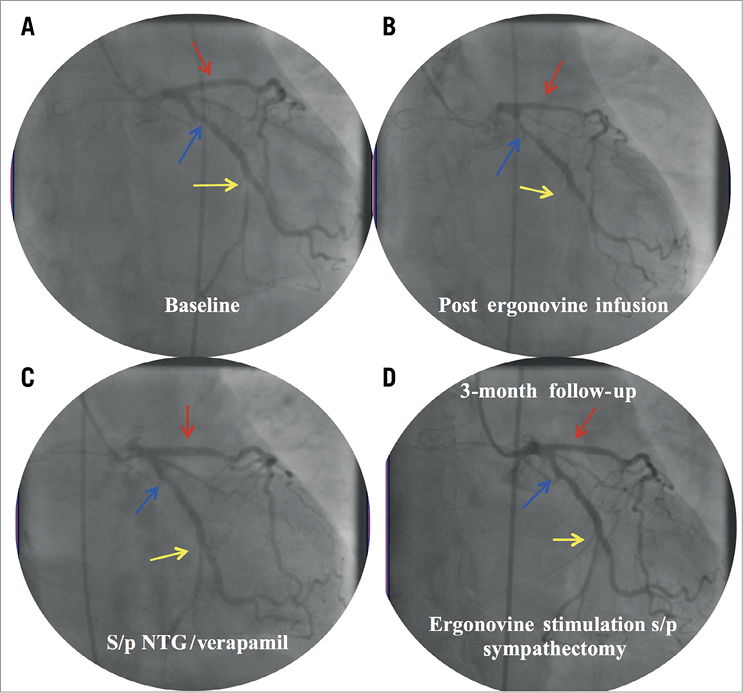
Figure 1. Coronary angiogram demonstrating vasospasm provocation by ergonovine. Red arrow: proximal left anterior descending artery. Blue arrow: proximal left circumflex artery. Yellow arrow: distal left circumflex artery
A 49-year-old female presented to the emergency room with resting chest pain. She carried a history of CAD, initially diagnosed in 2012, as well as dysautonomia and coronary vasospasm. Over the past five years, she has seen several cardiologists and has undergone over 10 catheterisations and four stent implantations. Despite these prior coronary interventions, she continued to be symptomatic with chest pain, at times even at rest, and a recent catheterisation revealed patent intervention sites with only a 60% ostial distal left circumflex artery stenosis. Treatment with beta-blockers and calcium channel blockers was attempted unsuccessfully as they were poorly tolerated and resulted in hypotension associated with her dysautonomia.
The current presentation was similar to prior acute coronary syndromes (ACS), where she had ST-elevation myocardial infarction (STEMI) at rest, which resolved spontaneously as she became chest pain free. The decision was made to perform left heart catheterisation with intracoronary ergonovine infusion, which resulted in 50% stenosis of the proximal left anterior descending artery, 50% stenosis of the proximal left circumflex and total occlusion of the distal left circumflex, associated with ST-elevations on ECG (Figure 1A, Figure 1B, Moving image 1-Moving image 6). Intracoronary nitroglycerine and verapamil resulted in complete reversal of vasospasm (Figure 1C, Moving image 7). Given refractoriness, the decision was made to pursue cardiac sympathectomy, which was accomplished through ablative therapy to the T5 ganglion to the lower half of the stellate ganglion, bilaterally. Postoperatively, the patient had an uncomplicated recovery, besides pain at the surgical site. Upon follow-up, her only complaint was atypical chest pain, probably related to the surgery, without ECGs demonstrating ischaemia. A repeat catheterisation also showed no response to ergonovine (Figure 1D, Moving image 8, Moving image 9).
Coronary vasospastic angina remains a difficult entity to treat1. Bilateral cardiac sympathectomy may be considered in patients with refractory coronary vasospasm2.
Conflict of interest statement
S. Sharma declares financial disclosures for the speaker’s bureau of Abbott, Boston Scientific, and Cardiovascular Systems, Inc. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 2. Pre-ergonovine RAO cranial.
Moving image 3. Pre-ergonovine LAO cranial.
Moving image 4. Ergonovine provocation RAO caudal.
Moving image 5. Ergonovine provocation RAO cranial.
Moving image 6. Ergonovine provocation LAO cranial.
Moving image 7. IC nitro and verapamil RAO caudal.
Moving image 8. 3-month follow-up ergonovine provocation RAO caudal.
Moving image 9. 3-month follow-up ergonovine provocation LAO cranial.
Moving image 1. Pre-ergonovine RAO caudal.