Abstract
Aims: Despite the widespread use of the radial approach in coronary interventions, left ventricular endomyocardial biopsy (LV-EMB) is most frequently performed via the femoral artery. We sought to assess the feasibility and safety of radial compared to femoral access in a large cohort of patients undergoing LV-EMB.
Methods and results: Data from 264 patients who underwent LV-EMB in Germany, Portugal, Japan and Canada were collected. Clinical, procedural, safety and feasibility data were evaluated and compared between the two groups. LV-EMB was successfully performed by the radial approach in 129 (99%) of 130 and in 134 (100%) patients by the femoral access. Patients in the radial group were older (mean age 55.7 versus 44.3 years) and were more likely to have moderate-severe mitral regurgitation (27.7% versus TF 0%). Sheathless guides were used in 108 (83.1%) of the radial and 2 (1.5%) of the femoral patients, so the mean guiding catheter size (radial 7.0±1.0 Fr versus femoral 8.0±0.0 Fr) was significantly smaller in the radial group (p<0.001). Mild or moderate radial artery spasm occurred in 13 (10.0%) patients but only one (0.8%) patient required conversion to femoral access due to severe spasm. No access site-related complications were reported in the radial group, while 11 (8.2%) patients in the femoral group had access-site haematomas (p=0.001). There were no major complications (mitral valve injury, pericardial tamponade requiring intervention, cerebrovascular accidents, persistent high-degree atrioventricular block, major bleeding or death) in either group.
Conclusions: The radial approach for LV-EMB appears to be safe and associated with a high success rate while possibly leading to fewer access-site bleeding complications compared to the femoral access. The results of this international multicentre study support the radial approach for LV-EMB and further inspire the expansion of “radial first” in the field of interventional cardiology.
Introduction
Endomyocardial biopsy (EMB) is most frequently undertaken from the right ventricle (RV). Left ventricular EMB (LV-EMB) is less often performed, possibly due to anecdotal concerns regarding safety. However, observational data have shown that LV-EMB is equally safe as compared to RV-EMB1,2. Furthermore, in conditions where the non-invasive investigations show a predominant pathological involvement of the left ventricle (LV), LV-EMB provides a higher diagnostic yield compared to RV-EMB2,3.
LV-EMB has traditionally been performed via the femoral approach, but recent small observational studies4,5,6 have shown that transradial LV-EMB is feasible and safe. Lower profile bioptomes along with the advent of sheathless guide catheters have allowed the performance of transradial LV-EMB. It is known that the transradial approach for percutaneous coronary intervention (PCI) improves bleeding outcomes which further translates into mortality benefit as compared to the transfemoral approach and across a broad spectrum of presentations7,8,9,10. However, whether the benefits seen in coronary interventions translate to LV-EMB is, at present, unknown. Although LV-EMB can be performed using similar equipment to that used for PCI, there are certain differences between the two procedures. These include the use of larger sheaths and guides with transfemoral LV-EMB, whereas performing transradial LV-EMB usually requires smaller outer diameter sheaths or sheathless guide catheters as compared to in patients undergoing routine PCI. Therefore, we sought to assess the safety, feasibility and procedural outcomes of radial compared to femoral approaches for LV-EMB in a multicentre study.
Methods
STUDY POPULATION AND OUTCOME DEFINITIONS
This is a multicentre, international registry of patients undergoing LV-EMB via the radial or femoral access in Canada, Germany, Japan, and Portugal. Data were gathered prospectively in local databases and then analysed centrally (T. Choudhury and R. Bagur). Data were collected using electronic and paper health records on multiple variables including, but not limited to, demographics and baseline clinical data, access route, and procedural characteristics (including sheath, guiding catheter and bioptome size along with haemostasis management). Procedure-related complications occurring in the periprocedural period were recorded. Major complications were defined as pericardial tamponade requiring intervention, cerebrovascular accidents, persistent high-degree atrioventricular block, mitral valve injury, major bleeding defined as per Bleeding Academic Research Consortium (BARC) definitions11 or death. All access site-related complications were recorded. The Early Discharge After Transradial Stenting of Coronary Arteries (EASY) scale was used to grade wrist haematomas: grade I (up to 5 cm), grade II (up to 10 cm), and grade III (>10 cm)12. Femoral haematomas were likewise graded using the EASY scale. The incidence of pseudoaneurysms and retroperitoneal haemorrhage was also recorded. Procedural success was defined as the completion of the EMB via the intended access route along with obtainment of number and quality of samples deemed satisfactory for pathological analysis. The study was in accordance with local ethics standards at each participating institution and informed consent was obtained for the procedure.
LEFT VENTRICULAR ENDOMYOCARDIAL BIOPSY: TECHNICAL ASPECTS
All procedures were performed by experienced radial and femoral operators who were well versed in performing both RV-EMB and LV-EMB. The choice of access site was not influenced by the indication for LV-EMB but rather by the overall centre experience, expertise and access route of preference of the operator. The decision to perform LV-EMB instead of RV-EMB was based on clinical and non-invasive assessment. LV-EMB was preferred where the pathological involvement predominantly involved or was suspected to involve the LV on non-invasive studies and/or clinical assessment. The radial LV-EMB procedure has been previously described4,5,13. Briefly, transradial LV-EMB can be performed using a standard sheath or a sheathless guide (Eaucath; Asahi Intecc, Aichi, Japan). The sheath (if used) and guide catheter size depends on the outer diameter of the bioptome. The bioptome is the same type and length required for femoral RV-EMB. For transradial LV-EMB, the use of sheathless guides is preferred in view of the smaller outer diameter for the same inner diameter as compared to sheaths. For instance, 6.5 Fr or 7.5 Fr sheathless Judkins Right or Multipurpose guides are most commonly used due to their shape that follows the long axis of the LV cavity. After radial access is gained, the sheathless guide mounted on its dilator is advanced over a 0.035” guidewire under fluoroscopy guidance up to the ascending aorta, where the dilator is then removed. Intravenous heparin is recommended to reduce the risk of systemic embolisation and is administered as per standard practice to prevent radial artery occlusion (RAO); doses were left to the operator’s discretion.
Transfemoral access for LV-EMB was performed under fluoroscopic guidance, in an anteroposterior view, and using a radiopaque marker placed at the femoral head level as landmark. Once access has been gained, the guiding catheter is advanced over a 0.035” wire under fluoroscopy guidance up to the ascending aorta. The remainder of the procedure is as described below.
A pigtail catheter can be inserted into the guide catheter for additional safety and used to cross the aortic valve, thereby positioning the guide catheter in the mid LV cavity, then the pigtail catheter is removed. The position of the guide catheter is confirmed in orthogonal views (i.e., right anterior oblique 30-45º and left anterior oblique 30-45º). A Y-type haemostatic valve is connected to the guide catheter, and thorough flushing with saline is performed after connection to a conventional manifold. A bioptome is advanced into the LV through the haemostatic valve and guide catheter. Bioptome size is usually 5.5 Fr, although smaller sized bioptomes (3 Fr) are also available. Samples are then obtained. Importantly, repetitive bleed-back and manual flushing are strongly advised to avoid air embolisation during each sample extraction and bioptome re-insertion. Following completion of a transradial LV-EMB, a radial haemostatic band is positioned over the radial access site, the guide catheter is removed over the 0.035” guidewire and, at this point, the haemostatic band is adjusted to the wrist4,5,13. For transfemoral LV-EMB, manual pressure or a vascular closure device is employed to achieve haemostasis.
STATISTICAL ANALYSIS
Continuous variables are expressed as mean±standard deviation, and categorical variables are expressed as n (%). Comparison of continuous variables was performed using the Student’s t-test, and categorical variables were compared using the chi-square test. All statistical tests were two-tailed, and differences were considered statistically significant when a p-value was <0.05. Data analyses were performed using the Statistical Package for Social Sciences (SPSS), Version 24 (IBM Corp., Armonk, NY, USA).
Results
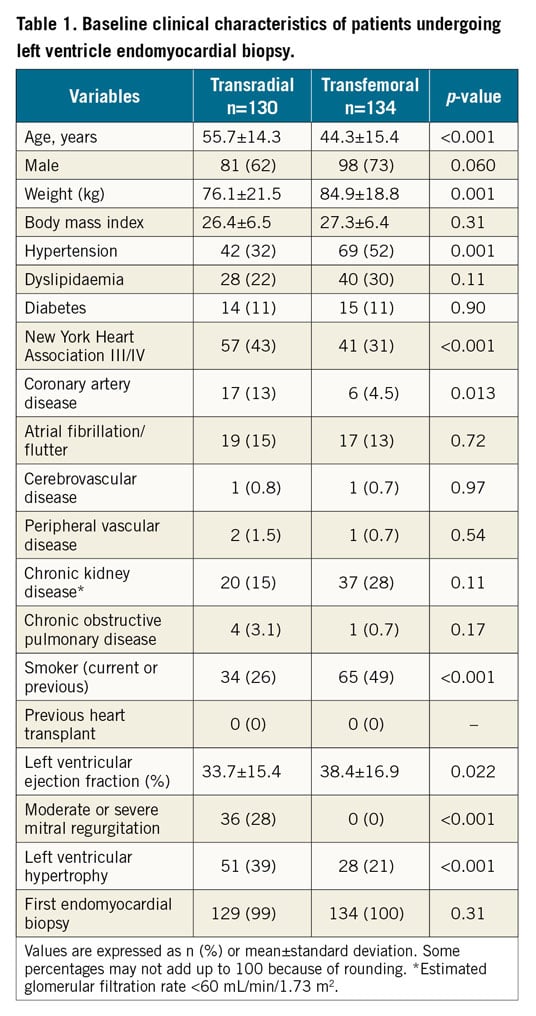
POPULATION AND PREPROCEDURAL CHARACTERISTICS
A total of 264 patients underwent LV-EMB. Of these procedures, 130 (49.2%) were performed through the radial and 134 (50.8%) through the femoral access. Patients in the radial group were significantly older (55.7±14.3 versus 44.3±15.4 years, p<0.001) and had a lower mean left ventricular ejection fraction (33.7±15.4% versus 38.4±16.9%, p=0.02) compared to the femoral group. More patients in the radial group presented with New York Heart Association Class III/IV (43.8% versus 30.6%, p<0.001). All patients had LV-EMB for the first time (except one patient in the transradial group). In the transradial group, the most common indications for LV-EMB were dilated cardiomyopathy (30.5%), infiltrative cardiomyopathy (21.1%) and myocarditis (14.1%), whereas in the transfemoral group it was myocarditis. Relevant patient demographics and baseline clinical characteristics are detailed in Table 1.
ACCESS, SHEATH AND GUIDE CATHETERS
Intravenous heparin was administered in 124 (95.4%, mean 4,252±1,104 IU) patients in the radial group and none in the femoral group. Mild or moderate radial artery spasm occurred in 13 (10.0%) patients, and one (0.8%) patient required crossover to femoral access due to severe spasm.
In the radial group, 22 (16.9%) patients had sheaths inserted while the remainder (n=108; 83.1%) underwent LV-EMB via a sheathless guide. In the femoral group, 132 (98.5%) patients had sheaths inserted (all 8 Fr) while two patients had LV-EMB via a sheathless guide (both 7.5 Fr). Sheath size was significantly smaller in the radial group (radial 5.1±0.2 Fr versus TF 8.0±0.0 Fr, p<0.001). The majority of sheathless guide catheters were 7.5 Fr (n=93/110; 84.5%); therefore, the mean guide catheter size was significantly smaller in the radial group (radial 7.0±1.0 Fr versus femoral 8.0±0.1 Fr, p<0.001). Table 2 shows the procedural data.
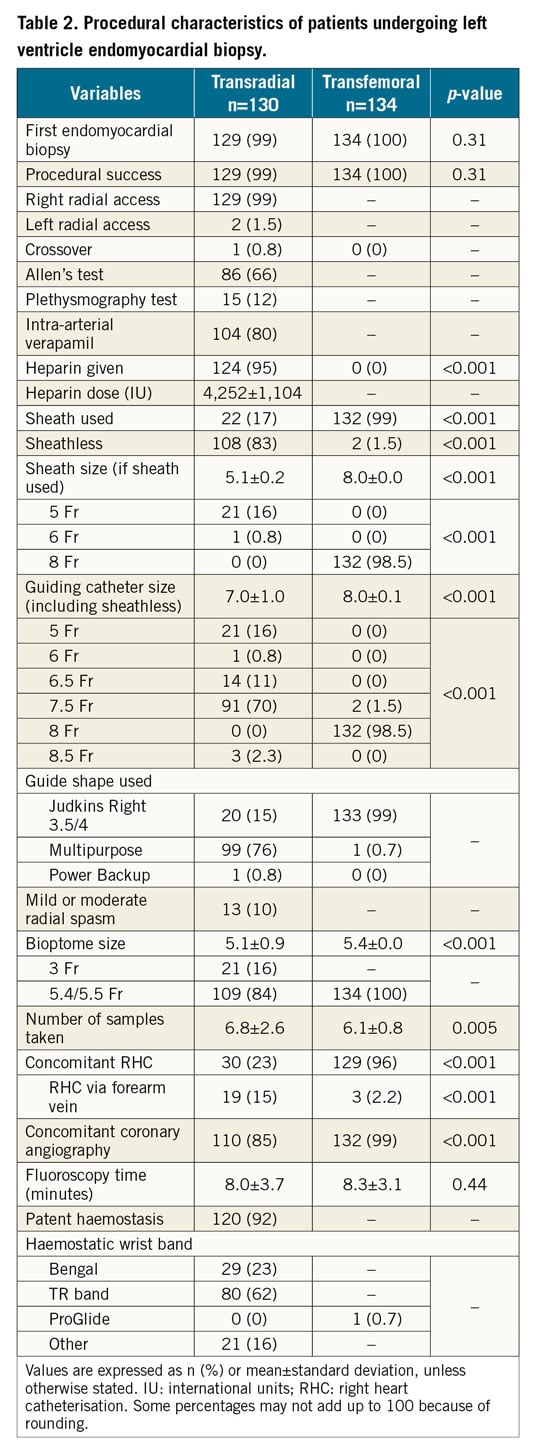
LEFT VENTRICULAR ENDOMYOCARDIAL BIOPSY
The procedural success rate was 99% (129 of 130 patients) in the transradial group and 100% in the transfemoral group (p=0.31). In radial patients, 5.5 Fr (84%) and 3 Fr (16%) bioptomes were used whereas all femoral patients had 5.4 Fr bioptomes. The radial group had a higher number of samples obtained per LV-EMB as compared to the femoral group (6.8±2.6 versus 6.1±0.8, p=0.005). Samples obtained were quantitatively and qualitatively suitable for pathological analysis in all patients and in both groups. The fluoroscopy times were similar in the two groups (TR 8.0±3.7 versus TF 8.3±3.1 minutes, p=0.44).
In the radial group, the most common pathology diagnoses were myocarditis (20.8%), idiopathic dilated cardiomyopathy (19.2%), and amyloidosis (13.1%). In the femoral group, the most common pathology diagnoses were myocarditis (70.9%), idiopathic dilated cardiomyopathy (14.2%) and persistent chronic viral infection (9.7%).
CONCOMITANT CORONARY ANGIOGRAPHY AND RIGHT HEART CATHETERISATION
A total of 110 (84.6%) patients in the radial group and 132 (98.5%) patients in the femoral group underwent concomitant coronary angiography (Table 2). Thirty (23.1%) patients in the radial group underwent concomitant right heart catheterisation (RHC), 19 (63%) of them through a forearm vein. In the femoral group, 129 (96.3%) patients underwent concomitant RHC, and only 3 (2.3%) of these had RHC through a forearm vein.
POST-PROCEDURAL MANAGEMENT
Patent haemostasis was achieved in 120 patients (92.3%) in the transradial group (Table 2). The TR Band® (Terumo Corp., Tokyo, Japan) was used in 80 (61.5%) patients and the Bengal™ Radial Compression Band (Ates Group, St-Bruno, QC, Canada) in 29 (22.3%) patients. In the transfemoral group, haemostasis was achieved using manual pressure and compression bandage in all patients except for one, who had a suture-mediated vascular closure device (ProGlide®; Abbott Vascular, Santa Clara, CA, USA).
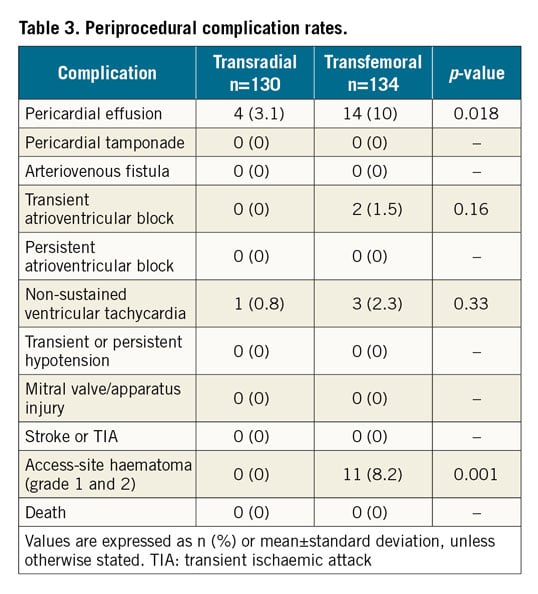
PERIPROCEDURAL COMPLICATIONS
There were no major complications in either group. Access site-related haematoma occurred in 11 (8.2%) patients in the transfemoral group and in no patients in the transradial group (p=0.001). Of the 11 femoral access patients, 9 had grade 2, and 2 had grade 1 haematomas. No retroperitoneal bleeds or pseudoaneurysms were reported. Pericardial effusion was noted in 4 transradial and 14 transfemoral patients. None of the pericardial effusions was haemodynamically significant to require any form of intervention. Two patients in the femoral group developed transient high-degree atrioventricular block, but no pacing was required. Non-sustained ventricular tachycardia was observed in 1 (0.8%) patient in the transradial group and 3 (2.3%) patients in the transfemoral group (p=0.33). Table 3 shows detailed procedure-related complications.
Discussion
The results of this study including 264 patients undergoing LV-EMB show that the radial approach is feasible and safe, achieving similar high procedural success rates whilst it appears to be associated with fewer access site-related bleeding complications as compared to the femoral route.
The safety of LV-EMB has already been demonstrated in reports comparing LV-EMB versus RV-EMB1,2,3 using the femoral artery and vein routes. Yilmaz et al1 showed a higher rate of minor complications in the LV-EMB group as compared to the RV-EMB group; however, the authors found similar, low rates of major complications including haemopericardium requiring pericardiocentesis and stroke (0.32% each). Chimenti et al2 reported data on patients undergoing transfemoral LV-EMB and noted a 0.08% rate of cardiac perforation and tamponade, a 0.22% rate of transient cerebral ischaemia and no deaths. The authors also reported more frequent local complications (access-site haematoma) or vasovagal reaction during LV-EMB compared to RV-EMB2. Conversely, Stiermaier et al3 showed one major complication, a pericardial tamponade requiring surgical revision during RV-EMB, whereas no severe complications occurred during LV-EMB.
Notably, data on transradial LV-EMB are still scant. Previous case series have shown an absence of major complications during the procedures5,6, and very low rates of minor complications, yet with small sample sizes. In the present study, we show a very low rate of complications using either transradial or transfemoral access. To the best of our knowledge, we are the first to compare the transradial and transfemoral approaches for LV-EMB, and further confirm the safety profile of the transradial approach in terms of lowering access site-related bleeding complications.
A recent study14 showed that, over a 12-year period, more than 70,000 EMB were performed in the USA; thus this number is certainly much larger worldwide. While the vast majority of these procedures are likely to be RV-EMB (site of EMB not specified in study), the already known equivalent safety of RV-EMB and transfemoral LV-EMB1,2 may potentially increase the adoption of LV-EMB into clinical practice. Hence, extrapolating these findings to a larger population, it suggests a fairly sizeable composite risk of major and minor complications with the femoral access for LV-EMB and therefore raises the question of whether the radial approach would contribute to further minimisation of this risk.
ACCESS SITE, CATHETERS AND CONCOMITANT PROCEDURES
The choice of the initial access site for LV-EMB directly influences the access for concomitant coronary angiography and/or RHC, as seen in the present study. Previous studies in the coronary setting have evaluated the frequency of access-site crossovers. Importantly, the main reasons for conversion from radial to femoral are usually failure to obtain access/significant radial artery spasm, or forearm and subclavian tortuosity. Our crossover rate from transradial to transfemoral was only 0.8%, and was secondary to severe radial spasm. We observed mild or moderate radial spasm in 10% of patients, but this can be easily overcome in most cases with intra-arterial vasodilators. Furthermore, sizing of the radial artery using ultrasound guidance might help to reduce the chances of radial spasm further.
The sheath (when used) and guiding catheter sizes were significantly smaller in the radial group compared to the femoral group, thus allowing the procedure to be performed via smaller sized arteries. Smaller sheath size has been shown to be an independent predictor of access site-related bleeding and RAO complications in transradial coronary interventions15. Importantly, sheath and guiding catheter size is not a limiting factor for transradial LV-EMB with the advent of smaller profile bioptomes and sheathless guides. Indeed, 84% of the transradial LV-EMBs were performed with a 5.5 Fr bioptome, a slightly larger size compared to the femoral group (5.4 Fr). Sheathless guides have overcome the “working space advantage” of femoral access. For instance, a 7.5 Fr sheathless guide has a 2.49 mm external diameter and 2.05 mm internal diameter, allowing the passage of a 5.5 Fr (1.85 mm shaft outer diameter) biopsy forceps. Moreover, the outer diameter of a 7.5 Fr sheathless guide is smaller than a standard 6 Fr sheath (2.70 mm). In addition, smaller-sized (3 Fr) bioptomes have allowed LV-EMB via 5 Fr sheaths in 16% of our radial patients.
These data are also relevant for those patients undergoing concomitant coronary angiography, RHC, and EMB, since the three procedures can be performed via the radial artery and forearm vein, providing a “one-stop shop” to perform these procedures through the arm at a lower bleeding risk. Patients undergoing coronary angiography can have their angiography carried out using 5 Fr catheters, and then have the radial sheath exchanged for a 6.5 Fr or 7.5 Fr sheathless guide catheter for performing LV-EMB. Even though we found that transfemoral patients had more concomitant RHCs and angiograms, transradial patients had more samples taken. Thus, the fluoroscopy times were comparable between the groups.
BLEEDING RISK, HAEMOSTASIS, AND POST-PROCEDURAL CARE
The radial artery is a superficial artery that can be easily compressed. Liberal compression can be applied along the distal forearm to achieve haemostasis. In our study, the transfemoral group had a significant number of patients with access-site haematoma (EASY grade 1 and 2, 8.2%), whereas none of the transradial patients had any access-site bleeding complications. Notably, although 98.5% of patients undergoing transfemoral LV-EMB received 8 Fr sheaths, they did not systematically receive IV heparin, while almost all transradial patients did. Although manual compression was used in the majority of patients in the femoral group, and a vascular closure device was used in one patient only, this is unlikely to influence the rate of access site-related complications in the femoral group, as manual compression and closure devices have been shown to be comparable in terms of safety16. Our findings build upon the evidence base for the well-known reduction in access-related risk of bleeding using the transradial approach, now applied to the setting of LV-EMB. Moreover, elective patients undergoing transradial LV-EMB can be mobilised earlier, and thus potentially be discharged more quickly17.
Importantly, one of the limitations of the transradial route might be the need for repeat EMB (i.e., heart transplant patients needing surveillance EMB). Repeat procedures via the same radial artery are both feasible and safe. However, the rate of RAO may increase with successive procedures18,19. Intravenous heparin 50 U/kg along with patent haemostasis and shortened compression time (i.e., 60 minutes) protocols significantly reduce the incidence of RAO20,21. In our series, intravenous heparin was administered in 95% of the patients and patent haemostasis was achieved in the majority (92%) of them. Notably, although the risk of ventricular perforation is rare, and even more with LV-EMB as compared to RV-EMB2,3, heparin can be rapidly reversed with protamine.
Limitations
The main limitation of this study lies in its non-randomised nature and the inherent risk of selection bias encountered in these study populations. Another limitation of this study is that ultrasound guidance was not systematically used to identify the bifurcation of the common femoral artery while obtaining femoral access. As mentioned above, almost all patients in the transfemoral group had 8 Fr sheaths and guides, therefore precluding a head-to-head comparison in terms of sheath size. Despite this limitation, the risk of access-site complications is likely to be influenced by a balance of factors such as sheath size, arterial access and haemostasis techniques and also the use of heparin. Nonetheless, our study shows a real-world population comparing current practices of radial and femoral access for LV-EMB. A potential limitation with the use of 3 Fr bioptomes is the likelihood of obtaining smaller sample sizes and hence non-diagnostic EMB. However, this was not the case in any of the 21 patients undergoing LV-EMB using 3 Fr bioptomes, highlighting the importance of the technique rather than the actual bioptome size. Radial artery patency was not systematically assessed using the reverse Barbeau test and/or colour Doppler ultrasound; however, these data reflect daily real-world practice and are not dissimilar to the coronary practice where radial artery patency is not routinely assessed prior to hospital discharge. Although randomised controlled trials may help to determine the superiority or non-inferiority of either access for LV-EMB, these might be difficult to undertake. These results should be validated and supported by future, larger-scale studies. Meanwhile, in the absence of definitive evidence, the well-established benefits of the radial access in minimising vascular and bleeding complications may also apply to patients undergoing LV-EMB.
Conclusions
The radial approach for LV-EMB appears to be safe and associated with a high success rate while possibly leading to fewer access-site bleeding complications compared to the femoral access. The results of this multicentre international study support the radial approach for LV-EMB and further inspire its expansion in the field of interventional cardiology. Moreover, the conversion to a “radial first” access strategy could also be encouraged for invasive cardiologists, without interventional training, performing diagnostic procedures and EMB.
|
Impact on daily practice Left ventricular endomyocardial biopsy (LV-EMB) appears to be as safe as right ventricular endomyocardial biopsy. The transradial approach for LV-EMB is associated with a high success rate in patients undergoing native LV-EMB, while possibly leading to fewer access-site bleeding complications compared to the femoral access. Transradial access is associated with the use of smaller sheaths, guiding catheters and bioptomes. The results of this multicentre international study further inspire the expansion of “radial first” in the field of interventional cardiology. |
Conflict of interest statement
The authors have no conflicts of interest to declare.