Intravascular ultrasound (IVUS) is the most common intravascular imaging method used to guide percutaneous coronary intervention (PCI). Several recent studies have shown that IVUS guidance has a better PCI outcome compared to angiography guidance1. These studies consistently suggest that post-stenting IVUS influences stent optimisation strategies and, as a result, increases post-PCI minimum stent area and improves the PCI outcome. However, the impact of pre-stenting IVUS on procedural and clinical outcomes has not been fully investigated.
Present study
In the current issue of EuroIntervention, Hong et al report the clinical significance of pre-stenting IVUS in IVUS-guided PCI2.
Pre-stenting IVUS was associated with a larger post-PCI minimum stent area in patients with acute myocardial infarction (AMI) or small vessel disease and better one-year clinical outcomes in patients with chronic total occlusion (CTO). The authors attributed these clinical benefits of pre-stenting IVUS primarily to the selection of larger diameter stents.
Pre-stenting IVUS
There are two possible reasons why IVUS guidance leads to the selection of larger diameter stents compared to angiographic guidance. First, angiography guidance determines the stent diameter based on the lumen diameter at the reference site, while IVUS guidance often determines the stent diameter based on the vessel diameter (i.e., external elastic membrane diameter) at the reference site. A more aggressive IVUS guidance determines the stent diameter based on the vessel diameter at the minimal lumen area site in the lesions presenting with positive arterial remodelling. Second, IVUS estimates the lumen diameter more accurately when compared to angiography. Angiography is inherently limited by its two-dimensional lumen display with respect to lumen assessment. In addition, the image size of angiography is influenced by the distance from the calibration point to the X-ray source. Therefore, the measurement of coronary lumen by angiography is likely to deviate from the actual size. Angiography frequently underestimates the size of coronary arteries. A previous study showed that IVUS measurements were more accurate and about 13% larger than angiographic measurements3.
IVUS is useful in guiding primary PCI for AMI4. Angiography has limitations in assessing reference vessels distal to the occlusive lesions. Predilatation does not always result in adequate restoration of coronary blood flow. Since IVUS works even in coronary arteries with reduced blood flow, this technique can assess distal reference vessel dimensions and lesion length in AMI. Therefore, IVUS allows the optimal selection of stent size and stent landing zones in AMI.
Angiographic measurements of small vessels are less accurate3. The resolution of angiography is not enough to delineate the lumen boundaries clearly. Even small errors in identifying lumen boundaries can have a significant impact on lumen diameter measurements, especially for small vessels. Since small vessel disease has a high risk of restenosis after PCI, the selection of a larger diameter stent based on accurate vessel measurements by IVUS is important to increase post-PCI minimum stent area and improve PCI outcomes.
IVUS is an indispensable imaging method to guide PCI for CTO5. IVUS distinguishes whether the guidewire is in the true lumen or subintimal space. In the CTO occurring at the bifurcation, IVUS placed in the side branch allows us to identify the origin of the main vessel occlusion. During retrograde CTO PCI, IVUS can effectively guide the controlled antegrade and retrograde subintimal tracking (CART or reverse CART) technique. IVUS after guidewire crossing of the CTO lesion allows accurate assessment of the longitudinal extent of vascular injury due to wire manipulation or predilatation and helps adequate stent coverage of the lesion without leaving untreated plaques or dissections. In addition, IVUS guidance in PCI for CTO reduces contrast agent usage and improves PCI safety.
Final remarks
Pre-stenting IVUS is used to plan the PCI strategy. The role of pre-stenting IVUS is to measure the vessel and lumen cross-sectional dimensions, estimate longitudinal lesion length, analyse plaque characteristics, and assess morphological lesion complexity (Figure 1). According to the results of the study by Hong et al, pre-stenting IVUS changes PCI procedures, including the selection of a larger diameter stent, and exerts a favourable impact on PCI outcomes.
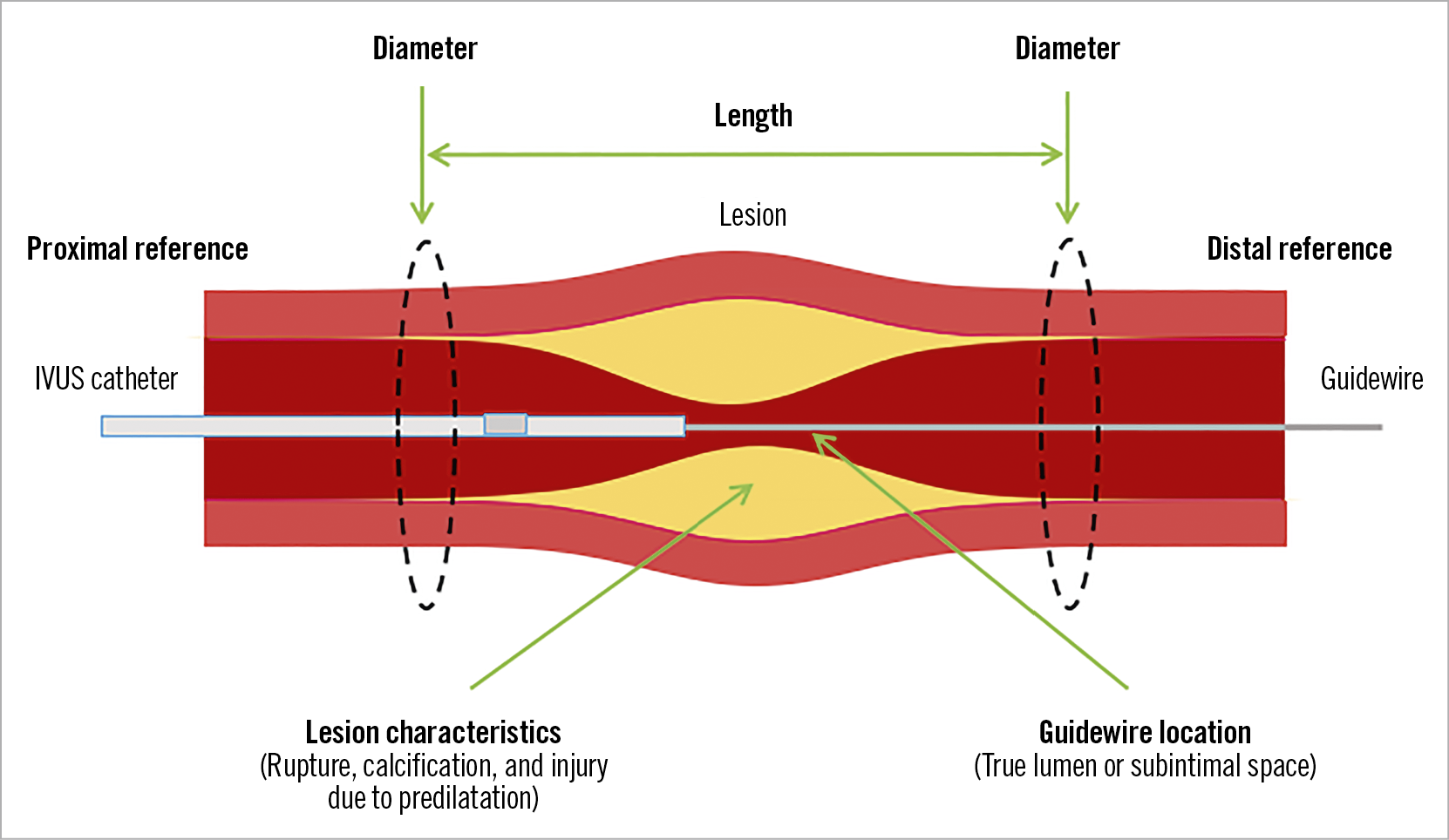
Figure 1. Role of pre-stenting IVUS. IVUS information on reference vessel/lumen diameter, lesion length, lesion characteristics and guidewire location can help with optimal stent implantation.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.