Abstract
Aims: Endomyocardial biopsies (EMBs) are performed infrequently in children owing to significant past complication rates and controversial discussions about the therapeutic value of results. The objective of this study was to investigate the safety and feasibility of EMBs for suspected myocardial disease in relation to their clinical value.
Methods and results: We performed a retrospective multicentre review of the Working Group for Interventional Cardiology of the German Society for Paediatric Cardiology. During three consecutive years, 206 EMBs (84 female/mean age 8.95±6.62 years) were performed and analysed at 15 heart centres. In the majority of cases, biopsies were taken from the right ventricle (RV/89.8%; p<0.001). The overall complication rate was 9.7%, whereas major complications occurred in only 0.97% of cases. Risk factors associated with a higher complication rate were biopsy during the first year of life (20.5%) and from the left ventricle (31.1%) (p<0.05). There was no procedure-related mortality. Treatment was changed in 18.0% of cases based on biopsy results.
Conclusions: Today, endomyocardial biopsies in older children with suspected myocardial disease can be performed safely with a low risk of major complications and mortality, whereas the risk of complications if the biopsy is carried out in the first year of life or taken from the left ventricle remains high.
Abbreviations
DCM: dilative cardiomyopathy
EMB: endomyocardial biopsy
Introduction
Since the introduction of catheter-based endomyocardial biopsies (EMBs) in 1962 by Sekiguchi and Konno1, endomyocardial biopsy (EMB) has become a valuable diagnostic tool for the evaluation of myocardial tissue from suspected cardiomyopathy, myocarditis, cardiac tumour or different types of cardiac involvement in systemic diseases2. Owing to the development of histological and molecular diagnosis, immunohistochemistry, in situ hybridisation and polymerase chain reaction informative values have improved significantly. Analysis of myocardial tissue for the confirmation of diagnosis has become the gold standard in different myocardial diseases and is of great importance, especially in rare myocardial disorders, where non-invasive tools might miss the diagnosis. New potential treatments for specific myocardial diseases on the basis of EMB results highlight the therapeutic value of this procedure3. Furthermore, EMB remains crucial in the care of children following cardiac transplantation despite reliable, non-invasive indices for rejection.
The benefits of EMB for children with suspected myocardial disease are controversial points of daily discussion. Reported complication rates vary from 0.1% to 15.5%, and mortality is reported in up to 1.7% of cases4-7. The complication rate in biopsies for myocardial disease is higher than that in biopsies for transplant rejection surveillance8. In some centres, EMB is thus performed infrequently in infants and small children for the diagnosis of myocardial diseases.
The right ventricular approach by the femoral or jugular vein has widespread acceptance, as the left ventricular approach involves more, and possibly severe, complications, although a biventricular approach may have some potential advantages9. With the development of dedicated flexible bioptomes available in small sizes, less is known currently about myocardial biopsy approaches and the risk of complications in children and adolescents.
The objective of this multicentre study was to investigate the actual safety and feasibility of EMBs in suspected myocardial diseases from neonatal ages to young adulthood and to assess the impact of the results on the subsequent clinical treatment.
Material and methods
This was a retrospective multicentre study organised by the Working Group for Interventional Cardiology of the German Society for Paediatric Cardiology. The analysis of EMBs in paediatric patients (<18 years) from 15 heart centres (Germany 12, Austria 2, Switzerland 1) was performed during three consecutive years. Cardiac catheterisation reports were analysed for EMBs in patients with clinically suspected myocardial disease. Patients who received a biopsy to monitor heart transplantation were not included in this study.
Each patient’s data were reviewed for gender, age at biopsy, first or repeated biopsy and their clinical status including inotropic support (catecholamine, milrinone or levosimendan) or ventilator support in case of haemodynamic or respiratory compromise due to cardiomyopathy before EMB. A clinical analysis was performed for the potential indications for EMB involving clinical scenarios when EMB should be taken, as recommended by the AHA and ESC and published by Cooper et al in 20073.
In addition, the ventricular chamber of the biopsy collection and the number of biopsies taken were evaluated for technical analyses of EMBs. Procedure-related complications were reviewed. Major complications were defined as death in relation to EMB, pericardial effusion requiring pericardiocentesis, brain or pulmonary embolisation and permanent complete atrioventricular block. Minor complications included transient conduction disturbances, vascular complications (e.g., massive haematoma, retroperitoneal bleeding and thrombosis), arrhythmias, tricuspid regurgitation due to EMBs from the right ventricle or aortic regurgitation due to EMBs from the left ventricle and pericardial effusion not requiring pericardiocentesis.
EMB histological results were grouped by cardiomyopathy type according to the recommendation by the AHA from 2006 reported by Maron et al10. In cases of infective myocarditis, the types of detected organism and inflammatory reaction (acute vs. chronic or healing myocarditis) were analysed. Non-infective reasons for myocarditis, such as post-viral autoimmune myocarditis, myocarditis in the case of systemic disease, giant cell myocarditis, eosinophilic myocarditis and further rare EMB results were evaluated.
Finally, specific treatment change or initiation due to EMB results, such as the initiation or cessation of antiviral therapy (e.g., IFN-beta, IFN-alpha), immunosuppressive therapy (e.g., corticosteroids, azathioprine, cyclosporine), immuno-adsorptive therapy, immunoglobulin therapy and specific antimicrobial therapy were analysed and observed in relation to indications, procedures and complication rates.
Statistical analysis
All data were analysed by a single investigator and expressed as mean±standard deviation or absolute numbers and percentages. Correlations of age, clinical status, indications and complications were performed via chi² tests. Binary logistic regression was used for identification of differences in study populations. All p-values were two-sided and we considered p-values <0.05 as being statistically significant. Microsoft Office Excel 2010 (Microsoft Corporation, Redmond, WA, USA) was used for collecting data. Analyses were performed using SPSS, Version 21.0 (IBM Corp., Armonk, NY, USA).
The study was registered, designed, performed and controlled according to the current guidelines of Good Clinical Practice, approved by the leading ethics committee at the Ärztekammer Hamburg and by other local committees. It complies with the Declaration of Helsinki.
Results
PATIENT CHARACTERISTICS
At 15 heart centres, 206 EMBs (84 female) were performed in 200 paediatric patients with suspected myocardial disease. Biopsies were taken at a mean age of 8.95±6.62 years (male 10.56±6.53 vs. female 7.55±6.30 years; p<0.001). The youngest patient had a biopsy performed at six days old, the oldest at the age of 18 years. In 39 patients (18.9%), biopsies were taken in the first year of life. Before EMB, 25.7% of patients required inotropic support. Respiratory support was present in 12.6% of cases (Table 1). In 88% of cases requiring respiratory support further inotropic support was needed.
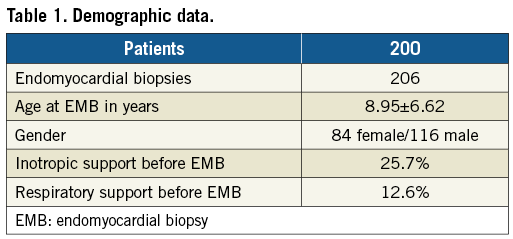
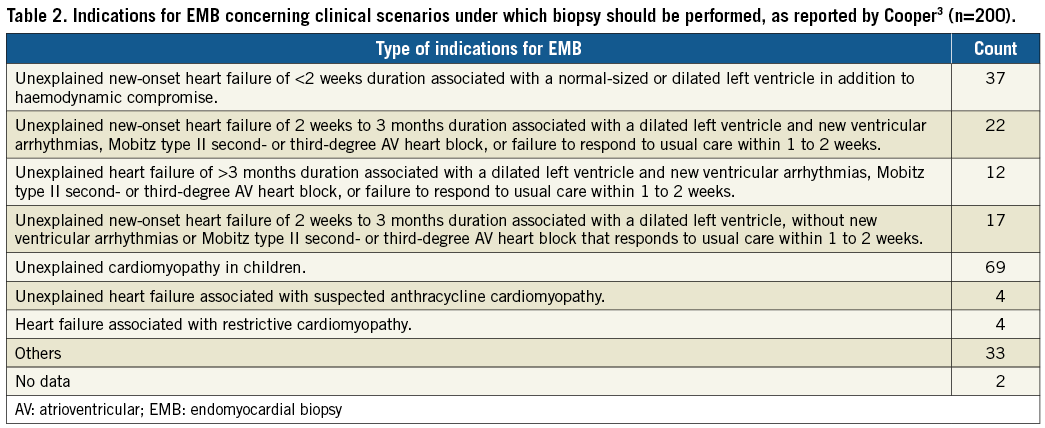
Types of indications were analysed in 198 patients. The most common indications for biopsy were unexplained cardiomyopathy in childhood in 69 patients and unexplained new-onset heart failure <2 weeks duration associated with a normal-sized or dilated left ventricle, and haemodynamic compromise in 37 cases (Table 2).
TECHNICAL ASPECTS OF EMB IN CHILDREN AND ADOLESCENTS
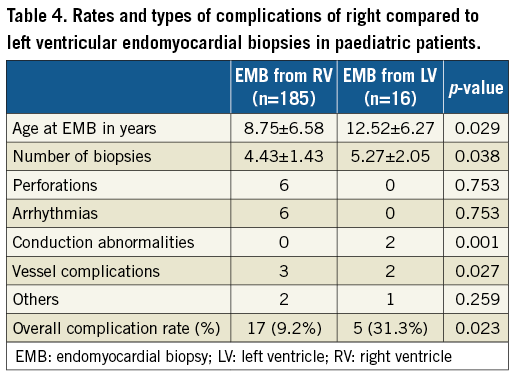
In the majority of the 206 cases analysed, the EMB was taken from the right ventricle (RV/89.8%; p<0.001). Biopsies from the left ventricle (LV) were performed in 7.5% and biventricular biopsies in only 0.5% of cases. In 2.2% of patients, no data about the ventricular chamber of the endomyocardial biopsy were available. Patients receiving a biopsy from the left ventricle were significantly older than children receiving a right heart biopsy (12.52±6.27 yrs vs. 8.75 ±6.58 yrs; p=0.029). Left ventricular biopsies were performed in only two centres in cases of patients with unexplained new-onset heart failure >2 weeks duration associated with a normal-sized or dilated LV in addition to haemodynamic compromise. The mean number of biopsies taken was 4.5±1.49. More biopsies were taken from the LV compared with the RV (LV 5.27±2.05 vs. RV 4.43±1.43; p=0.038). Biopsy count did not depend on indications for biopsy or age at biopsy.
COMPLICATIONS OF EMB
The overall complication rate from 206 EMBs in cases of suspected myocardial disease was 9.7% without gender-specific differences (male 8.0% vs. female 10.5%; not significant [ns]). Major complications (0.97%) included two cases of pericardial drainage in cases of pericardial effusion. However, no patient needed surgical treatment. There was no procedure-related death in this population.
Minor complications (8.7%) included arrhythmias in seven (3.4%), conduction anomalies in two (1.0%), vascular complications in five (2.4%) and pericardial effusion without drainage in four patients (1.9%). No patient needed permanent pacemaker therapy, medical antiarrhythmic or heart failure treatment and surgical or interventional procedures owing to EMB complications.
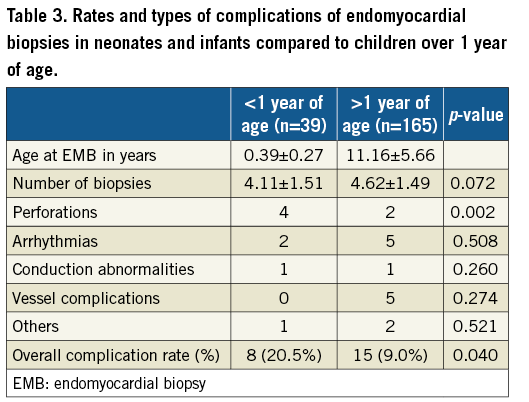
Age under one year at EMB was identified as a risk factor for complications. The complication rate in the first year of life was more than two times higher than that in later childhood and adolescence (p=0.04) (Table 3).
The complication rate of left ventricular biopsies was significantly higher compared with that in EMBs from the right ventricle (31.3% vs. 9.2%; p=0.023), whereas the type of complication after left ventricular biopsies was different to that following right heart biopsies. In left heart biopsies, vessel complications and conduction anomalies were found more often, whereas cardiac perforation and arrhythmias complicated right ventricular biopsies (Table 4). Indications for EMB or number of taken biopsies did not influence the complication rate (ns).
Interestingly, patients receiving inotropic support for haemodynamic compromise before EMB were younger than patients without. The rate of complications in critically ill patients treated with inotropes was however comparable to the rate of complications in untreated patients (ns). Respiratory support before EMB did not influence the complication rates (ns). Anaesthesia-related complications were not reported.
HISTOPATHOLOGICAL DIAGNOSES AND TREATMENT CONSEQUENCES
Histopathological and molecular analyses were performed mostly in the Department of Molecular Pathology at the University Hospital of Tübingen, Germany. The results of 197 histopathological findings classified according to the AHA classification for cardiomyopathies published by Maron et al in 200610 are reported in Figure 1. Inflammatory cardiomyopathies were most common in this population and significantly more frequent in male patients (male 72.2% vs. female 27.8%; p<0.001). Analysed cases of inflammatory cardiomyopathies revealed signs of active myocarditis in 40.9% of patients versus signs of chronic myocarditis in 59.1%. Polymerase chain reaction analysis detected viral genomes in 30.1% of patients with inflammatory cardiomyopathy. Parvovirus B19 was detected in 66.1%, HHV-6 in 29%, HHV-7 in 3.2% and enterovirus in 1.6% of patients. Bacterial infection was suspected in one patient. Fungi or protozoans did not appear. Non-infective myocarditis was found in nine cases (4.4%). Diagnosis of inflammatory cardiomyopathy led to treatment change in 24.7% of patients.
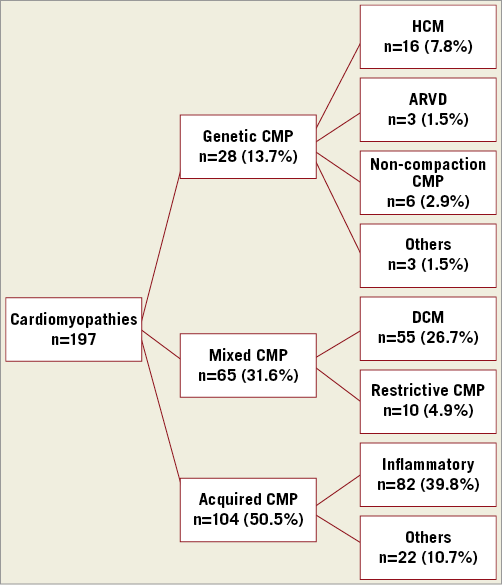
Figure 1. Distribution of histopathological findings referring to AHA classification reported by Maron in 200610. ARVD: arrhythmogenic right ventricular dysplasia; CMP: cardiomyopathy; DCM: dilative cardiomyopathy; HCM: hypertrophic cardiomyopathy
Dilative cardiomyopathies (DCM) were the second largest group and significantly more common in female patients (female 64.7% vs. male 35.3%; p<0.001). Treatment strategy was changed in 18.9% due to diagnosis of DCM. Other cardiomyopathies were diagnosed less frequently with no differences in gender distribution.
Overall, histopathological findings, immunohistochemistry, and polymerase chain reaction analysis led to treatment changes in 18.0% (n=37) of patients. Treatment changes due to EMB results varied significantly due to different diagnoses and clinical settings. Immunoglobulins were started in nine cases and stopped in seven; anti-inflammatory therapy was stopped in one case and started in one; antiviral treatment was stopped in five cases and antimicrobial therapy started in two and ceased in another. Two patients received modification of medical treatment for heart failure. One patient received a wearable cardioverter defibrillator in case of significant ventricular arrhythmias and histopathological diagnosis of acute myocarditis. Another patient received a pacemaker due to histopathological diagnosis of arrhythmogenic right ventricular dysplasia. Six patients were listed for cardiac transplantation after secured diagnosis of dilative cardiomyopathy, acute myocarditis and hypertrophic cardiomyopathy. One patient was transferred for mitral valve surgery after exclusion of acute myocarditis.
EMBs from the left ventricle and during the first year of life were identified as high-risk EMBs. For a better understanding as to whether EMBs in these high-risk groups are meaningful, treatment changes following EMB results in these subgroups were analysed. Rates of treatment change in the first year of life were not different to those following EMBs at older ages (ns). Concerning the ventricular side of the biopsy, all treatment changes were based on right ventricular EMBs; no high-risk left ventricular biopsy led to treatment change in this paediatric population (p=0.033).
Discussion
This study reports on the actual safety and feasibility of EMBs in paediatric patients with suspected myocardial diseases in a high number of heart centres in Germany, Austria and Switzerland. A total of 200 patients had a biopsy in a three-year period in 15 heart centres. An average of 4.4 EMB procedures per centre and year in cases of suspected myocardial disease in childhood demonstrate that EMB in paediatric patients is still not a commonly used diagnostic tool. Previous studies including post-transplant surveillance report a range of 2.3-15.4 biopsied patients per centre and year8,11,12.
EMBs are the gold standard for the diagnosis of myocardial diseases but less is known about the exact timing of EMB for a definitive diagnosis13. The most common reasons for biopsy were unclear cardiomyopathy, and unexplained heart failure with a dilated left ventricle in this population of paediatric patients. Comparable data for indications of EMB in paediatric patients with suspected myocardial disease in particular are very rare.
TECHNICAL ASPECTS
One of the diagnostic limitations of EMBs is the selective ventricular approach. The diagnostic yield of EMB may be optimised when samples from both ventricles are available8. In adult patients, EMBs from the left ventricle are known to be safe and of higher diagnostic yield compared with EMBs from the RV2; however, the left ventricular approach has not yet gained widespread acceptance due to concerns about more severe potential complications.
In this multicentre study of paediatric patients with suspected myocardial disease, EMBs were mostly taken from the right ventricle. Left ventricular approaches were used in only a few cases. These data correspond to previous reports about EMB in children8,12.
COMPLICATIONS
The risks, especially of major complications and mortality, of EMB in childhood remain a controversial point in the discussion about the time, location and indications for EMBs. Lower complication rates were found in heart transplant recipients compared with those for myocarditis8,12.
Complication rates are higher in children compared with adults, even in heart transplant recipients with low complication rates after EMB14. In our cohort, younger age could be identified as a risk factor for complications due to EMBs. In infants, the risk of complications was more than two times higher than that for older children and adolescents (overall complication rate: <1 year of age 20.5% vs. >1 year of age 9%; p<0.04).
Major complications and mortality during EMBs have been reported previously. This is one of the reasons for the discussion in terms of the benefit-to-risk profile of EMBs in suspected myocardial diseases during childhood7,8. In our cohort, however, no mortality occurred in 15 heart centres within a three-year period. Major complications appeared in only two patients (0.97%). Minor complications were found in 8.7% of patients. Ventricular perforation due to endomyocardial biopsies is of special interest because of the potential mortality risk. A higher incidence of perforation in patients being evaluated for myocarditis compared with post-cardiac transplantation is known (5.2% vs. 0.1%) from previous studies12. In this population, the perforation rate was 2.9% with a significantly higher perforation incidence in infants. All perforations occurred within the right ventricle. Small ventricular anatomy as well as thin right ventricular and structurally altered myocardium (by the acute inflammation and oedema) may be reasons for the greater perforation rate in this population. Relevant clinical deterioration due to myocardial perforation of the right ventricle did not occur within this evaluation.
Rhythm disturbances such as supraventricular and ventricular tachycardia appeared in 3.4% of EMBs. One patient required cardioversion owing to supraventricular tachycardia. Temporary conduction anomalies with 2:1 atrioventricular block and complete heart block occurred in two patients without the need for pacemaker treatment. Conduction anomalies appeared during left ventricular biopsies in this study population in contrast to previous reports4,9. Manipulation on the interventricular septum by a bioptome or catheter in smaller anatomy and smaller aortic arch angulation could be the reasons for conduction anomalies during left heart biopsies in this paediatric population.
Vascular complications such as massive haematoma, retroperitoneal bleeding and vessel thrombosis were found in five patients with a mean age of 13.28±3.5 years. Previously reported complications such as embolism, coronary fistula, and ruptured tendineae of the tricuspid valve or pneumothorax were not found in this three-year period in 15 heart centres15,16.
In this population, a number of critically ill children supported by inotropes and respiratory support received EMBs. Contrary to results from previous studies, treatment by inotropes or respiratory support did not influence the risk of complications in the present study12.
Left ventricular biopsies are common in adult patients with suspected myocardial disease. In our population, left ventricular biopsies were performed only in a minority of older children and adolescents. Children receiving left ventricular biopsies had higher overall complication rates with a preponderance of conduction anomalies and vessel complications. Left ventricular perforation did not occur. A lower perforation rate in the case of left ventricular biopsy was found in adult patients, but the mortality rate due to left ventricular perforation was significantly higher (12.9%) compared with RV perforation (5.2%)17. Brain embolisation as reported in adult patients with left ventricular biopsy did not occur in this paediatric population2.
HISTOLOGICAL RESULTS AND THERAPEUTIC CONSEQUENCES
The therapeutic relevance of biopsy results is a critical issue. Myocarditis studies have demonstrated no difference in long-term outcome regardless of the presence or absence of myocardial inflammation in patients with acute LV dysfunction18,19. In 2010, Foerster et al reported no difference in outcomes after biopsy-confirmed and probable myocarditis in children20. Nevertheless, biopsy results can help to bring a deeper understanding of the pathogenetic features of inflammatory cardiomyopathies in terms of fundamental differences, for example between a coxsackievirus-associated myocarditis and parvovirus B19 vasculitis-dependent cardiomyopathy taking into account prognostic as well as therapeutic differences21-23. Finally, the benefit of EMBs in rare cases such as eosinophilic myocarditis seems indisputable24. In this multicentre study, participating colleagues were asked for EMB results that corresponded to a change in current therapy. In 18% of patients the treatment was changed due to EMB results. The types of treatment change varied widely due to different clinical settings and diagnoses. The results regarding therapeutic consequences due to EMB results can only be landmarked in the wider field of cardiomyopathies and their treatment options.
Limitations
In this retrospective multicentre study, selection bias for EMB indication as well as potential treatment change had to be taken into consideration. Further, the different experience of examiners and different strategies for EMB procedures have to be noted. Although this multicentre study included 15 heart centres and a three-year period of evaluation, the limited number of EMBs performed has to be taken into account.
Conclusions
Today, endomyocardial biopsies in older children with suspected myocardial disease can be performed safely with a low risk of major complications and mortality, whereas the risk of complications of EMBs in the first year of life and from the left ventricle remains high. A diagnosis of inflammatory cardiomyopathies is the reason for treatment change in most cases following EMB results.
| Impact on daily practice This multicentre study from 15 heart centres demonstrates the actual feasibility, safety and impact of endomyocardial biopsies for the diagnosis of myocardial disease in children. These data are helpful for deciding for or against endomyocardial biopsies in children at times of controversial discussions about the benefits and risks of invasive procedures in the young. |
Conflict of interest statement
The authors have no conflicts of interest to declare.