Diabetes is recognised as one of the most important global health threats today. In 2011, an estimated 52 million Europeans were diabetic, a figure that is steadily increasing. As many of them are asymptomatic, only half are diagnosed. The incidence rises with age and the lifetime risk of developing diabetes in Europe is 30-40%. The great majority, over 90% of cases, have type 2 diabetes caused by a combination of insulin resistance and failing beta cell function1. A glycaemic continuum is recognised, whereby progressively abnormal glucometabolic regulation is associated with decreased insulin sensitivity, hyperinsulinaemia and rising glucose levels until thresholds for a diagnosis of diabetes are reached. The early stages of the continuum are often associated with other vascular risk factors, and macrovascular disease is frequently manifest before or early after a diagnosis of diabetes is made, unlike microvascular complications which are more closely linked to chronic severe hyperglycaemia. Cardiovascular disease develops in over 60% of patients with diabetes and is the main cause of death.
A typical diabetic coronary phenotype is readily identified, characterised by small diffusely diseased vessels, a pattern of sequential stenoses and distal tapering, as a consequence of a large atheroma burden as well as negative remodelling. Less often are interventionists aware of the glycaemic status of a patient, particularly if a diabetic pattern of disease is absent and there is no history of diabetes. There are several reasons why it matters to establish a patient’s glycaemic status which impact on therapeutic decisions relating to drug and device use and choice of revascularisation approach. It is well recognised that diabetic patients presenting with an acute coronary syndrome and/or undergoing intervention, despite contemporary best practice, have a worse prognosis2. The BARI diabetic substudy published in 19973 generated a decade-and-a-half controversy regarding the optimal revascularisation approach to patients with diabetes and multivessel disease. This continued despite multiple subset analyses of randomised trials and meta-analyses until a large randomised controlled trial confined to patients with diabetes confirmed that patients with predominantly three-vessel disease requiring multivessel intervention had a better outcome following bypass surgery4. The SYNTAX trial confirmed that patients with the most diffuse and complex disease, typical of that found in diabetics, and characterised by a high SYNTAX score, were surgical candidates5. That anatomical features alone do not account for this treatment effect is suggested by the benefit of surgery over PCI extending to diabetic patients with multivessel disease but with a low SYNTAX score4. Apart from the mode of revascularisation, other aspects of the management of patients with diabetes with ACS and/or undergoing intervention are affected by diabetic status. A study of a large pre-specified subgroup of patients with diabetes in the TRITON-TIMI 38 trial suggested a particular advantage of prasugrel over clopidogrel in this group, most marked in those requiring insulin. The bleeding risk was higher in patients with diabetes but, in contrast to the non-diabetic population, there was no difference in bleeding risk for those receiving prasugrel compared to clopidogrel amongst diabetics6. Whereas heightened platelet reactivity and an increased risk of thrombosis are recognised in diabetics, so too is a higher risk of bleeding7. Drug-eluting stents (DES), particularly third-generation DES, outperform bare metal stents in diabetic patients and receive a strong recommendation in current guidelines1.
In this issue of EuroIntervention, two studies are reported which focus on different aspects of the impact of diabetes in patients undergoing PCI. The first by Ndrepepa et al8 is a retrospective observational study assessing the impact of early peri-interventional bleeding in a cohort of 4,329 patients with known diabetes. The Bleeding Academic Research Consortium (BARC) criteria9 were applied retrospectively to data sourced from the combined database of 14,180 patients recruited in seven ISAR trials, one third treated for acute myocardial infarction (AMI). Bleeding occurred in 11% of patients, slightly more non-access-site than access-site related. A considerable proportion, 38%, of bleeds were small and “unactionable” (BARC 1). The principal finding was a higher mortality at one year in diabetic patients who suffer bleeding complications (adjusted hazard ratio 2.04), more pronounced in those with non-access-site bleeding. The odds ratio for stent thrombosis and myocardial infarction was 2.04 and 2.95, respectively, in those with bleeding compared to those without. As previously demonstrated, there appeared to be a positive correlation between the severity of bleeding and the rate of stent thrombosis and myocardial infarction. The study failed to show a difference in the rate of bleeding in those treated with or without insulin, although a more detailed correlation of severity of diabetes and bleeding risk was not undertaken.
The study confirms that bleeding is dangerous in patients with diabetes undergoing percutaneous intervention and provides a figure for how often this occurred in a large cohort of diabetic patients. The finding reinforces the fact that bleeding in all patients undergoing intervention is a powerful negative prognostic indicator10. The study is limited by its retrospective nature, including the retrospective classification of bleeding, and the failure to compare rates of bleeding in diabetics and non-diabetics in the overall seven-study cohort. The universal use of femoral access limits the study’s significance to contemporary practice, at least as it pertains to access-site bleeding rates.
The second report by Hoebers et al11 is a retrospective observational study that compared the long-term outcome following treatment for STEMI in patients with and without diabetes. The diabetic patients were further classified according to whether they received insulin. The study included 4,402 patients treated for STEMI between 1997 and 2007. A relatively small number were diabetic, just 11%, and of these there were 176 insulin-treated and 354 non-insulin-treated diabetic patients. The primary outcome was all-cause five-year mortality. This was highest in the insulin-treated group at 36%, 25% in non-insulin-treated diabetics, and 18% in non-diabetics. Following adjustment for age and gender, insulin-treated diabetic patients had elevated adjusted risk compared to non-diabetics (HR 1.9), but surprisingly this was not found for non-insulin-treated diabetic patients.
That diabetic patients have a worse prognosis is not a novel finding. Insulin-treated diabetics were relatively few in the study and were not characterised beyond preadmission treatment history, although, given the more advanced age of these patients, as pointed out by the authors, it can reasonably be assumed that most were insulin-requiring type 2 diabetics. It is not surprising that more advanced disease and use of insulin were associated with higher risk. The novel finding of the study of a comparable five-year survival in non-insulin-requiring diabetic patients and those without diabetes is counterintuitive and at odds with previous studies which have shown a worse prognosis in patients with undifferentiated type 2 diabetes presenting with ACS2,12. This may represent poor characterisation of diabetic management in previous studies, or might be spurious given the small sample size, but at any rate merits further scrutiny.
Our knowledge of the interaction of diabetes and percutaneous intervention has been hampered by the lack of dedicated studies. Most of the evidence base comprises subgroup analysis of randomised trials in which a variable proportion, typically between 15% and 25%, are diabetic (Figure 1). Whereas the upper figure may come close to representing the prevalence of confirmed diabetes in patients presenting with coronary artery disease, a number of studies highlight the much higher level of glucometabolic abnormality which is found if actively sought13,14. Insofar as they add to our understanding of this important interaction, the studies in this issue of EuroIntervention are welcome. Randomised trials dedicated to patients with diabetes provide the most convincing answers to outstanding questions but are difficult and expensive to conduct and not all questions are suitable for this form of enquiry. The randomised registry trial is being considered as an alternative strategy15. A number of key features for this to work include the prospective collection of standardised predefined data in a comprehensive manner in sequential patients, a worthwhile but challenging undertaking. To enrol patients usefully in prospective observational studies and to improve the management of diabetic patients through risk prediction and avoidance measures, a crucial first step is actively to make the diagnosis. Interventionists should remember to measure glycosylated haemoglobin and fasting blood sugar systematically and to have a low threshold for performing a glucose tolerance test in all patients without a diagnosis of diabetes presenting with coronary artery disease.
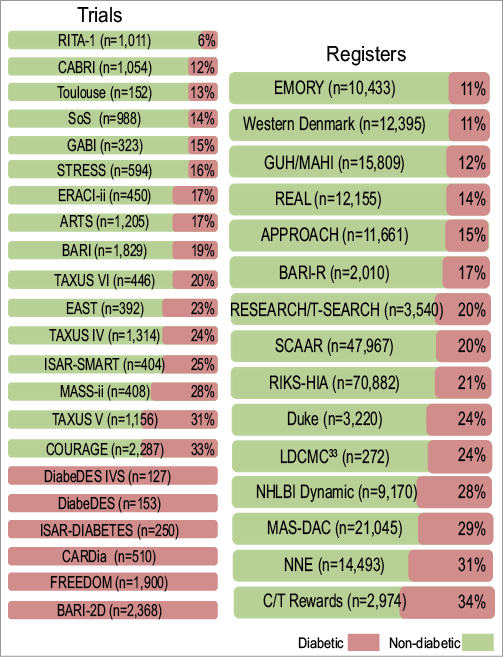
Figure 1. Selection of trials and registers showing proportion of diabetic patients.
Conflict of interest statement
The authors have no conflicts of interest to declare.

