Since the introduction of new potent P2Y12 inhibitors for acute coronary syndrome patients 15 years ago, several strategies have been developed which aim to reduce bleeding complications while maintaining the benefits of intense inhibition of the P2Y12 receptor in the first weeks after percutaneous coronary intervention (PCI). Two main de-escalation options have been tested that can reduce the need for dual antiplatelet therapy (DAPT) after PCI: 1) the discontinuation of DAPT for monotherapy with aspirin or a P2Y12 inhibitor; 2) maintaining DAPT but reducing the intensity of the P2Y12 inhibitor by reducing the dose of the P2Y12 inhibitor (same drug but lower dosage) or by switching from a potent P2Y12 inhibitor (ticagrelor/prasugrel) to clopidogrel, using, if available, an individualised guidance based on platelet function or genetic testing. Considering these strategies all together, an antithrombotic de-escalation strategy leads to a reduced bleeding risk and even to a reduced ischaemic risk. Indeed, a recent meta-analysis including 10,133 patients comparing standard and combined de-escalation strategies reported a 30% and 24% reduction of relative bleeding and ischaemic risks, respectively. Subgroup analyses revealed that, compared to guided de-escalation, unguided de-escalation had a significantly larger impact on bleeding endpoint reduction, although no direct comparison was prespecified1. Nevertheless, the antithrombotic strategies evaluated in all these studies concerned all-comer coronary patients undergoing PCI without consideration of the individual risk of bleeding. However, in clinical practice, individualisation of the antithrombotic regimen is crucial for physicians to choose the best ischaemic/bleeding risk balance.
In this issue of EuroIntervention, Kim et al present a post hoc analysis of the TALOS-AMI study focused on the efficacy and the safety of a de-escalation strategy from ticagrelor to clopidogrel after PCI according to the risk of bleeding2. From the 2,625 patients included in the TALOS-AMI study, 589 patients (22.4%) met the definition of high bleeding risk (HBR). "HBR patients" were identified using modified criteria of the international Academic Research Consortium (ARC) HBR definition3. Among the “modified HBR patients”, the primary endpoint, a composite of cardiovascular death, myocardial infarction, stroke, or minor and major bleeding (Bleeding Academic Research Consortium [BARC] 2, 3 or 5) from 1 to 12 months, occurred less frequently in the de-escalation group (5.7 vs 11.8%, hazard ratio [HR] 0.47, 95% confidence interval [CI]: 0.26-0.84; p=0.011). The incidence of major bleeding (BARC 3 or 5) alone was also lower in the de-escalation group (1.0 vs 4.2%, HR 0.24, 95% CI: 0.07-0.84; p=0.026). On the contrary, in the non-HBR population, no significant reduction of BARC 3 or 5 bleeding was observed with the de-escalation strategy.
The population of patients at high risk of bleeding have previously been poorly represented in clinical studies despite them representing a substantial proportion of patients undergoing PCI (around 40%)34. Following the treatment of more complex PCI associated with a frequently prolonged duration of DAPT and the rising use of potent P2Y12 inhibitors, bleeding risk has received great interest in recent years. The publication of the ARC HBR criteria has been a very important step, leading to a harmonisation of the definitions of patients at high risk of bleeding, which is useful for evaluating antithrombotic strategies more precisely in dedicated trials and, above all, for evaluating patient risk in clinical practice.
The more intuitive strategy to reduce bleeding risk was to shorten the DAPT duration, and numerous randomised trials have investigated this in the specific context of HBR patients. The MASTER DAPT trial was the first to compare an abbreviated duration with a standard duration of DAPT in a large population of HBR patients5. In this study, there was an improved net clinical benefit in the abbreviated DAPT group with a significant reduction in major or clinically relevant non-major bleeding.
Antithrombotic de-escalation strategies comparing standard to abbreviated DAPT duration (1, 3 or 6 months) to reduce bleeding risk in PCI patients are summarised in Figure 1, although de-escalation has been poorly studied in the context of HBR patients. On the basis of the TALOS-AMI substudy2, a new de-escalation strategy could be of interest for HBR patients. However, these results should be interpreted cautiously. Beyond the inadequate power of the study, the use of the modified ARC criteria is an important limitation. Of the 11 major and 6 minor criteria of the ARC definition, 9 major and 2 minor criteria were excluded: specifically, those associated with the most significant risk of bleeding, the occurrence of previous bleeding and long-term anticoagulation therapy. These extensive modifications of the criteria may have reduced the level of bleeding risk of the studied population, which questions the real HBR status of this HBR subpopulation. Indeed, in this study, age ≥75 years (53.0%) and moderate chronic renal failure (48.9%) were the most common major criteria of HBR, both of which are usually considered minor criteria. Likewise, in previous cohorts, moderate/severe anaemia, which was seen in more than 30% of the patients, and long-term oral anticoagulation, observed in 15-20% of the patients34, were excluded in this substudy, preventing any extrapolation on the results.
Further trials are necessary to more completely evaluate this de-escalation strategy in the specific population of HBR patients. Waiting for a head-to-head comparison, the recent European Society of Cardiology Guidelines for the management of acute coronary syndromes proposed an equivalent class of recommendation for de-escalation as an alternative to a DAPT strategy to reduce bleeding (Class IIb, Level of Evidence [LoE] A) and shortened 1-month DAPT (Class IIb, LoE B) for HBR patients6. This is a choice that seems to be linked to the concomitant ischaemic risk. Consequently, as presented in Figure 1, a shortened DAPT duration appears to be beneficial in terms of net clinical benefit and major bleeding in HBR patients with a predominant bleeding risk without an associated significant ischaemic risk. On the other hand, a not-too-short DAPT duration and a strategy based rather on a de-escalation strategy from potent P2Y12 inhibitor to clopidogrel one month after PCI should be preferred in patients with a combined high bleeding/ischaemic risk and particularly in cases of complex coronary artery disease or in patients who experience stent thrombosis or recurrent ischaemic events.
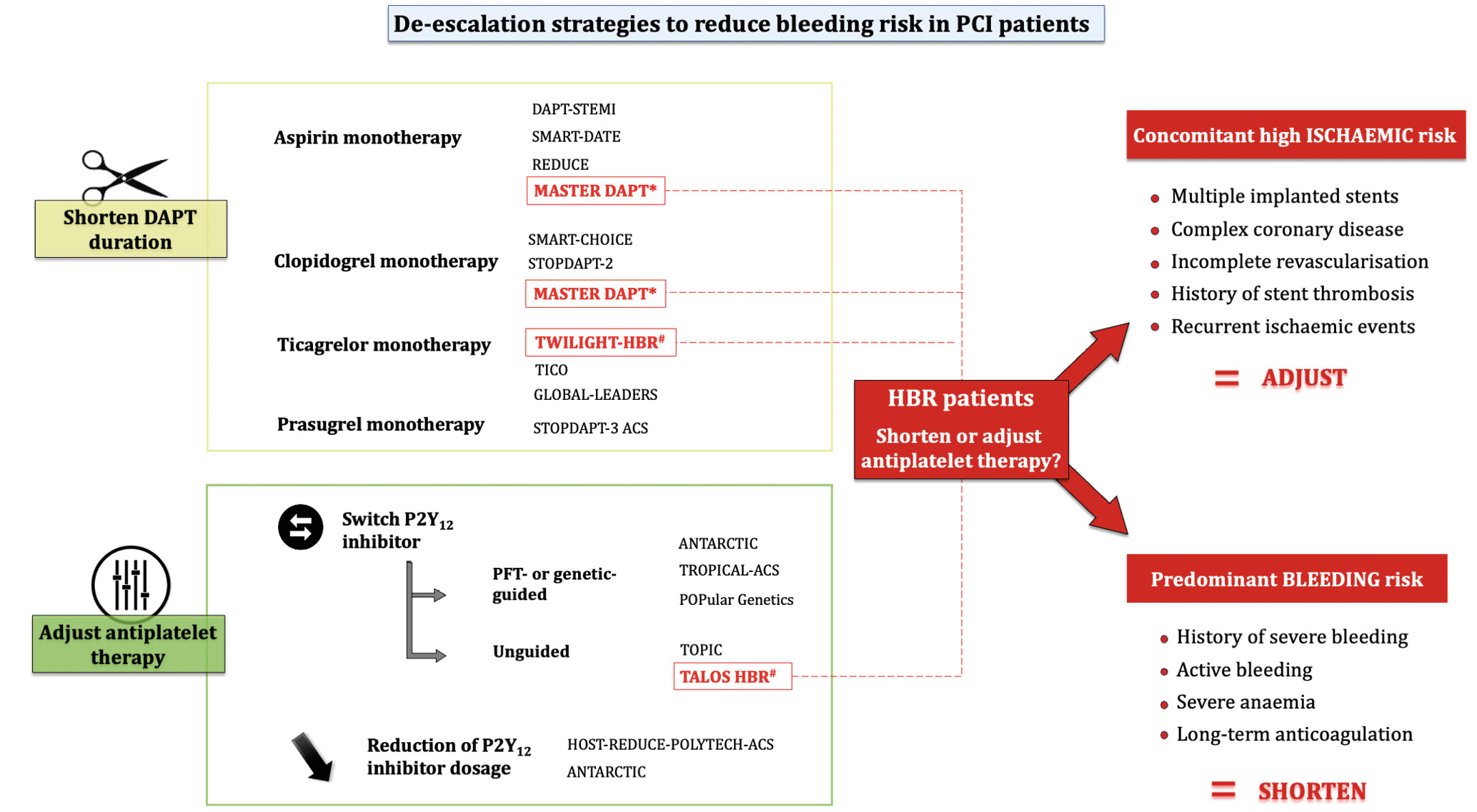
Figure 1. De-escalation strategies to reduce bleeding risk in PCI patients. The studies represented in red are those that specifically included high bleeding risk patients. *In the MASTER DAPT trial, 31% of the patients were treated by aspirin monotherapy and 55.6% by clopidogrel monotherapy after randomisation. #TALOS HBR and TWILIGHT HBR represent the substudies concerning HBR patients from the TALOS and TWILIGHT trials. DAPT: dual antiplatelet therapy; HBR: high bleeding risk; PCI: percutaneous coronary intervention; PFT: platelet function testing
Conflict of interest statement
G. Cayla has received research grants/lecture fees from Abbott, Amgen, AstraZeneca, Bristol-Myers Squibb, Edwards Lifesciences, MicroPort CRM, Medtronic, and Pfizer. B. Lattuca has received research grants from Biotronik, Daiichi Sankyo, La Fédération Française de Cardiologie, and the Institute of Cardiometabolism and Nutrition; has received consultant fees from Abbott Vascular, Daiichi Sankyo, and Eli Lilly; and has received lecture fees from Amarin, AstraZeneca, Medtronic, Novartis, Sanofi, and Terumo.

