The past few weeks have reminded us, if ever there was a need, that the peer review process is imperfect and fraught with dangers. In the space of a few days, authors of COVID-19 studies published in prestigious journals such as The Lancet and the New England Journal of Medicine have retracted their articles due to the inability to access raw data and validate the study findings after serious criticisms were raised on their strength and reliability. In particular, many have wondered how it was possible that the owners of the data had such large data sets of COVID-19 patients, in contrast to the numbers reported at national level by official sources. This story underlines the fragility of the review process of COVID-19 papers in these incredible months, where journals have been struggling with the need to inform their readers without compromising on quality and scientific rigour. Here at EuroIntervention, from the outset we have chosen a very prudent strategy in relation to articles on COVID-19. We have decided to consider only a few original contributions and consensus documents to enter the revision process, and suggested to the authors of other types of contribution (e.g., checklists, standard operating protocols) that they submit these for the attention of the editorial board of PCRonline, for quicker dissemination in case of acceptance. I can’t say that I’m sorry about how prudent we have been after seeing how complex it is to manage and verify these submissions, even for journals with a higher impact factor than ours. It is definitely better to stay in our comfort zone and do what we are primarily asked to do in these pages, which is to try to give you the best of what is submitted for our attention in the field of interventional cardiology. With that goal in mind, here is a summary of what you will find in this July’s issue of EuroIntervention.
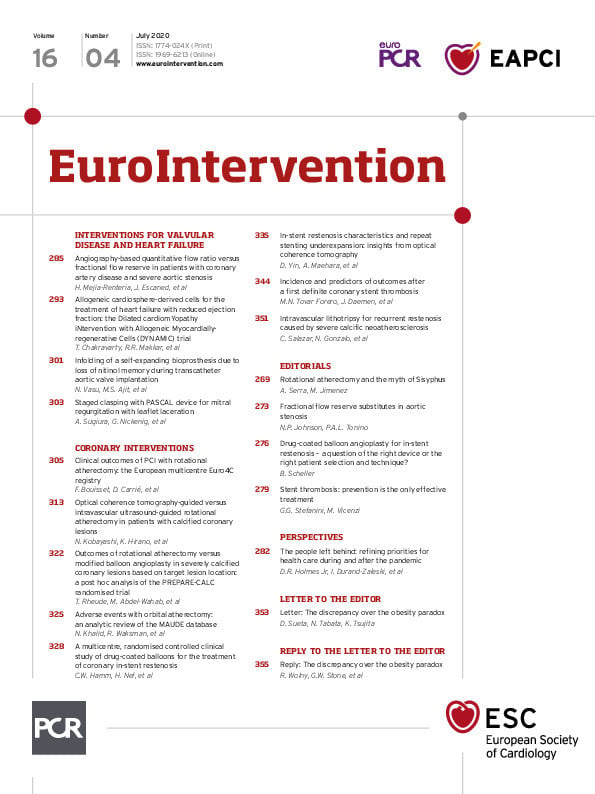
The section on coronary interventions this month hosts a series of studies on modification of calcified plaques. Frédéric Bouisset, Didier Carrié and colleagues present the Euro4C registry, the first large international prospective cohort focusing on percutaneous coronary intervention procedures performed with rotational atherectomy. This study included 966 patients from 19 centres and 8 European countries, a complex subset with 43% of diabetes, 25% of left main disease, 38% of three-vessel disease and 29% with at least one chronic total occlusion. In this context, rotational atherectomy ended with 92% technical success and major adverse events in 13% at 1 year. This is a reference paper if you want to learn more on the outcomes of this technique in the contemporary era of interventional cardiology, accompanied by an editorial from Antonio Serra. In another study, Norihiro Kobayashi, Keisuke Hirano and colleagues explore the value of intravascular imaging as a guidance for rotational atherectomy, comparing the outcome of optical coherence tomography and intravascular ultrasound. Interestingly, they found that burr upsizing was more frequently performed and that the final burr size was significantly larger in the group guided by optical coherence tomography, which also led to greater percent stent expansion as compared with intravascular ultrasound. The authors conclude that optical coherence tomography may be the ideal tool to improve the clinical outcomes of calcified coronary lesions.
Two short reports complete our mini-focus on calcified lesions. The first study, from Tobias Rheude, Mohamed Abdel-Wahab and colleagues, is a subgroup analysis of the PREPARE-CALC trial, which previously demonstrated superiority for a strategy of lesion preparation with rotational atherectomy prior to drug-eluting stent implantation compared to a modified balloon angioplasty strategy. This substudy clarifies those findings by suggesting that lesions located in the left anterior descending may be equally well treated with an initial strategy of rotational atherectomy or modified balloon angioplasty, whereas other lesion locations may favour a strategy of rotational atherectomy upfront. Another popular atherectomy modality, particularly in the USA, is orbital atherectomy, which − as with any intervention − needs ongoing surveillance of safety profiles, patient outcomes, and failure modes. Nauman Khalid, Ron Waksman and colleagues analysed post-marketing surveillance data from the US Food and Drug Administration Manufacturer and User Facility Device Experience (MAUDE) database, with a focus on safety profiles, patient outcomes, and failure modes for orbital atherectomy devices. A study where percentages represent the proportion of total submitted reports cannot really tell us about the incidence of complications with this technique. However, it highlights that such complications exist and are important, including vascular complications (perforation and dissection), arrhythmias, and death. The most commonly reported failure modes included detachment and/or structural damage of the device component, and device entrapment. The findings of this study may serve as an important platform for both manufacturers and clinicians to improve device performance and physician training, respectively.
Along the lines of percutaneous interventions for challenging lesions, three more studies tackle the issue of in-stent restenosis and stent thrombosis. In AGENT-ISR, Christian W. Hamm, Holger Nef and colleagues randomised a total of 125 patients with in-stent restenosis of a previously treated lesion <28 mm in length to two different drug-coated balloons. The study, accompanied by an editorial from Bruno Scheller, was designed for demonstrating the non-inferiority of the Agent balloon to the SeQuent Please balloon for 6-month in-stent late lumen loss. In another study, Dong Yin, Akiko Maehara and colleagues used optical coherence tomography to investigate the morphological characteristics associated with underexpansion of a newly implanted stent used to treat in-stent restenosis. This is a must-read to understand how, when re-stenting a restenotic lesion, factors such as old stent underexpansion, the amount of neointima or peri-stent calcium, and multiple old stent strut layers are important determinants of new stent underexpansion that is then associated with adverse long-term outcomes. Finally, Maria N. Tovar Forero, Joost Daemen and colleagues investigated the incidence and predictors of adverse cardiac events after treatment of a definite stent thrombosis. This is an interesting insight into the outcomes of such a complication, on quite large numbers, as the authors included all first definite stent thrombosis cases from 1996 to 2017 (695 cases). At 60 months, the cumulative incidence of major adverse events was 43.7%, but you will have to read the article to get more information, particularly on strategies that were found to be effective in improving the outcomes of patients experiencing a first thrombosis. The study is accompanied by an editorial from Giulio Stefanini.
Finally, in the section on interventions for valvular disease and heart failure, a study from Hernan Mejia-Renteria, Javier Escaned and colleagues provides new evidence on the diagnostic performance of quantitative flow ratio, using fractional flow reserve as a reference, in 115 patients with concomitant severe aortic stenosis awaiting TAVI, accompanied by an editorial from Niels Johnson. Compared with fractional flow reserve, angiography-based functional assessment demonstrated good diagnostic characteristics, which were superior to coronary angiography in assessing the functional relevance of coronary lesions in this particular subset. Another study from Tarun Chakravarty, Raj R. Makkar and colleagues assessed the safety and explored the efficacy of multivessel intracoronary infusion of allogeneic cardiosphere-derived cells in patients with advanced heart failure and reduced ejection fraction. The principal finding of this pilot trial concerns feasibility and safety, but there were also encouraging and concordant efficacy signals, especially evident at 6 months. The next step should be to proceed to a randomised, placebo-controlled trial.
This and much more is what we have in store for you in the July issue of the Journal. As the summer season comes alive, we hope you can find the time and desire to let us know your opinions, suggestions and reactions, on the website or through social media, to what you read here.
Supplementary data
To read the full content of this article, please download the PDF.