Very often we encounter a diagnostic problem in patients with symptoms and signs of cardiac ischaemia, but without overt disease in the epicardial coronary arteries. We used to disregard the findings and stop the diagnostic approach right there. Patients were reassured and sent home on the supposition that the symptoms were not related to the heart. In 2018 this is no longer acceptable for the patients (often female) and the treating physicians. But how are we going to illustrate a disease that is difficult to prove, comes with variable symptoms and is hard to treat in a customised way?
As indicated in the recently published position statement on percutaneous and structural interventions in women by the EAPCI Women Committee in EuroIntervention, one of the knowledge gaps concerns coronary microvascular disease, especially in women1.
The concept of signs and symptoms in the absence of obstructive coronary artery disease (non-obstructive coronary artery disease [NOCAD]) has been well recognised for many years. In patients with stable angina undergoing coronary angiography, about 40% have NOCAD and the majority of these patients are women (70%). We all know that coronary spasm is a disease entity of the epicardial vessels. However, spasm can also be based on overreactive microvascular arteries. Keep in mind that the coronary microcirculation takes care of 90% of the blood supply of the heart. This implies that we have focused on only 10% for the past decades! Yet few centres around the globe undertake the effort of collecting proof of spasm through an invasive provocation test. One of the issues is that the test could be harmful for the patient. However, the group of Prof. Sechtem in Stuttgart and others have demonstrated it to be a safe procedure and easy to perform in daily practice. Also, the Coronary Vasomotion Disorders International Study group (COVADIS), led by Prof. Bairey Merz, urges the need for the implementation of standardised diagnostic criteria for microvascular dysfunction2. Limited access to functional tests is remarkable as we all know that definite proof for a correct diagnosis is mandatory. If we have a diagnosis we can start thinking about mechanisms, customised treatment and prognosis. Therefore, every interventional cardiologist should be trained in the functional approach, especially in NOCAD patients.
Also in patients with MINOCA (myocardial infarction with non-obstructive coronary artery disease) further investigation should be carried out in order to find the proper diagnosis as MINOCA is a working hypothesis, and not a diagnosis in itself3. In addition, the increased susceptibility to arterial dissection especially in younger females (44-53 yrs) is well known. At times dissections can have a complete or partial occlusive presentation leading to an acute coronary syndrome. Treatment should be conservative, although sometimes a percutaneous coronary intervention is needed. Here too we know little of the mechanisms involved and therefore hardly anything is known about which medical treatment is best in these patients with again a strong predominance in women (>90%). In some cases, genetics would appear to play a dominant role. Hormonal changes around pregnancy and the menopause have been recognised as possibly contributing. In daily practice in most cases the cause remains to be determined.
In patients presenting with an ST-elevation myocardial infarction, but with NOCAD, Takotsubo syndrome should be looked for. In >70% of cases, the disease is preceded by an emotional trigger. It also has a strong predominance in women (90%); however, it occurs at an older (post-menopausal) age (60% >65 yrs).
If spasm, dissection and cardiomyopathy have been ruled out, coronary microvascular dysfunction defined as endothelium-independent decreased ability for dilatation of the microvascular coronary arteries remains an important condition. It has been shown that microvascular dysfunction has an effect on the long-term prognosis and quality of life and leads to high healthcare costs including incomplete coronary functional assessment with all the accompanying risks of a procedure.
How can we diagnose what we cannot see? We will have to rely on functional measurements and will have to expand our investigative repertoire. For instance, the coronary flow reserve (CFR) could be impaired in those patients, which helps to identify a subset of individuals. CFR can be measured by positron emission tomography by absolute flow; however, only a few hospitals have access to this expensive non-invasive imaging. Several other non-invasive techniques are suggested (cardiac magnetic resonance and Doppler ultrasound of the LAD); however, these techniques do not have a broad dissemination and often do not demonstrate an abnormality. Alternatively, CFR can be measured invasively during angiography. However, the technique is not performed everywhere, as it can be difficult to obtain good signals using the Doppler wire; also, this procedure is not completely free of risk. Of course, this can be overcome by using the thermodilution wire; however, this technique also has its drawbacks and is not used in a daily setting.
Even more important is the lack of knowledge concerning the diagnosis of those NOCAD patients with symptoms, but no (epicardial or microvascular) spasm and a normal CFR (20-50%). The CFR is currently determined to assess coronary microvascular dysfunction, but this technique does not detect all types of coronary microvascular dysfunction because it cannot evaluate the myocardial blood volume in a proper way.
Again, the coronary microcirculation determines about 90% of the blood supply of the heart. At rest, about 50% of the microcirculation contains blood, indicating that the volume can be regulated for instance by a higher level of myocardial O2 consumption or by hyperinsulinaemia which occurs by recruitment of the capillary vessels.
Also, insulin has been found to have important vascular effects in skeletal and cardiac muscle. However, research on cardiac muscle has only been performed in animals and healthy subjects. Other studies have shown that hyperinsulinaemia as a result of insulin resistance seems to be an independent predictor of ischaemic heart disease and that metformin, the standard pharmacological treatment for insulin resistance, reduces ischaemia in women with NOCAD. Thus, it is important to know whether the effects of insulin on cardiac muscle are relevant in NOCAD patients and what the mechanism behind this is. We all know that NOCAD patients have several risk factors including diabetes and also hypertension which can affect the function of the microvasculature.
Myocardial blood volume can be measured by myocardial contrast echocardiography. Echocardiography is, however, time-consuming and not all patients have good visualisation windows. Furthermore, images can be difficult to interpret. Therefore, we need to perform research and especially clinical studies using non-invasive imaging techniques in combination with invasive procedures to move the field forward and to understand better the pathophysiology of microvascular (dys)function. In our centre, VU University Medical Center in Amsterdam, we will perform a proof-of-concept trial, the MICORDIS study (Reduced Microvascular Blood Volume as a Driver of Coronary Microvascular Disease in Patients with Non-Obstructive Coronary Artery Disease), as a response to the urgent need for a better understanding of the pathophysiology and effective prevention, diagnosis, and management of NOCAD and its associated sex- and gender-specific features. We will determine the value of measuring myocardial blood volume in relation to microvascular dysfunction. Furthermore, we will test a cardiac magnetic resonance imaging protocol (T1) as a new imaging tool in addition to contrast echocardiography for measurement of myocardial blood volume in clinical practice.
In conclusion, what will be crucial for the next five years is to work on increasing the treating physicians’ awareness of microvascular disease in and raising interest in the small vessels of which we know too little. The work of the (interventional) cardiologist does not end when atherosclerosis has been excluded as the cause of symptoms and signs of ischaemia. Also, it is too early to start treating patients for potential spasm without demonstrating the occurrence and understanding the contributing factors. Lack of epicardial abnormalities on coronary angiography should be the starting point of a diagnostic work-up using invasive measurements. Additional European funding is essential to improve our diagnostic algorithm (Figure 1) and to register sufficient patient numbers. Finally, we will need more mechanistic insight to be able to develop new therapies to make the promise of customised treatment a reality, especially in women.
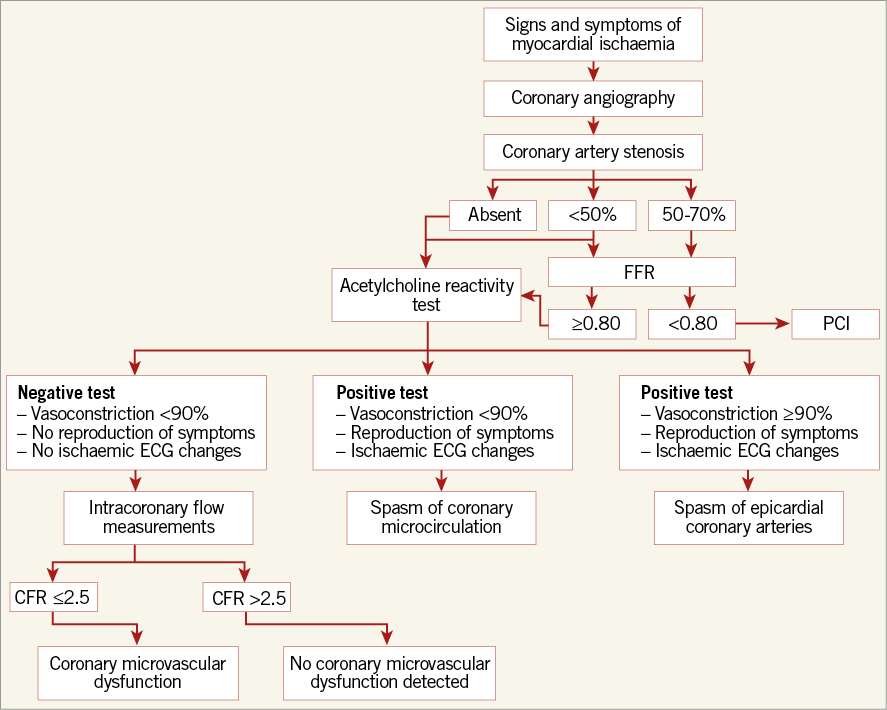
Figure 1. Diagnostic algorithm for NOCAD patients undergoing coronary angiography.
Conflict of interest statement
The author has no conflicts of interest to declare.