A 58-year-old man with treated hypercholesterolaemia and a smoking habit was admitted to hospital with stable angina. In April 2006, the patient was treated with an ABSORB bioresorbable everolimus-eluting vascular scaffold system (Abbott Laboratories, Abbott Park, IL, USA) (ABSORB BVS - 3.0×12 mm) in the left circumflex in the context of the ABSORB Cohort A trial. Per protocol, at six-month follow-up and at two years, the patient underwent intravascular imaging. In March 2011, the patient presented with stable angina and in the coronary angiography three intermediate lesions were found and evaluated with fractional flow reserve (FFR); one in the obtuse marginal FFR was 0.79 for which the lesion was treated with a XIENCE V stent 2.75×18 mm (Abbott Laboratories).
On IVUS, from baseline to six months, the mean vessel area decreased and the mean plaque area remained unchanged, resulting in a slight decrease in mean lumen area. In contrast, from six months to two years, there was a clear shrinkage of the plaque size accompanied by vessel size reduction (and preservation of the lumen). At this time point, which coincided with the near total resorption of the BVS, an anti-atherosclerotic effect was observed (i.e., regression of plaque size). At five years, within the previously treated segment, in its distal part, there was an increase in vessel size, in response to an increase in plaque size, but also with lumen enlargement; towards the mid and proximal part of the segment, remodelling was not compensatory and a clear reduction in lumen size could be observed (Figure 1). The serial angiographic changes, as well as the optical coherence tomography (OCT) results, can be found online.
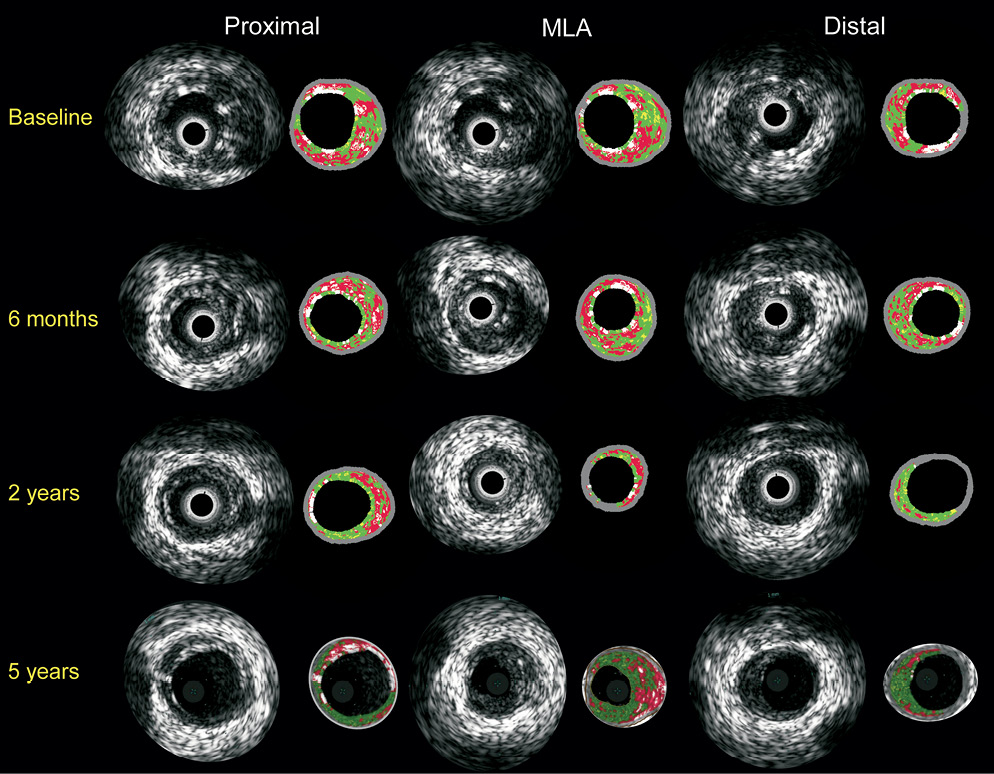
Figure 1. Intravascular ultrasound greyscale and virtual histology. This figure includes corresponding images of greyscale and virtual histology IVUS at three different locations within the scaffolded segment (proximal –first and distal– last frames of the BVS and MLA; of note, same anatomical references can be seen in the vicinity of the coronary vessel wall) at four different time points. At baseline and six months, struts can be recognised as hyperchogenic and white structures in greyscale and virtual histology respectively along the circumference of the lumen. The struts dramatically decrease at two years and are no longer present at five years. The serial changes over time in the vessel wall size, qualitatively, can be appreciated, from large to small, while in contrast the lumen area shows an increase in size over time. This can be quantitatively confirmed in the following: Online Figure 3.
Conflict of interest statement
The authors have no conflicts of interest to declare.
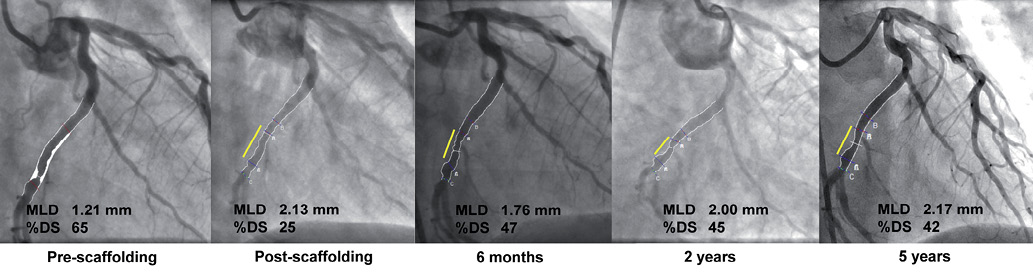
Figure 1. Serial quantitative coronary angiography. Pre-scaffolding (panel A), post-scaffolding (panel B), 6 months (panel C), 2 years (panel D) and 5 years (panel E) coronary angiograms showing the original lesion and the QCA at different time points. Yellow line indicates the location of the BVS. Please note the side branch coming off from the mid part of the scaffolded segment which can serve as an anatomical reference for the beginning of the original lesion. Minimum lumen diameter (MLD) and diameter stenosis (DS) represent the average of multiple views and not solely the depicted view.
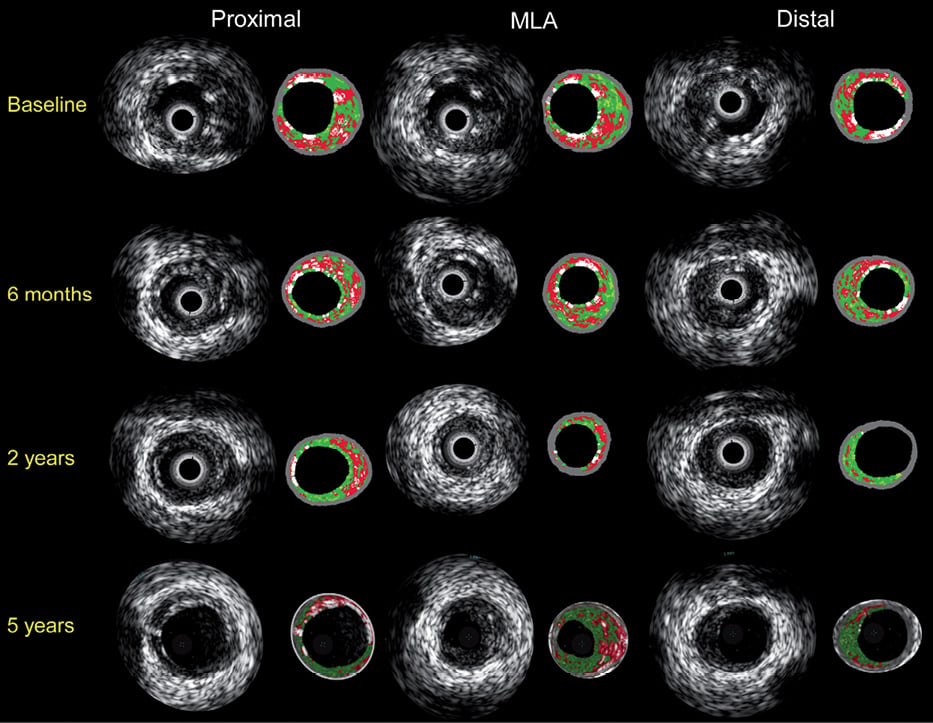
Figure 2. Intravascular ultrasound greyscale and virtual histology. This figure includes corresponding images of greyscale and virtual histology IVUS at three different locations within the scaffolded segment (proximal –first and distal – last frames of the BVS and MLA; of note, same anatomical references can be seen in the vicinity of the coronary vessel wall) at four different time points. At baseline and at six months, struts can be recognised as hyperchogenic and white structures in greyscale and virtual histology respectively along the circumference of the lumen. The struts dramatically decrease at two years and are no longer present at five years. The serial changes over time in the vessel wall size, qualitatively, can be appreciated, from large to small, while in contrast the lumen area shows an increase in size over time. This can be quantitatively confirmed in the following figure.
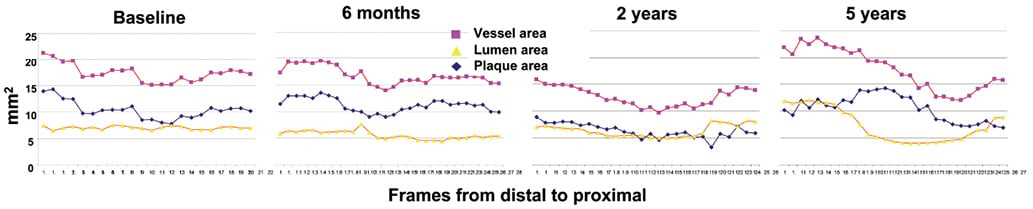
Figure 3. Serial quantitative intravascular ultrasound (IVUS). These graphs show the number of IVUS cross sections within the scaffolded segment (x axis) and the areas (mm2) in the y axis at four different time points, from left to right: baseline, 6 months, 2 and 5 years. The lines represent the vessel (pink), plaque (blue) and lumen (yellow) areas. From baseline to six months, vessel and plaque size remain unchanged and only a slight decrease in lumen size is observed. In contrast, at two years, there is a clear shrinkage of the plaque size at the expense of vessel size reduction and lumen enlargement. At this time point, which coincides with the nearly complete resorption of the ABSORB, an anti-atherosclerotic effect is observed (i.e., shrinkage of plaque). At five years, especially in the distal part, there is an important increase in vessel size (positive remodeling), in response to an increase in plaque size, but also with lumen enlargement; towards the mid and proximal part of the segment remodeling is not compensatory and a clear reduction in lumen size can be observed.
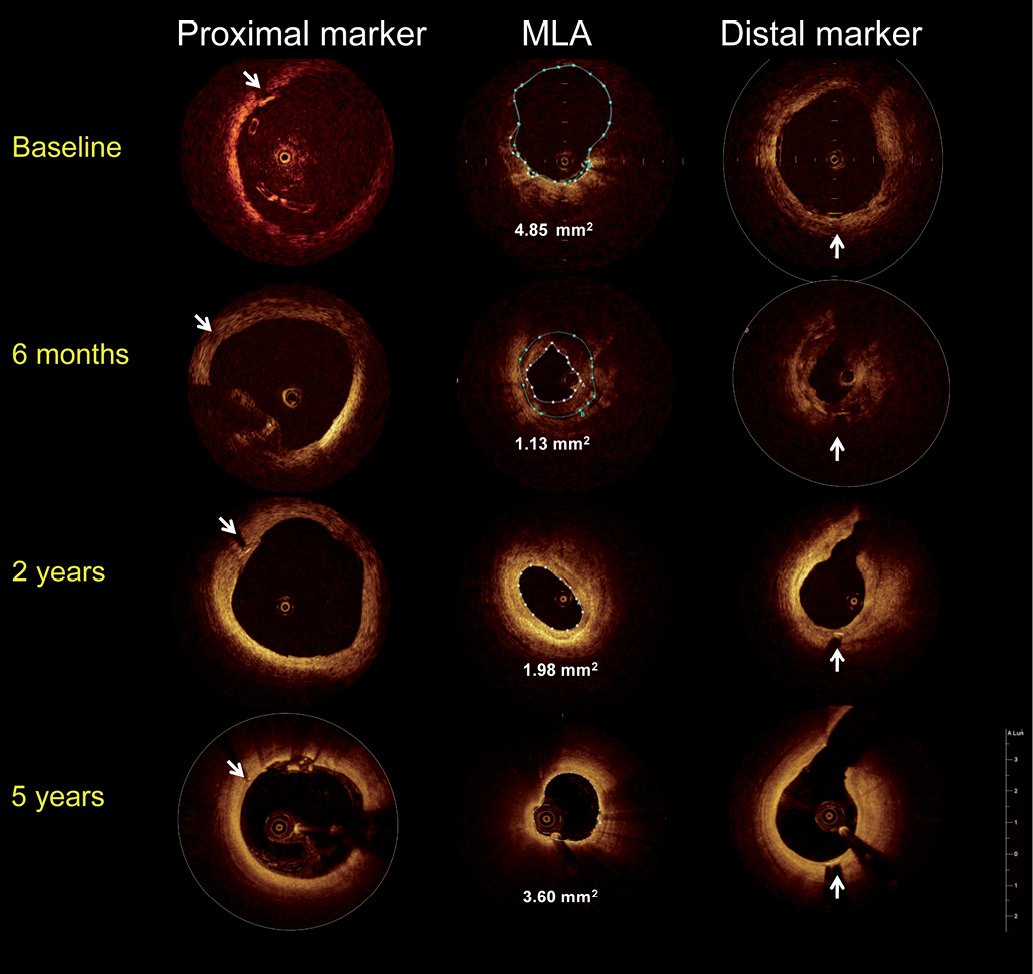
Figure 4. Serial changes in optical coherence tomography (OCT). This figure includes corresponding images of OCT at three different locations within the scaffolded segment (proximal marker and distal marker frames of the ABSORB and minimum lumen area (MLA) at our different time points. White arrows point at the metallic markers. At baseline and at 6 months, struts can be recognised as square boxes along the circumference of the lumen. At the proximal marker frames a few malapposed struts can be seen that are eventually integrated into the vessel wall as they become resorbed. At the MLA frames, a white line represents the lumen area and the blue area represents the scaffold area. This latter is only discernable at baseline and at six months. Minimum lumen area shows an important decrease at six months with an enlargement thereafter.

