Introduction
Chronic total occlusion (CTO) represents the most challenging setting for percutaneous coronary intervention (PCI). Although transfemoral (TF) access is still the preferred one, procedural success with the transradial (TR) approach can potentially reach comparable rates1. The small size of the radial artery remains a limitation for the use of >6 Fr guiding catheters. Aminian et al have reported their experience with the 7 Fr Glidesheath Slender® (Terumo, Tokyo, Japan) in complex TR-PCI, showing a high procedural success rate and a low rate of vascular complications2. Left distal transradial access (ldTRA) has been described for PCI3; however, no data are available on using a 7 Fr sheath. We evaluated the feasibility and safety of the ldTRA using a 7 Fr Glidesheath Slender in a consecutive series of CTO PCIs.
Methods
We included 41 consecutive CTO PCIs performed by CTO-dedicated operators having a personal ldTRA experience of ≥50 procedures. The ldTRA was evaluated as a standard arterial access site to advance a 7 Fr Glidesheath Slender, while the second vascular access was decided on a case-by-case basis. The presence of left distal radial artery (ldRA) pulse in the radial fossa was detected by manual palpation (Figure 1A). Doppler ultrasound examination was performed in case of absence or weakness of the pulse. The ldRA was punctured (Figure 1B) with a 21 gauge open needle at an angle of 30-45 degrees and from lateral to medial3. In case of difficulty in advancing the wire, we administered a spasmolytic cocktail containing 200 mcg of nitroglycerine and 5 mg of verapamil, then angiography was carried out to assess the occurrence of radial artery loops or tortuous courses. After successful wire advancement (Figure 1C), a 7 Fr Glidesheath Slender was inserted (Figure 1D), then the arm was moved across the patient’s body with the left palm on the right groin (Figure 1E). After completion of the procedure, patent haemostasis was achieved in all patients using a radial band (Figure 2A), which was left in situ for two or a maximum of three hours, as proposed by Kiemeneij3. Before discharge, the presence of a radial pulse at the distal forearm and in the anatomical snuffbox was checked by manual palpation and Doppler ultrasound (Figure 2B). The primary endpoint was procedural success which was defined as achievement of technical success using the initially selected ldTRA with no in-hospital major adverse cardiac events (MACE). Secondary endpoints were the occurrence of major bleeding, vascular access-site complications, spasm, major sheath kinking, and post-procedural left distal radial artery occlusion (ldRAO), assessed clinically and by Doppler ultrasound examination the day after the procedure and at one-month follow-up.
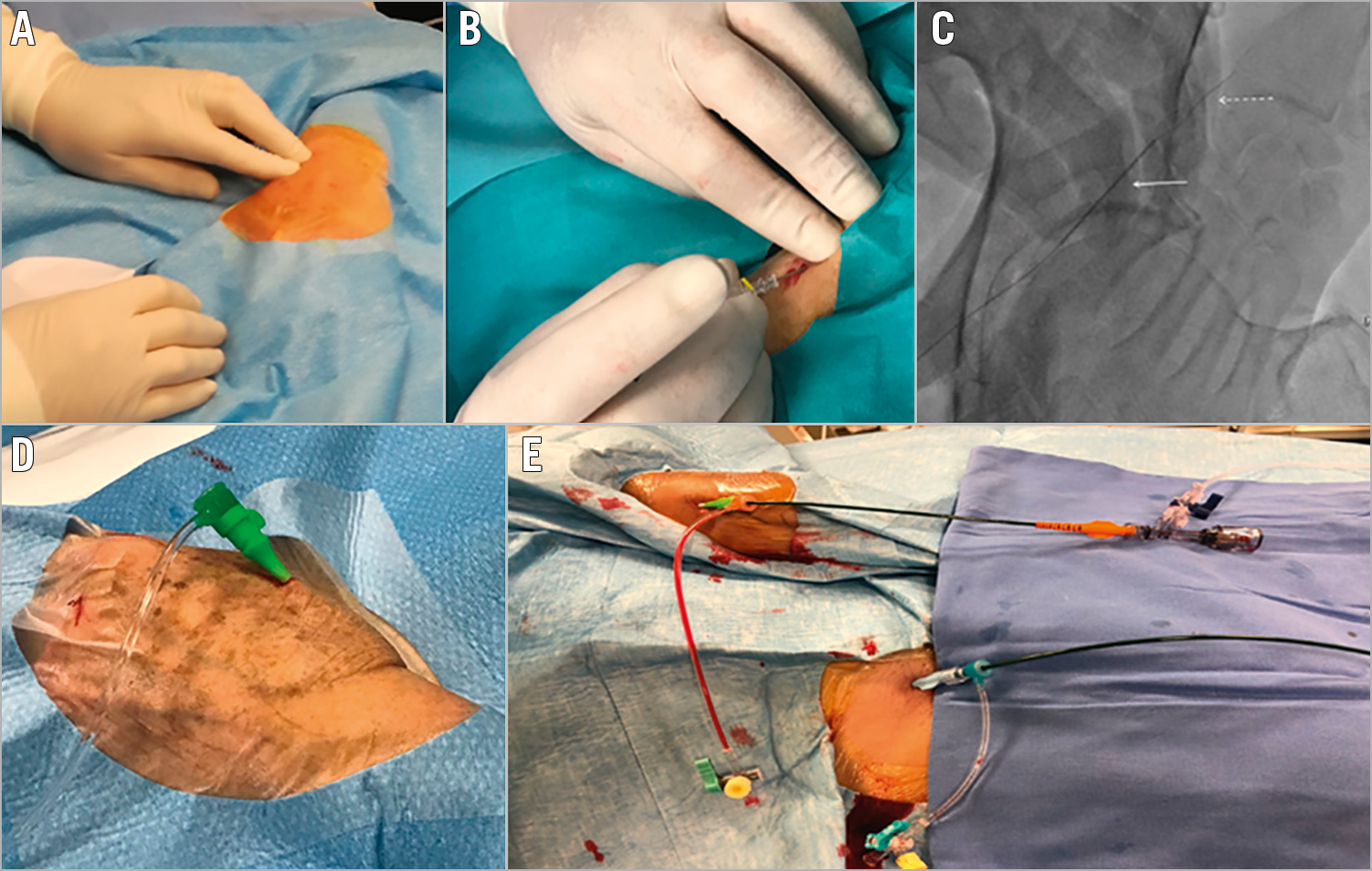
Figure 1. Procedural setting of left distal radial approach. A) Manual palpation of ldRA. B) Puncture of ldRA. C) Wire advancement. D) Insertion of 7 Fr Glidesheath Slender. E) Patient’s left palm on the right groin.
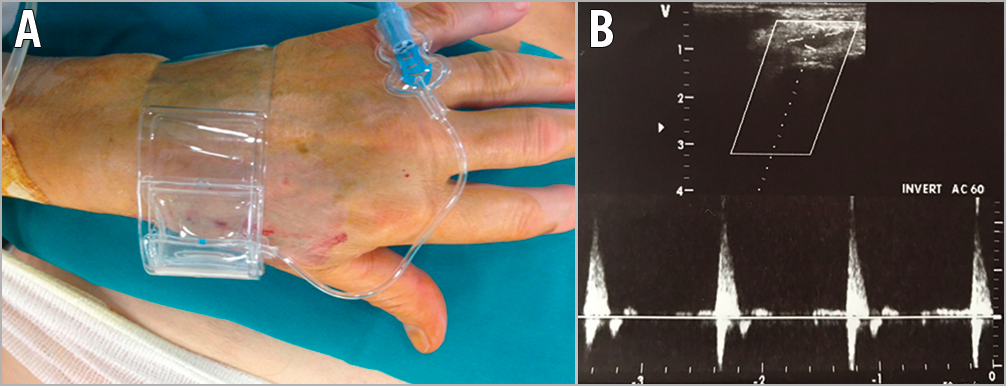
Figure 2. Post-procedural access management. A) Haemostasis with radial band. B) Post-procedural ultrasound examination of ldRA.
Results
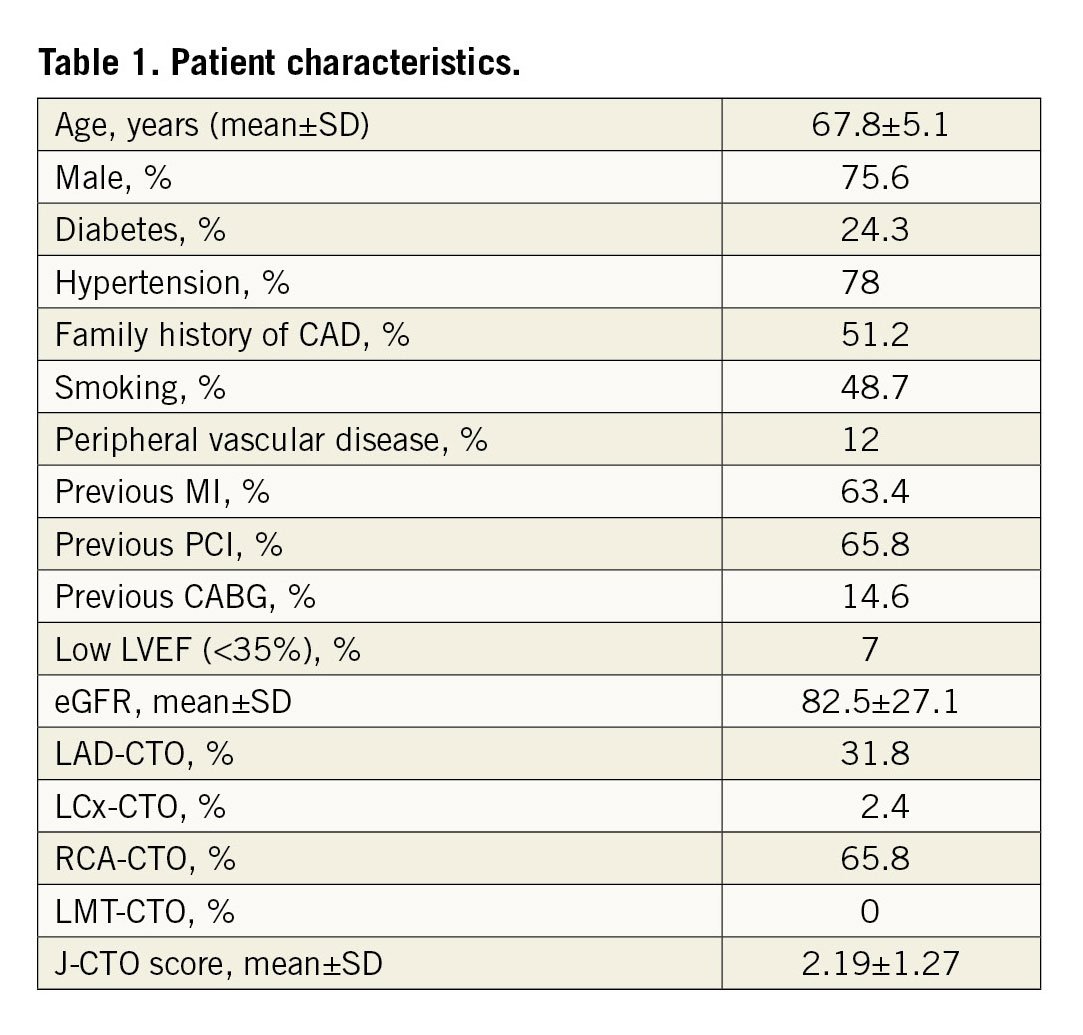
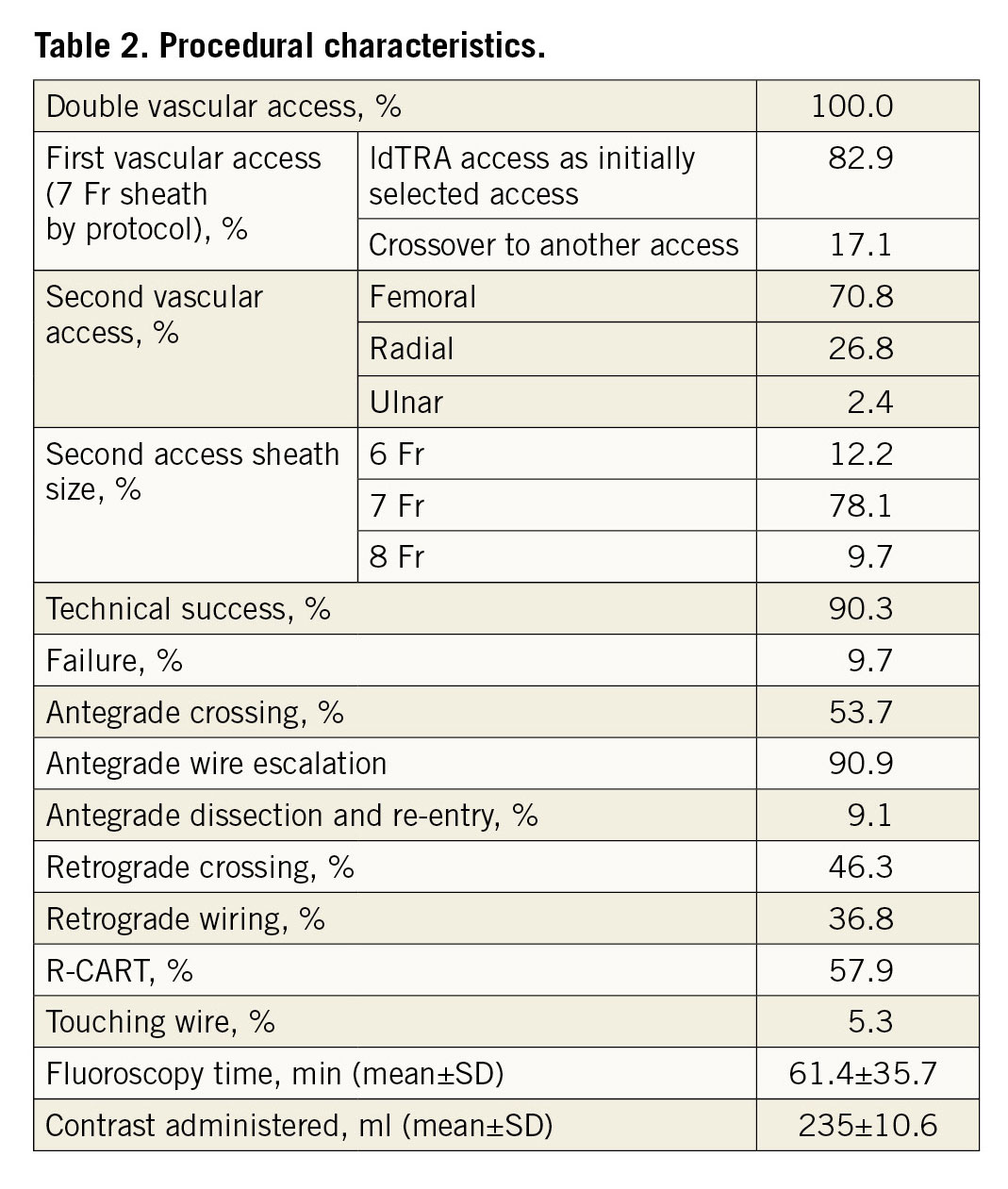
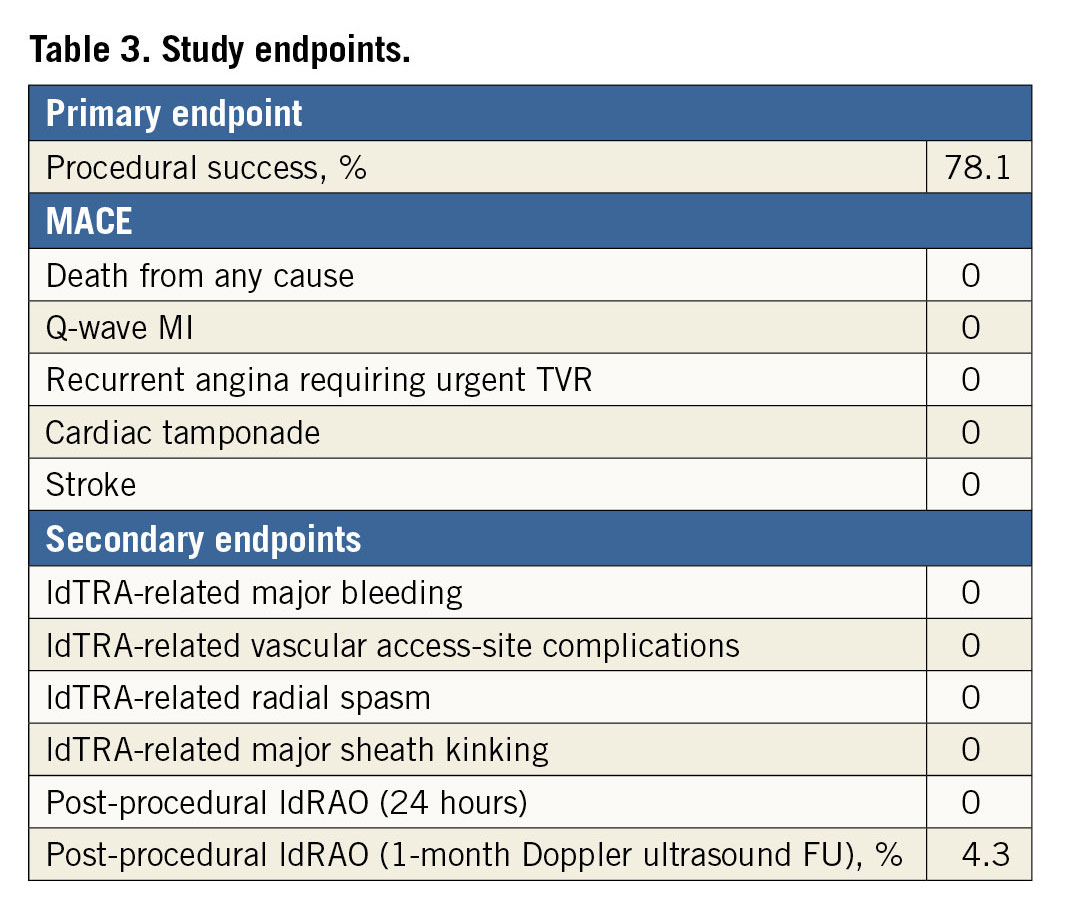
A total of 41 CTO PCIs were included in our analysis. Patient characteristics are summarised in Table 1; procedural characteristics are summarised in Table 2. A successful vascular access through the ldTRA using a 7 Fr Glidesheath Slender was obtained in 34 patients (82.9%), while seven (17.5%) had a failed attempt, necessitating a crossover to another access. The reasons were weak or absent pulse in the anatomical snuffbox (3 patients) or excessive vessel tortuosity which did not allow the wire advancement towards the forearm part of the radial artery (4 patients). Study endpoints are listed in Table 3. Technical success was achieved in 90.3% of patients (37/41). There were four procedural failures not related to the ldTRA itself. Procedural success was achieved in 78.1% of patients. In-hospital MACE, ldTRA-related vascular access-site complications, major sheath kinking and major bleeding events were not registered in the study population. Likewise, no post-procedural ldRAOs were detected by clinical assessment and Doppler ultrasound examination, and no radial artery occlusions at the site of the forearm were encountered. Doppler ultrasound imaging of the ldRA at one month was available in 23 out of 34 (67.6%) patients, with only one case (4.3%) of ldRAO in a woman.
Discussion
Our data demonstrated that ldTRA using a 7 Fr Glidesheath Slender for CTO PCIs is feasible and associated with a high procedural success rate and low vascular access-site complication rates. No significant ldRA spasm was observed, probably due to the smaller diameter in combination with the hydrophilic coating of the Glidesheath Slender. The low rate of ldRAO we observed is consistent with the available published data; however, use of Doppler ultrasound to evaluate the ldRA diameter before inserting a 7 Fr sheath could prevent ldRAO in case of considerable mismatch between ldRA inner diameter and sheath outer diameter. The advantages of this access during CTO PCI are several: first of all, the arm position during the intervention is more comfortable both for the patient and for the operator. Additional advantages are represented by low haemorrhagic risk, short haemostasis time and low rate of ldRAO. Finally, the operator can work at a safe distance from the radiation source.
Limitations
First, only 41 CTO PCI procedures were evaluated. Second, all procedures were performed by highly experienced CTO operators, with an ldTRA experience level of >50 procedures per operator; therefore, the observed results may not be widely applicable. Third, most patients included were men, although women are more likely to have smaller ldRAs. Fourth, one-month assessment by Doppler ultrasound was performed in a relatively small number of patients.
Conclusion
Our experience demonstrates that ldTRA in the setting of CTO PCI using a 7 Fr Glidesheath Slender is feasible and safe, with a high procedural success rate and low access-site complication rates.
|
Impact on daily practice Including this technique in the armamentarium of CTO operators may be helpful when bifemoral access is not feasible or as an alternative entry site when biradial access is preferred. |
Conflict of interest statement
R. Garbo reports receiving consulting/speaker honoraria from Terumo, Volcano, IMDS, and Alvimedica. J. Oreglia reports receiving consulting/speaker honoraria from Terumo, Abbott Vascular, Volcano, IMDS, and Boston Scientific. G.L. Gasparini reports receiving consulting/speaker honoraria from Terumo, Volcano, Abbott, IMDS, and Cardinal Health. A. Gagnor reports receiving consulting/speaker honoraria from Terumo, Volcano, Abbott, and IMDS. P. Mazzarotto reports receiving consulting/speaker honoraria from Terumo.