [CI]: 0.22-0.44, p<0.001) and 0.34 mm (95% CI: 0.27-0.40, p<0.001), respectively. IVUS guidance was also associated with more stents and longer stents, and the mean difference in the number and length of stents used was 0.27 (95% CI: 0.11-0.43, p<0.001) and 0.18 mm (95% CI: 0.08-0.27, p<0.001). Because the post-procedural minimal stent area achieved is one of the most important determinants of MACE after stenting2, achievement of larger luminal dimensions with IVUS guidance might lead to better clinical outcomes.
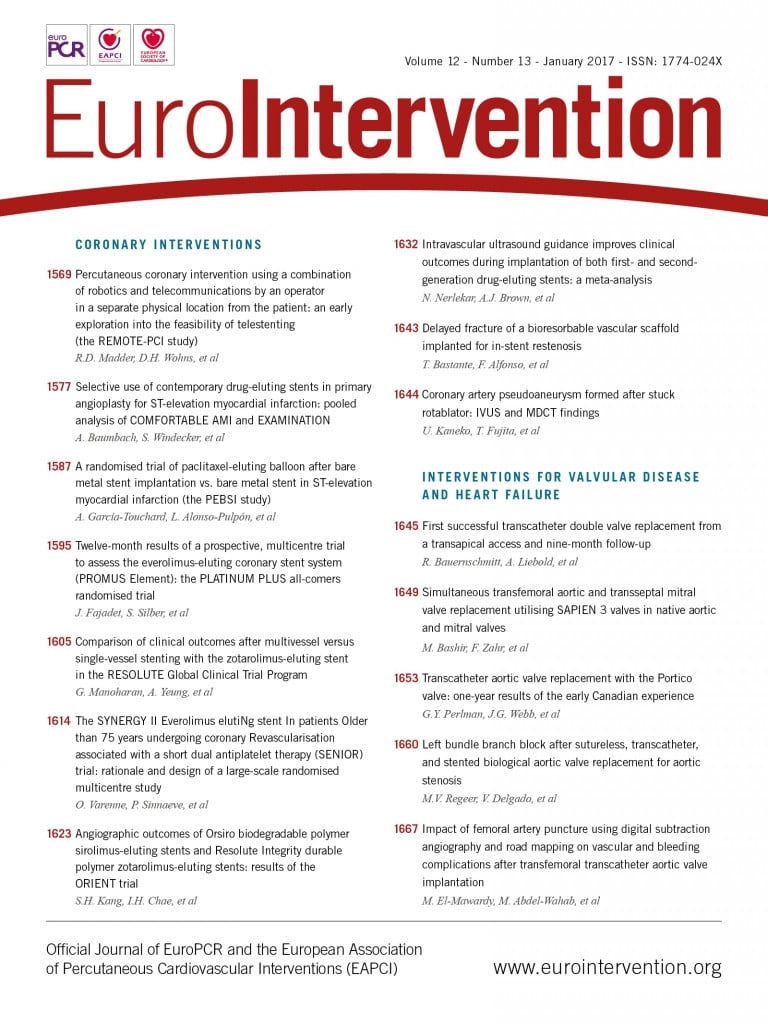
In this issue of EuroIntervention, Nerlekar et al3 report an extensive meta-analysis concerning the clinical impact of IVUS-guided drug-eluting stent (DES) implantation. In a total of 9,313 patients from six randomised trials and nine observational studies, IVUS guidance showed a significant reduction in major adverse cardiac events (MACE) compared with angiography guidance (odds ratio [OR] 0.71, 95% CI: 0.64-0.85, p<0.001). The difference was not only driven by the reduction of target lesion revascularisation (OR 0.77, 95% CI: 0.52-0.84, p<0.001), but also by the hard MACE endpoints of cardiac death (OR 0.55, 95% CI: 0.36-0.83, p=0.005), myocardial infarction (OR 0.67, 95% CI: 0.50-0.90, p=0.01), and stent thrombosis (OR 0.56, 95% CI: 0.40-0.79, p<0.001). In addition, the difference was consistent across first- and second-generation DES and a progressive trend towards a greater beneficial effect to reduce MACE was observed (OR 0.60, 95% CI: 0.48-0.75, p<0.001). Therefore, the authors suggested that the use of IVUS guidance should be encouraged in contemporary PCI.
Because only studies which were stratified by stent generation were included, the size of the data set decreased to 9,313 patients. However, the proportion of patients enrolled in randomised controlled trials has risen to 32% with recently published randomised trials, in comparison with the high proportion of observational data in previous meta-analyses (98.1% in Ahn et al1, 96.4% in Zhang et al4). Therefore, this study is based on one of the best data sets specifically regarding second-generation DES and is the first to evaluate a positive temporal trend between stent generations. Because the use of new-generation DES produces better clinical outcomes compared to first-generation DES, it is claimed that the clinical benefit of IVUS would be smaller in second-generation DES compared to first-generation DES. Nevertheless, a clinical benefit for the clinical endpoint was also revealed in second-generation DES, even stronger in the recent studies with a progressive temporal trend. More recent large-volume clinical trials using second-generation DES have enrolled patients with difficult lesion characteristics. The CTO-IVUS trial enrolled 402 patients with chronic total occlusions5 and the IVUS-XPL trial enrolled 1,400 patients with long coronary lesions (stent length ≥28 mm)6. Tan et al enrolled a total of 123 elderly patients with unprotected left main disease7. Therefore, the trend would imply that IVUS guidance is especially beneficial during complex PCI such as for chronic total occlusions or long lesions. In addition, improved IVUS catheters and better image quality could contribute to the beneficial effect.
The role of intravascular imaging is also highlighted in bioresorbable vascular scaffold (BVS) implantation. The recently published ILUMIEN III: OPTIMIZE PCI trial reported that intravascular imaging-guided BVS implantation, including optical coherence tomography (OCT) and IVUS, displayed a larger stent area than with angiographic guidance (5.79 mm2 with OCT, 5.89 mm2 with IVUS, and 5.49 mm2 with angiography)8. The currently ongoing GUIDE-BVS trial (NCT02831218) comparing clinical outcomes between intravascular imaging and angiography-guided BVS implantation will address the role of intravascular imaging in the BVS era.
IVUS enables accurate lesion assessment, adequate stent selection and optimal stent outcome by way of increased stent size and minimal luminal diameter. Well composed IVUS images make for a good post-procedural result, thus achieving a good long-term clinical outcome. Small details make a big difference!
Conflict of interest statement
The authors have no conflicts of interest to declare.